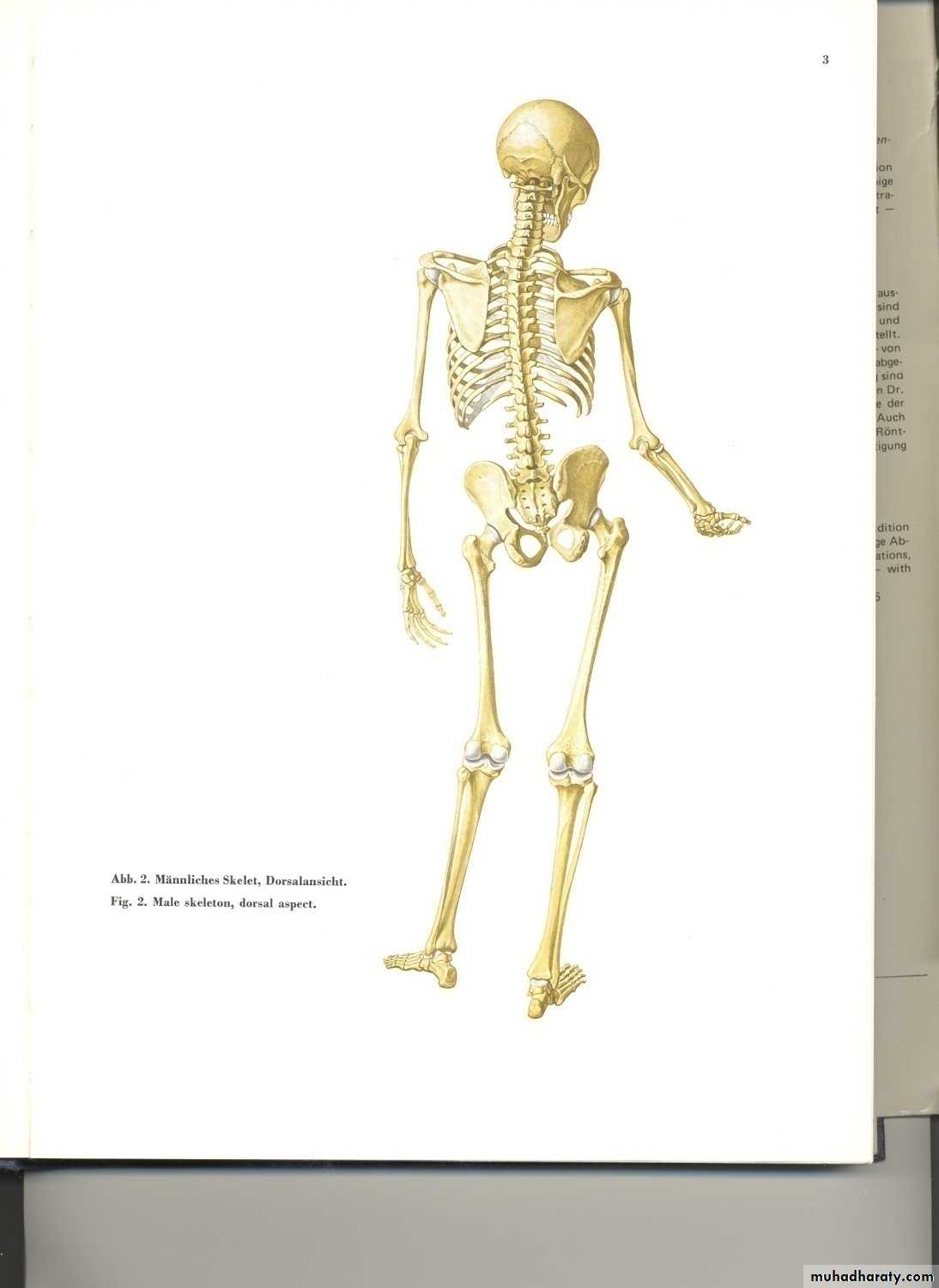
Injuries of the spine
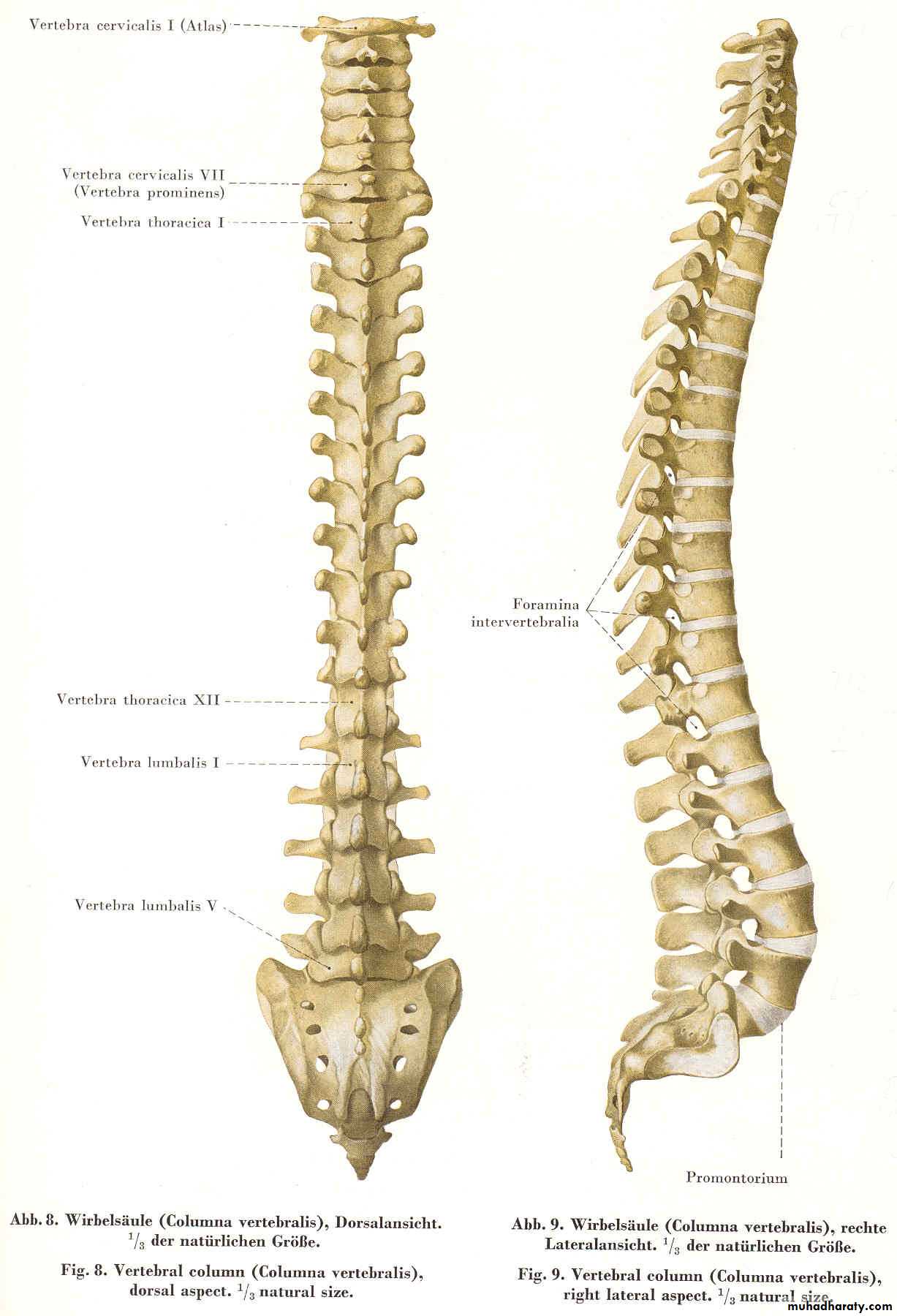
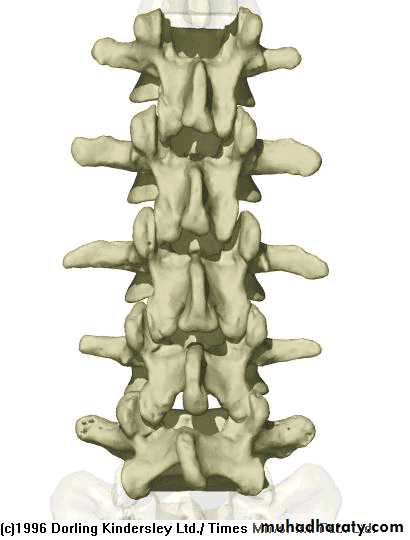
Anatomy: Spinal Column - Orientation• AP View
• (from posterior)left
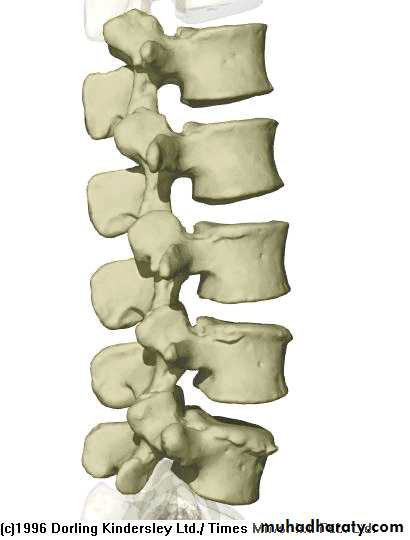
right• Lateral View
cranialcaudal
anterior
(ventral)
posterior
(dorsal)
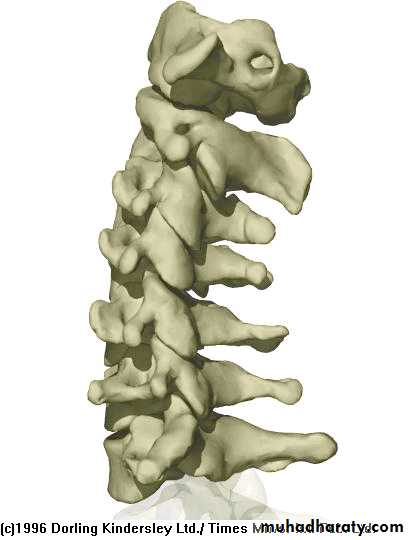
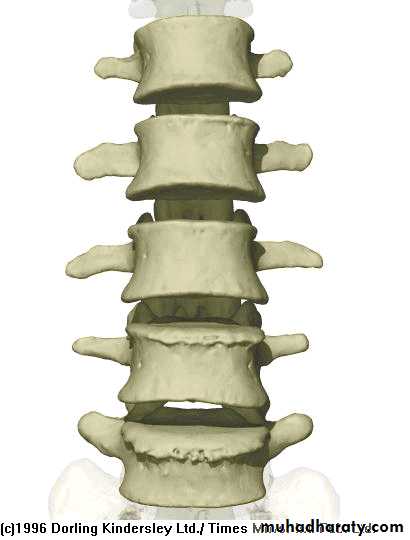
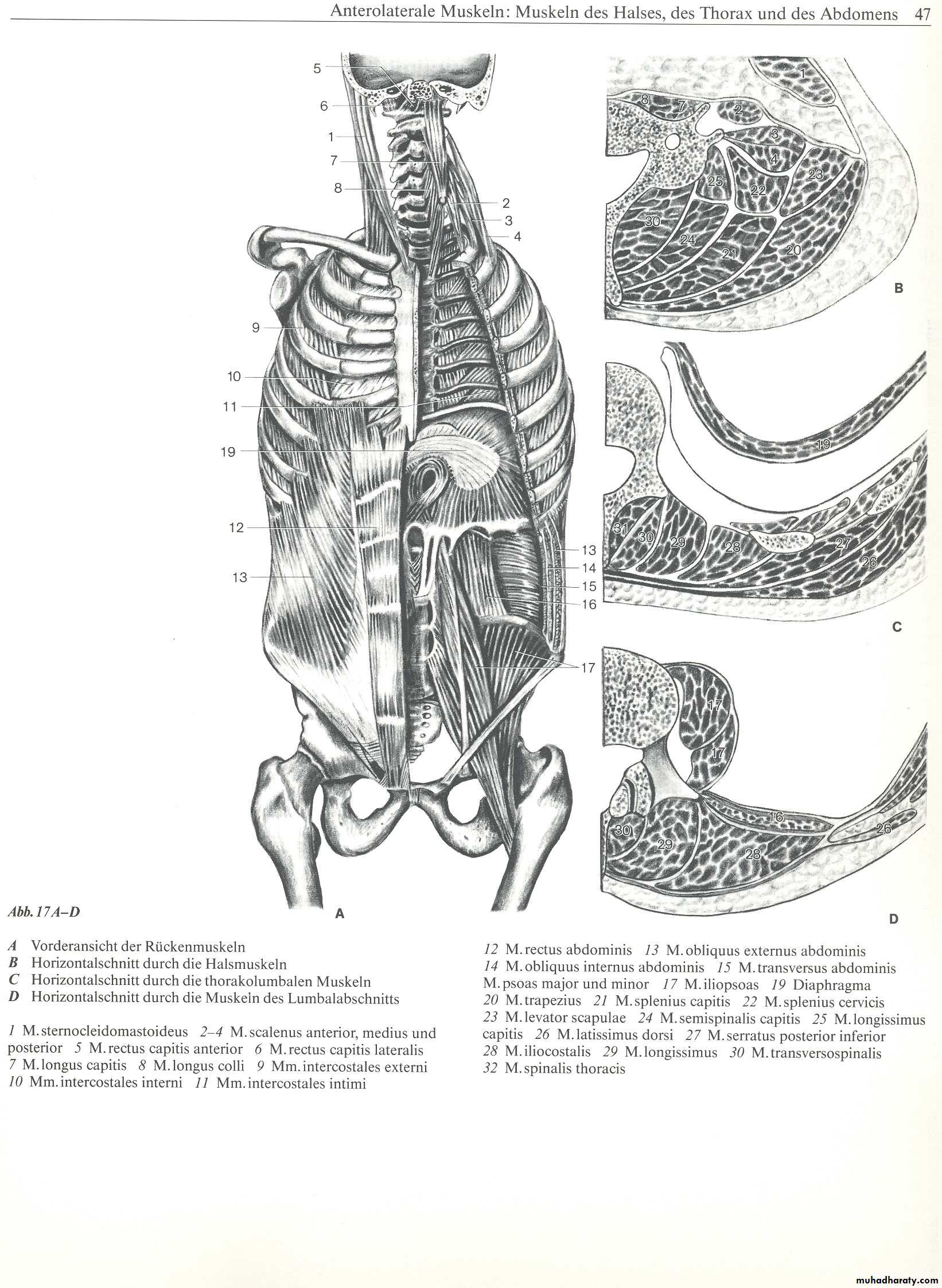
Anatomy: Spinal Column - Vertebrae
• Cervical Vertebrae: 7
• Lumbar Vertebrae: 5• Thoracic Vertebrae: 12
• Sacral Vertebrae: 5
• Coccygeal Vertebrae: 4
• Lordosis
Cervical Spine AnatomyNormal curvature is lordosis
Spinous Processes are BifidA flexible group of vertebrae that support the skull
C1, Atlas
C2, Axis
C3
C4
C5
C6
C7
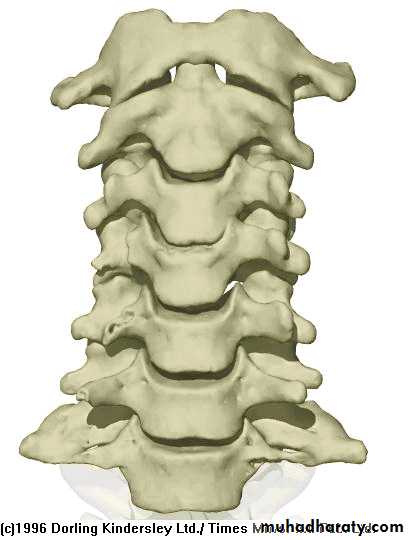
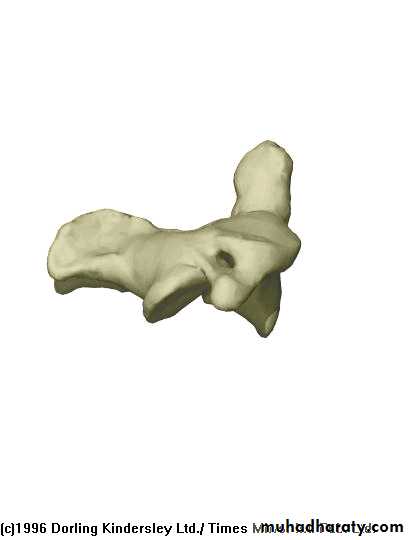
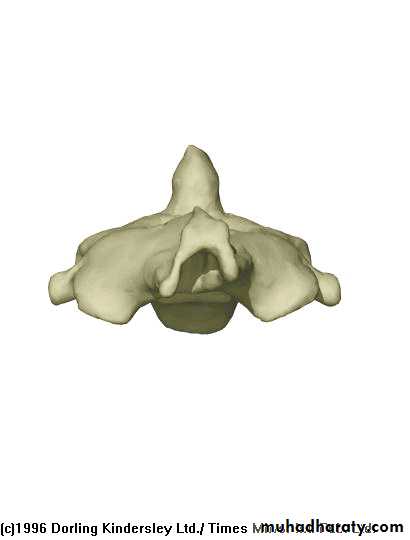
Cervical Vertebrae
Atlas (C1)
Axis (C2)C3-C7
Has two transverse foramen
Cervical Spine X-RayLateral radiograph
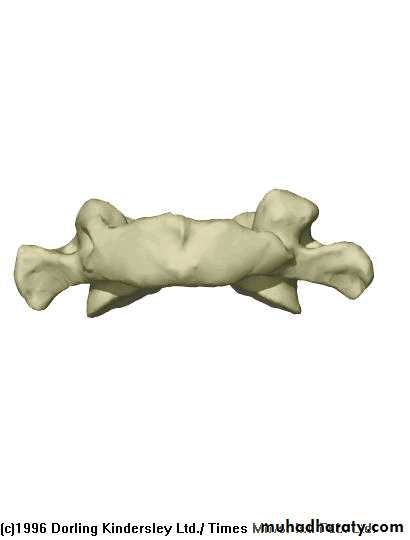
A/P radiographThoracic Anatomy
Curvature is Kyphosis
Gradual increase in sizeof vertebrae from top to bottom
Facets are aligned
horizontally
Articulate with ribs
Rigid
helps support the thorax
or trunk of the body
T1
T2
T3
T4
