DRUG ERUPTIONS
Adverse drug reactions are a common cause of dermatologic consultation.drug eruptions are not simply drug "allergy," but result from variations in
drug metabolism
immune status
coexistent viral disease
the patient's racial background
the patient's HLA status
the inherent chemical structure
dosage of the medication itself
Non-allergic drug reactions
Overdosageaccumulation of drugs
unwanted pharmacological effects (stretch marks from systemic steroids) .
idiosyncratic (odd reaction peculiar to one individual)
mouth ulcers cytotoxicity of methotrexate.
Silver based preparations, (argyria).
vaginal candidiasis: antibiotics remove resident bacteria
Dapsone or rifampicin, lepromatous leprosy, may cause erythema nodosum leprosum
Allergic drug reactions
appear after the latent period
Chemically related drugs may cross-react.
majority caused by cell-mediated immune reaction
commonly a maculopapular eruption
Helper CD4+ T cells morbilliform eruptions,
cytotoxic CD8+ T cells predominate in blistering eruptions ( TEN, Stevens–Johnson syndrome) and fixed drug eruptions.
urticaria and angioedema, immunoglobulin E (IgE) mediated type I hypersensitivity reactions
vasculitis type III immune complex-mediated reactions.
Evaluation
1. Previous general experience with the drug2. Alternative etiologic candidates
3. Timing of events
4. Drug levels and evidence of overdose
5. Response to discontinuation (dechallenge)
6. Rechallenge
Exanthems are the most common form of adverse cutaneous drug eruption.
They are characterized by erythema, often with small papules throughout.
They tend to occur within the first 2 weeks of treatment but may appear later, or even up to 10 days after the medication has been stopped.
Exanthems
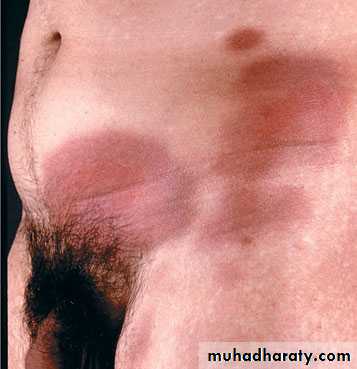
Lesions tend to appear first proximally, in the groin and axilla, generalizing within 1 or 2 days.the face may be spared. Pruritusis usually prominent, helping to distinguish a drug eruption from a viral exanthem.
Antibiotics, penicillins and trimethoprim
Urticaria/angioedema
Medications may induce urticaria by immunologic and nonimmunologic mechanisms.In either case, clinically there are pruritic wheals or angioedema .
Urticaria may be part of a more severe anaphylactic reaction (bronchospasm, laryngospasm, or hypotension).
Aspirin and the NSAIDs common causes of nonimmunologic
Immunologic urticaria is most associated with penicillinAngioedema is a known complication of angiotensin-converting enzyme inhibitors .
Lisinopril and enalapril more commonly than captopril
Angioedema typically occurs within a week of starting therapy.
Bullous drug reactions (Stevens-Johnson syndrome [SJS] and toxic epidermal necrolysis [TEN])
S]S and TEN are considered by some as parts of a disease spectrum based on the following:
1.commonly induced by the same medications.2.Patients initially presenting with S]S may progress to extensive skin loss resembling TEN.
3.The histologic findings are indistinguishable.
More than 100 medications have been reported to cause S]S and TEN.
S]S has less than 10% body surface area (BSA) involved, cases with 10-30% are S]S- TEN overlap cases, and more than 30% BSA erosion is called TEN .
1. trimethoprim-sulfamethoxazole
2.carbamazepine.
3.Antibiotics (long acting sulfa drugs and penicillins),
Fever and influenza-like symptoms precede eruption
Skin lesions appear on face and trunk and rapidly spread. macular, followed by desquamation, or may form atypical targets that coalesce, form bullae, then slough.In SJS, two or more mucosal surfaces are also eroded, the oral mucosa and conjunctiva being most frequently affected.
photophobia, difficulty with swallowing, rectal erosions, painful urination, and cough
Fixed drug reactions
Fixed drug reactions (FDE) are common.Fixed drug eruptions are so named because they recur at the same site with each exposure to the medication.
The time from ingestion of the offending agent to the appearance of symptoms is between 30 minutes and 8 hours, averaging 2 hours.
In most patients, six or fewer lesions occur, and frequently only one.
They may present anywhere on the body, but half occur on the oral and genital mucosa.Clinically, an FDE begins as a red patch that soon evolves to an iris or target lesion similar to erythema multiforme, and may eventually blister and erode.
Lesions of the genital and oral mucosa usually present as erosions.
Most lesions are 1 to several cm in diameter, but larger plaques may occurCharacteristically, prolonged or permanent postinflammatory hyperpigmentation results,
Erythema multiforme
Target-like lesions appear mainly on the extensor aspects of the limbs, and bullae may form.Sulphonamides
barbiturates
lamotrigine
phenylbutazone
Acute generalized exanthematous pustulosis
suggests acute pustular psoriasis, with a dramatic generalized eruption of red plaques studded with tiny non-follicular pustules.
Patients have fever and leucocytosis.
Antibiotics and diltiazem are the most common drugs to induce AGEP, which usually develops after only a few days.
Drug rash with eosinophilia and systemic signs syndrome
triad of fever, rash (from morbilliform to exfoliative dermatitis) and internal organ involvement (hepatitis, pneumonitis,nephritis and haematological abnormalities).An eosinophilia and lymphadenopathy
develops 3–8 weeks after starting the causative drug.
anticonvulsants
minocycline
allopurinol
sulphonamides
Hair loss
Predictable acitretin and cytotoxic agents,an unpredictable anticoagulants, antithyroid drugs.
Diffuse hair loss use of an oral contraceptive.
Hypertrichosis
dose-dependent effect of diazoxide, minoxidil and ciclosporin.
Pigmentation
Melasma may follow an oral contraceptive
phenothiazines blue–grey colour to exposed areas
heavy metals can cause a generalized browning
clofazimine makes the skin red
mepacrine turns the skin yellow
minocycline turns areas of leg skin a curious greenish grey colour
Photosensitivity reactions (photosensitive drug reactions)
most photosensitizing drugs have absorption spectra in the UVA, UVA penetrates into the dermis where the photosensitizing drug is present.
Phototoxic reactions are related to dose of both the medication and the UV irradiation. appear from hours to days after exposure.
Photoallergic reactions are typically eczematous and pruritic, and may first appear weeks to months after drug exposure.
.Treatment may include dose reduction and photoprotection, with a sunblock with strong coverage through the whole UVA spectrum.
Treatment
withdraw the suspected drugIn urticaria, antihistamines are helpful.
topical or systemic corticosteroids can be used, and applications of calamine lotion may be soothing.
Plasmapheresis and dialysis
Anaphylactic reactions require special treatment
One or more injections of adrenaline (epinephrine) 0.3–0.5 ml should be given subcutaneously
slow intravenous injection of chlorphenamine maleate (10–20 mg diluted in syringe with 5–10 mL blood).
intravenous hydrocortisone (100 mg), it should be given in severely affected patients.