T5
T6
T7
T8
T9
T10
T11
T12
Thoracic Spine X Ray
Lateral radiograph
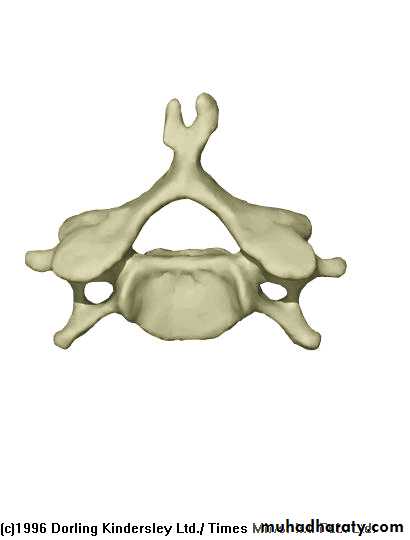
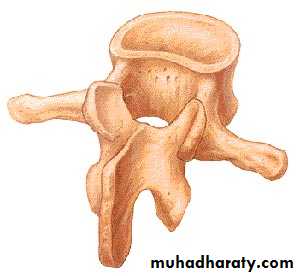
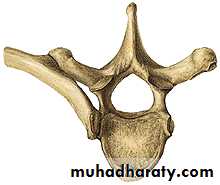
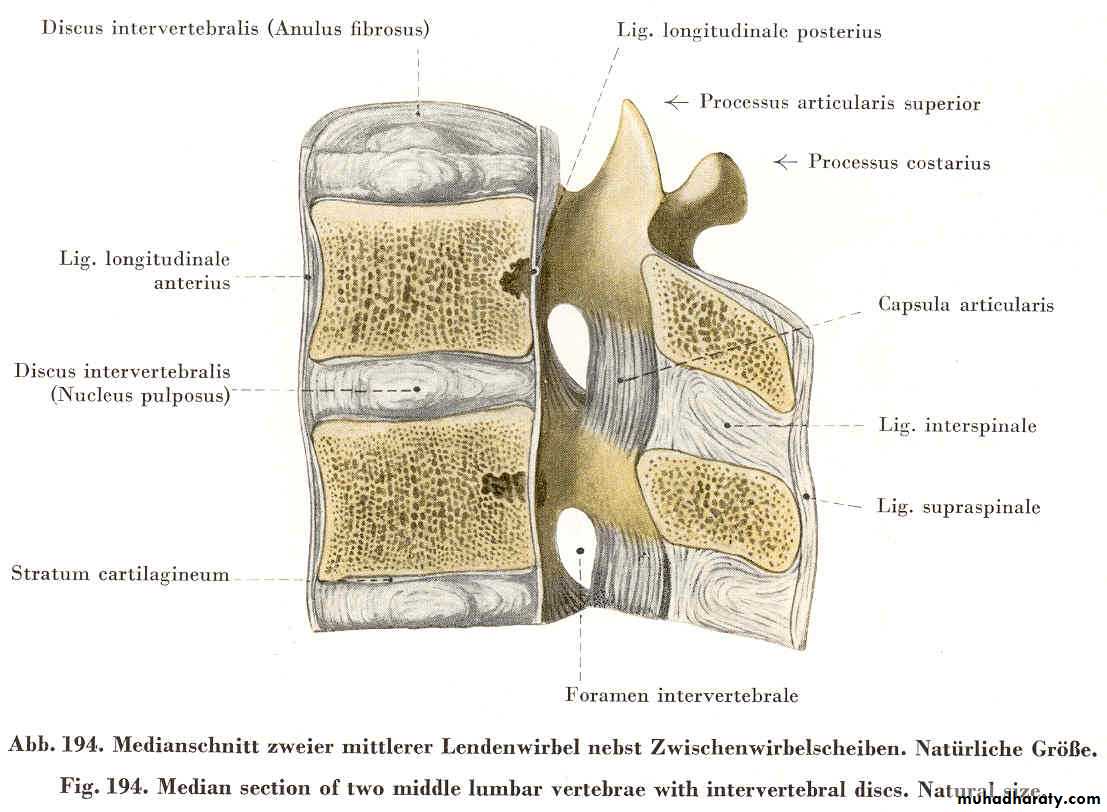
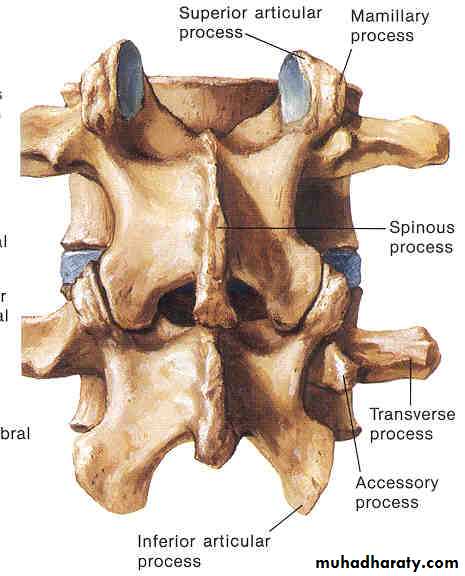
A/P radiographIn general a typical vertebra consists of :
large vertebral body in the front
two strong bony areas called pedicles connecting the vertebral body and the posterior archan arch of bony structures in the back (posterior arch) = (the spinous process).
BODY
PEDICLEspinous process
transverse process
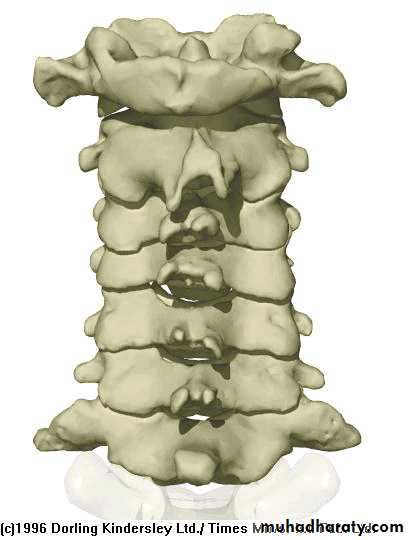
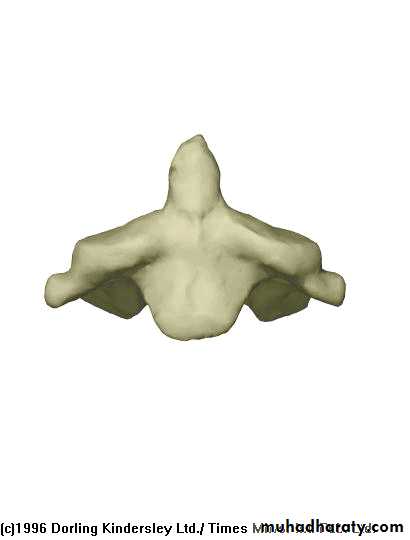
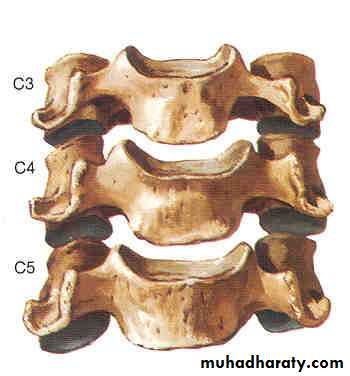
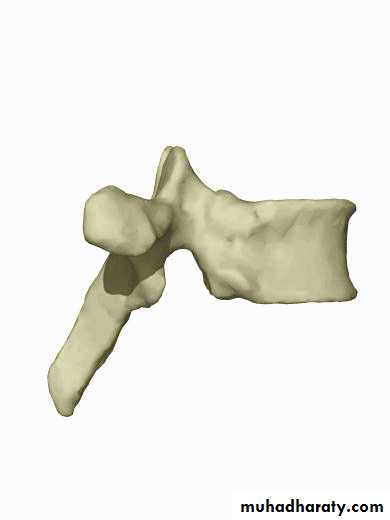
Lumbar Spine Anatomy
L1
L2
L5
L3
L4
Curvature is Lordotic
Facets are aligned vertically and allow bending
Vertebral body is kidney shaped in MRI
Lumbar Spine X Ray
Lateral radiograph
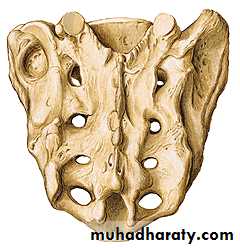
A/P radiograph• Sacrum
Sacrum ventral view
Sacrum posterior viewSacrum lateral view
median section
S3
S2
S4
S5
S1
S2 top view
CoccyxTriangular in shape formed by the fusion of four coccygeal vertebrae
Female coccyx points inferiorlyMale anteriorly
L4 superior view
L3 medial section
LaminaPedicle
Vertebral body
Spinous process
Processus articularis
Transverse processForamen
Vertebral Body
Thick disc-shaped anterior portionWeight bearing part
Superior & inferior surfaces roughened for attachment of the cartilaginous intervertebral disc
Anterior & lateral surfaces contain nutrient foramina for blood vessels
• Anterior
• Posterior
• 1• 2
• 3
• 4
• 5
• 6
• a
• b
• b
• Intervertebral Disc
• Two Vertebrae
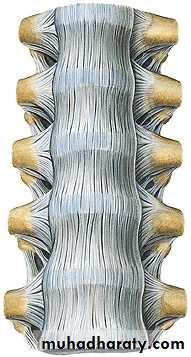
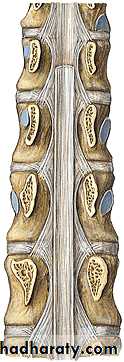
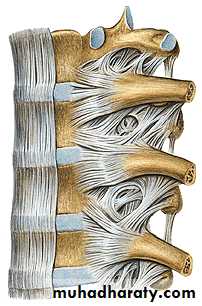
• Ligaments
• Anterior Longitudinal Ligament
• Posterior Longitudinal Ligament
• Capsular Ligament
• Ligamentum Flavum
• Interspinous Ligament
• Supraspinous Ligament
Ligaments
ALL
ALL
PLL
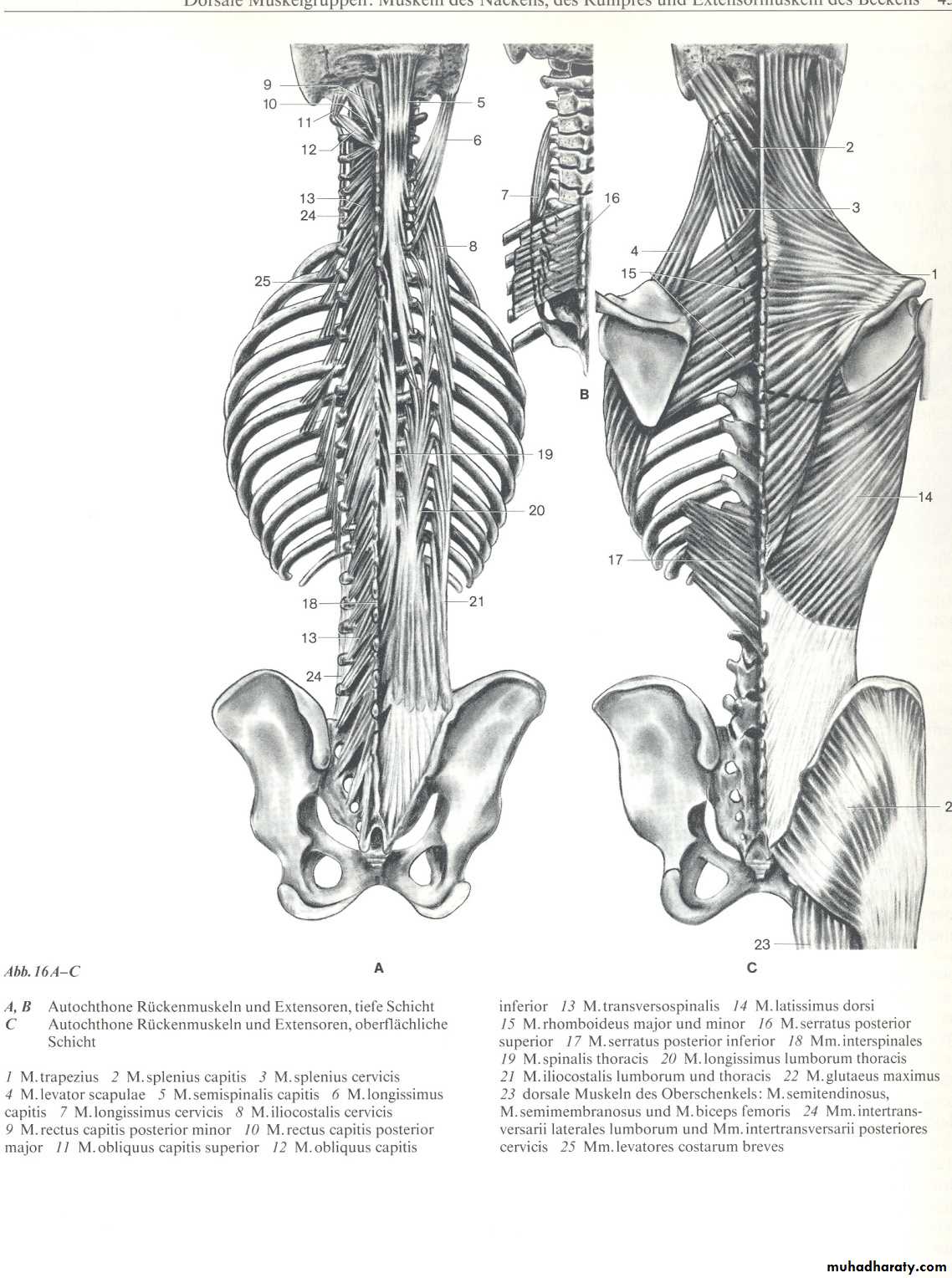
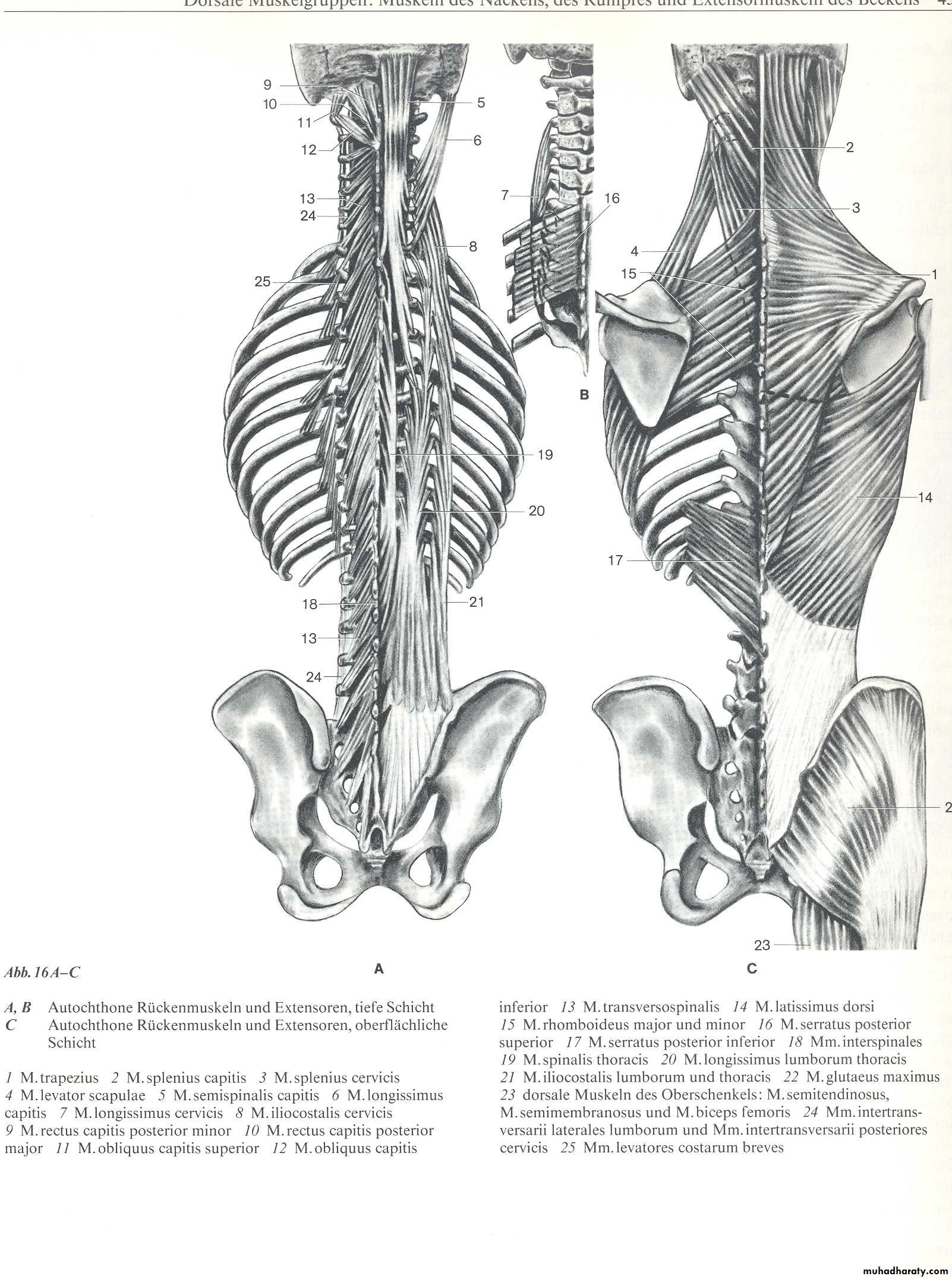
Anatomy: Posterior Muscles
Anatomy: Anterior Muscles
Motion Through Facets
PATHOPHYSIOLOGY OF SPINE INJURIES
Stable and unstable injuriesSpinal injuries carry a double threat: damage to the vertebral column and damage to the neural tissues.
While the full extent of the damage may be apparent from the moment of injury, there is always the fear
that movement may cause or aggravate the neural lesion; hence the importance of establishing whether
the injury is stable or unstable and treating it as unstable until proven otherwise.
A stable injury
is one in which the vertebral components
will not be displaced by normal movements;
in a stable injury, if the neural elements are undamaged
there is little risk of them becoming damaged.
An unstable injury
is one in which there is a significantrisk of displacement and consequent damage – or
further damage – to the neural tissues.
Posterior column
Posterior archPosterior ligaments
Inter-, Supraspinous lig.
Ligamentum flavum
Anterior column
Middle column
Posterior part of vertebral bodyPosterior longitudinal ligament
Posteror part of annulus
Anterior longitudinal ligament
Anterior part of annulus
Anterior part of vertebral body
Three column principle
Pathophysiology
Primary changes Physical injury may be limited to thevertebral column, including its soft-tissue components,
and varies from ligamentous strains to vertebral
fractures and fracture-dislocations. The spinal cord
and/or nerve roots may be injured, either by the initial
trauma or by ongoing structural instability of a
vertebral segment, causing direct compression, severe
energy transfer, physical disruption or damage to its
blood supply.
Secondary changes During the hours and days
following a spinal injury biochemical changes may lead
to more gradual cellular disruption and extension of
the initial neurological damage.
Mechanism of injury
Traction injury In the lumbar spine resisted muscleeffort may avulse transverse processes; in the cervical
spine the seventh spinous process can be avulsed (‘clay shoveller’s fracture’).
Direct injury Penetrating injuries to the spine,
particularly from firearms and knives, are becoming
increasingly common.
Indirect injury This is the most common cause of
significant spinal damage; it occurs most typically in a
fall from a height when the spinal column collapses in
its vertical axis,
NOTE: Insufficiency fractures may occur with
minimal force in bone which is weakened by osteoporosis
or a pathological lesion.
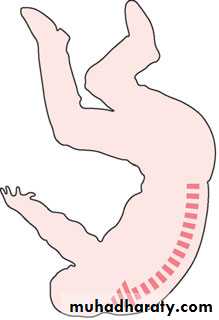
Mechanism of injury The spine is usually injured in
one of two ways: (a) a fall onto the head or the back ofthe neck; and (b) a blow on the forehead, which forces
the neck into hyperextension.
(a) (b)
DIAGNOSIS
History.
Examination.
1.NECK;
2.BACK; The patient is ‘log-rolled’ (i.e. turned over ‘in one piece’) to avoid movement of the vertebral column. The back is inspected for deformity
3. GENERAL EXAMINATION – ‘SHOCK.
4. NEUROLOGICAL EXAMINATION.5.IMAGING.
X-ray examination.
CT is ideal for showing structural damage to individual vertebrae.
MRI.
- Remember that the spine may be damaged in more
than one place.
- Do not accept poor quality images.
- Consult with the radiologist.
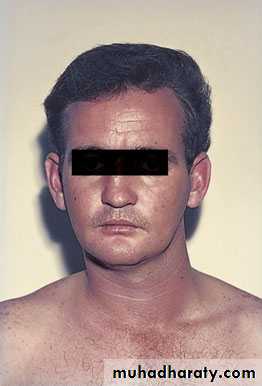
CERVICAL SPINE INJURIES
The patient will usually give a history of a fall from a height, a diving accident or a vehicle accident in which the neck is forcibly moved. In a patient unconscious from a head injury, a fractured cervical spine should be assumed (and acted upon) until proved otherwise.An abnormal position of the neck is suggestive, and careful palpation may elicit tenderness.
UPPER CERVICAL SPINE
Occipital condyle fractureThis is usually a high-energy fracture and associated
skull or cervical spine injuries must be sought. The
diagnosis is likely to be missed on plain x-ray examination
and CT is essential.
Impacted and undisplaced fractures can be treated
by brace immobilization for 8–12 weeks. Displaced
fractures are best managed by using a halo-vest or by
operative fixation.
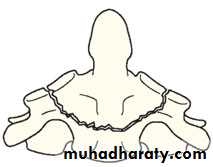
C1 ring fracture
Sudden severe load on the top of the head may cause
a ‘bursting’ force which fractures the ring of the atlas
(Jefferson’s fracture). There is no encroachment on
the neural canal and, usually, no neurological damage.
The fracture is seen on the open-mouth view (if the
lateral masses are spread away from the odontoid peg)
and the lateral view. A CT scan is particularly helpful
in defining the fracture.
Fracture of C1 ring Jefferson’s fracture – bursting
apart of the lateral masses of C1.Treatment
if stable and the patient wearsa semi-rigid collar
Or halo-vest until the fracture unites.
If there is sideways spreading of the lateral masses (more than 7 mm on the open-mouth view),
the transverse ligament has
ruptured; this injury is unstable and should be treated
by a halo-vest for several weeks. If there is persisting
instability on x-ray, a posterior C1/2 fixation and
Fractures of the atlas are associated with injury elsewhere in the cervical spine in up to 50 per cent of cases.
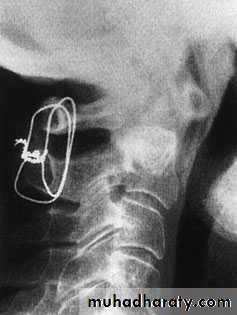
C2 pars interarticularis fractures
‘hangman’s fracture’ there are• bilateral fractures of the pars interarticularis of C2 and
• the C2/3 disc is torn;
2. the mechanism is extension with distraction.
This is one cause of death in motor vehicle accidents when the forehead strikes the dashboard.
Neurological damage, is unusual
because the fracture of the posterior arch tends to
decompress the spinal cord.
Nevertheless the fracture
is potentially unstable.
Undisplaced fractures which are shown to be stable
on supervised flexion–extension views (less than 3mmof C2/3 subluxation)
can be treated in a semi-rigid orthosis until united (usually 6–12 weeks).
Fractures with more than 3mm displacement but
no kyphotic angulation may need reduction; however,because the mechanism of injury usually involves distraction,
traction must be avoided.
After reduction, the neck is held in a halo-vest until union occurs.
C2/3 fusion is sometimes required for persistent pain and instability (‘traumatic spondylolisthesis’).
Occasionally, the ‘hangman’s fracture’ is associated with a C2/3 facet dislocation. This is a severely unstable injury; open reduction and stabilization is required.
Fracture of C2 ‘Hangman’s fracture’ – fracture of
the pars interarticularis of C2.C2 Odontoid process fracture
uncommon.occur as flexion injuries in young adults after highvelocity accidents or severe falls.
Also occur in elderly, osteoporotic people as a result of low-energy trauma in which the neck is forced into hyperextension,
cord damage is not uncommon and in
old people there is a considerable mortality rateClassification D’Alonzo
Type I – An avulsion fracture of the tip of the odontoidprocess due to traction by the alar ligaments. The fracture is stable (above the transverse ligament) and unites without difficulty.• Type II – A fracture at the junction of the odontoid
process and the body of the axis. This is the most
common (and potentially the most dangerous) type.
The fracture is unstable and prone to non-union.
• Type III – A fracture through the body of the axis.
The fracture is stable and almost always unites with
immobilization.
(type I) (type II) (type III)
Clinical featuresThe history is usually that of a severe neck strain
followed by pain and stiffness due to muscle spasm.
The diagnosis is confirmed by high quality x-ray
Imaging
Plain x-rays usually show the fracture, although theTomography is helpful
MRI has the advantage that it may reveal
rupture of the transverse ligament; this can cause
Treatment
Type I fractures Isolated fractures of the odontoid tipare uncommon. They need no more than
immobilization in a rigid collar until discomfort
subsides.
Type II fractures These are often unstable and prone to
non-union, especially if displaced more than 5 mm.
Undisplaced fractures can be held by fitting a halo-vest
Displacedfractures should be reduced by traction and can thenbe held by operative posterior C1/2 fusion;
Type III fractures If
undisplaced, these are treated in a
halo-vest for 8–12 weeks.
If displaced, attempts should
be made at reducing the fracture by halo traction,
which will allow positioning in either flexion or
extension, depending on whether the displacement is
forward or backward; the neck is then immobilized in
a halo-vest for 8–12 weeks.
LOWER CERVICAL SPINE C3 to C7
Posterior ligament injurySudden flexion of the mid-cervical spine in
damage to the posterior ligament complex (the interspinousligament, facet capsule and supraspinous ligament).
The upper vertebra tilts forward on the one
below, opening up the interspinous space posteriorly.
The patient complains of
pain and there may be localized tenderness posteriorly
X-ray may reveal a
slightly increased gap between the adjacent spines;
if the neck is held in extension this sign can be missed,
so it is always advisable to obtain a lateral view with the neck in the neutral position. A flexion view would, of course, show the widened interspinous spacethe injury is unstable and it should be treated as
a subluxation or dislocation. If it is certain that the
injury is stable, a semi-rigid collar for 6 weeks is adequate;
if the injury is unstable then posterior fixation and fusion is advisable.
Wedge compression fracture
A pure flexion injury results in a wedge compressionfracture of the vertebral body .The middle
and posterior elements remain intact and the
injury is stable. All that is needed is a comfortable collar for 6–12 weeks.
. Diagnosis.
1. The x-ray should be carefully
examined to exclude damage to the middle column
and posterior displacement of the vertebral body
fragment, i.e. features of a burst fracture (see below)
which is potentially dangerous. If there is the least doubt
2. an axial CT
3. MRI should be obtained.
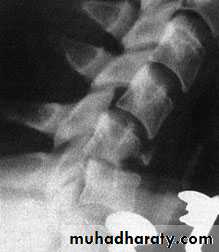
Burst and compression-flexion (‘teardrop’) fractures
These severe injuries are due to axial compression ofthe cervical spine,
usually in diving or athletic accidents
If the vertebral body is crushed in
neutral position of the neck the result is a ‘burst
fracture’. With combined axial compression and flexion,
an antero-inferior fragment of the vertebral body
is sheared off, producing the eponymous ‘tear-drop’
on the lateral x-ray. In both types of fracture there is a
risk of posterior displacement of the vertebral body
fragment and spinal cord injury.
diagnosis
Plain x-rays show either a crushed vertebral body(burst fracture) or a flexion deformity with a triangular fragment separated from the antero-inferior edge of the fractured vertebra (the innocent-looking ‘teardrop’).
CT or MRI should be performed
to look for retropulsion of bone fragments
into the spinal canal.
TREATMENT
If there is no neurological deficit, the patient can betreated surgically or by confinement to bed and traction
for 2–4 weeks, followed by a further period ofimmobilization in a halo-vest for 6–8 weeks.
If there is any deterioration of neurological status
while the fracture is believed to be unstable, and the
a threat of cord compression,
urgent anterior decompression is considered –
anterior corpectomy, bone grafting and plate fixation,
and sometimes also posterior stabilization.
Fracture-dislocations
Bilateral facet joint dislocations are caused by severe flexion or flexion–rotation injuries.
The inferior articular of one facets of one vertebra ride forward over the superior facets of the vertebra below.
Diagnosis
Lat X RAY
MRI
TREATMENT
it may be more convenient to immobilizethe neck in a halo-vest for 12 weeks.
Another alternative is to carry out a posterior fusion
as soon as reduction has been achieved; the patient is
then allowed up in a cervical brace which is worn for
6–8 weeks.
Posterior open reduction and fusion is also
indicated if closed reduction fails.
Unilateral facet dislocation
is the same as for bilateral dislocation.
Sometimes complete reduction is prevented by the
upper facet becoming perched upon the lower.
THORACOLUMBAR INJURIES
Most injuries of the thoracolumbar spine occur in the
transitional area – T11 to L2 – between the somewhat
rigid upper and middle thoracic column and the flexible
lumbar spine. The upper three-quarters of the
thoracic segments are also protected to some extent
by the rib-cage and fractures in this region tend to be
mechanically stable.
Pathogenesis
Pathogenetic mechanisms fall into three main groups:low-energy insufficiency fractures arising from comparatively mild compressive stress in
osteoporotic bone;
minor fractures of the vertebral processes due to compressive, tensile or tortional strains.
High energy fractures or fracture-dislocations due to major injuries sustained in motor vehicle collisions, falls or diving from
The common mechanisms of injury are:
• Flexion–compression – failure of the anterior column and wedge-compression of the vertebral body. Usually stable, but greater than 50 per cent loss of anterior height suggests some disruption ofthe posterior ligamentous structures.
• Lateral compression – lateral wedging of the vertebral body resulting in a localized ‘scoliotic’ deformity.
• Axial compression – failure of anterior and middle of retropulsion of a posterior fragment into the spinal canal. Often unstable.
• Flexion–rotation – failure of all three columns and a risk of displacement or dislocation. Usually unstable.
• Flexion–distraction – the so-called ‘jack-knife’ injury causing failure of the posterior and middle columns and sometimes also anterior compression.
• Extension – tensile failure of the anterior column and compression failure of the posterior column. Unstable.
Examination
Patients complaining of back pain following an injury
or showing signs of bruising and tenderness over the
spine, as well as those suffering head or neck injuries,
chest injuries, pelvic fractures or multiple injuries elsewhere, should undergo a careful examination of the spine and a full neurological examination, including rectal examination to assess sphincter tone.
Imaging
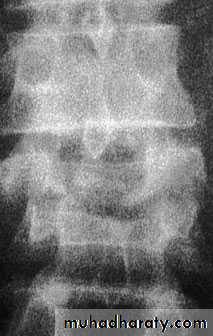
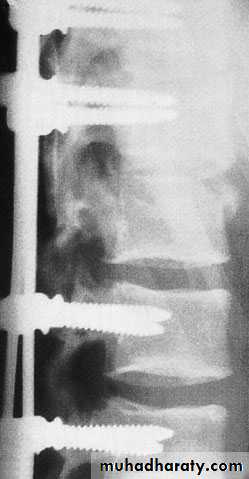
X-rays The anteroposterior x-ray may show loss of
height or splaying of the vertebral body with a crush
fracture
CT and MRI Rapid screening CT scans are now routine
in many accident units
MINOR INJURIES
Fractures of the transverse processesThe transverse processes can be avulsed with sudden muscular activity. Isolated injuries need no more than symptomatic treatment. More ominous than usual is a fracture of the transverse process of L5.
Fracture of the pars interarticularis
A stress fracture of the pars interarticularis should be
suspected if a gymnast or athlete or weight-lifter complains of the sudden onset of back pain during the course of strenuous activity. (traumatic spondylolysis). This is best seen in the oblique x-rays,
MAJOR INJURIES
Flexion–compression injury
This is by far the most common vertebral fracture and is due to severe spinal flexion, though in osteoporotic occur with minimal trauma.
The posterior ligaments usually remain intact,
Pain may be quite severe but the fracture is usually stable.
Neurological injury is extremely rare.
Those with moderate wedging (loss of 20–40 per cent) of anterior vertebral height) and a stable injury can be allowed up after a week, wearing a thoracolumbar brace or a body cast applied with the back in extension.
If loss of anterior vertebral height is greater than 40
per cent, it is likely that the posterior ligaments have
been damaged by distraction and will be unable to
resist further collapse and deformity. If the patient is
neurologically intact, surgical correction and internal
fixation is the preferred treatment,
If there is complete paraplegia with no improvement after 48 hours, conservative management is adequate;
the patient can be rested in bed for 5–6 weeks, then
gradually mobilized in a brace. With severe bony
injury, however, increasing kyphosis may occur and
internal fixation should be considered.
TREATMENT;
Axial compression or burst injury
Severe axial compression may ‘explode’ the vertebral body, causing failure of both the anterior and the middle columns. The posterior column is usually, but notalways, undamagedAnteroposterior x-rays may show
spreading of the vertebral body with an increase of the interpedicular distance
Posterior displacement of bone into the
spinal canal (retropulsion) is difficult to see on the plain lateral radiograph; a CT is essential.
.
If there is minimal anterior wedging and the fracture
is stable with no neurological damage, the patientis kept in bed until the acute symptoms settle (usually
under a week) and is then mobilized in a thoracolumbar brace or body cast which is worn for about 12 weeks.
However, any new symptoms such as tingling,
weakness or alteration of bladder or bowelfunction must be reported immediately and should
call for further imaging by MRI; anterior decompression
and stabilization may then be needed if there are
signs of present or impending neurological compromise
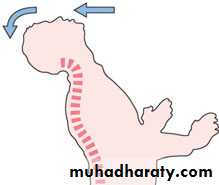
Jack-knife injury
Combined flexion and posterior distraction may cause the mid-lumbar spine to jack-knife around an axis that is placed anterior to the vertebral column. This is seen
most typically in lap seat-belt injuries
Neurological damage is uncommon,
the injury is (by definition) unstable.Xrays
may show horizontal fractures in the pedicles or transverse processes,
in the anteroposterior view the apparent height of the vertebral body may be increased. In the lateral view there may be opening up.
Fracture-dislocation
Segmental displacement may occur with various combinations of flexion, compression, rotation and shear.All three columns are disrupted and the spine is grossly unstable.
often associated with neurological damage to the lowermost part of the cord or the cauda equina.
TREATMENT
In neurologically intact patients, most fracture dislocations will benefit from early surgery.In fracture-dislocation with paraplegia, there is no convincing evidence that surgery will facilitate nursing, shorten the hospital stay, help the patient’s rehabilitation or reduce the chance of painful deformity
In fracture-dislocation with a partial neurological deficit, there is also no evidence that surgical stabilization and decompression provides a better
neurological outcome than conservative treatment.
In fracture-dislocation without neurological deficit, surgical stabilization will prevent future neurological complications and allow earlier rehabilitation.