1
The Urinary System
By
Dr. Mareb Hamed
Mosuel University
IRAQ
2
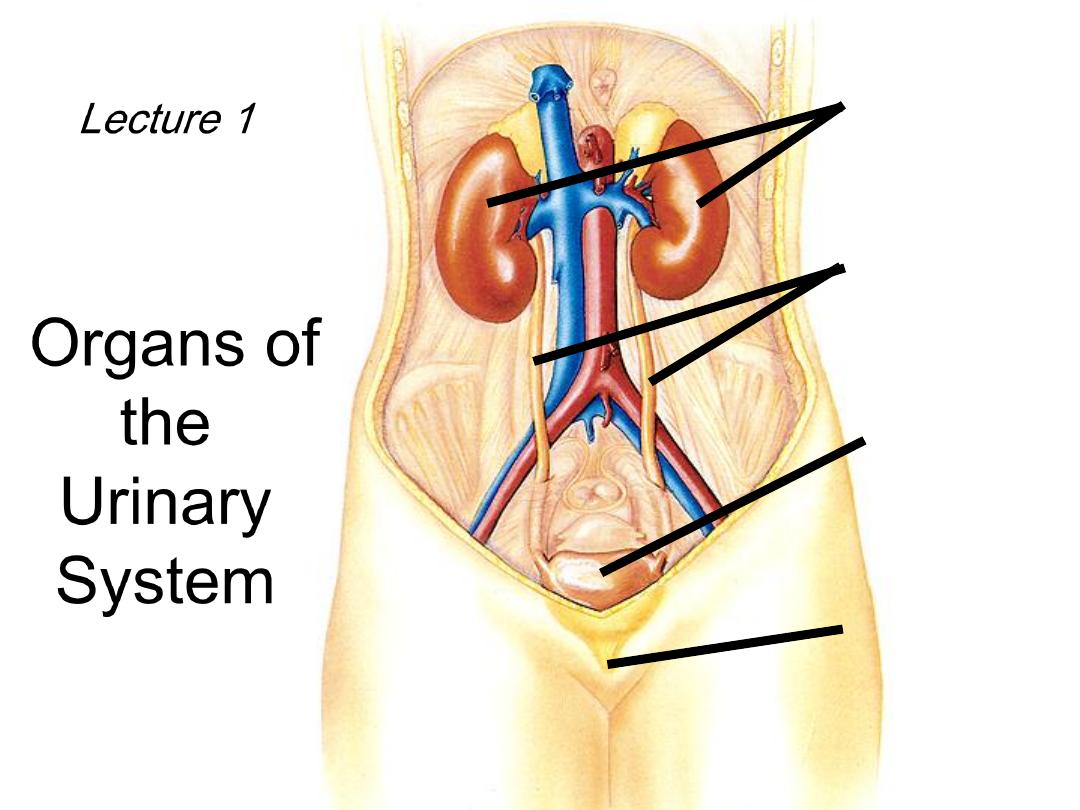
Lecture 1
Organs of
the
Urinary
System
kidneys
ureters
urinary
bladder
urethra
3

Kidney Functions
• Filters blood plasma, eliminates waste, returns
useful chemicals to blood
• Regulates blood volume and pressure
• Regulates osmolarity of body fluids
• Secretes renin, activates angiotensin, aldosterone
– controls BP, electrolyte balance
• Secretes erythropoietin, controls RBC count
• Regulates P
CO2
and acid base balance
• Detoxifies free radicals and drugs
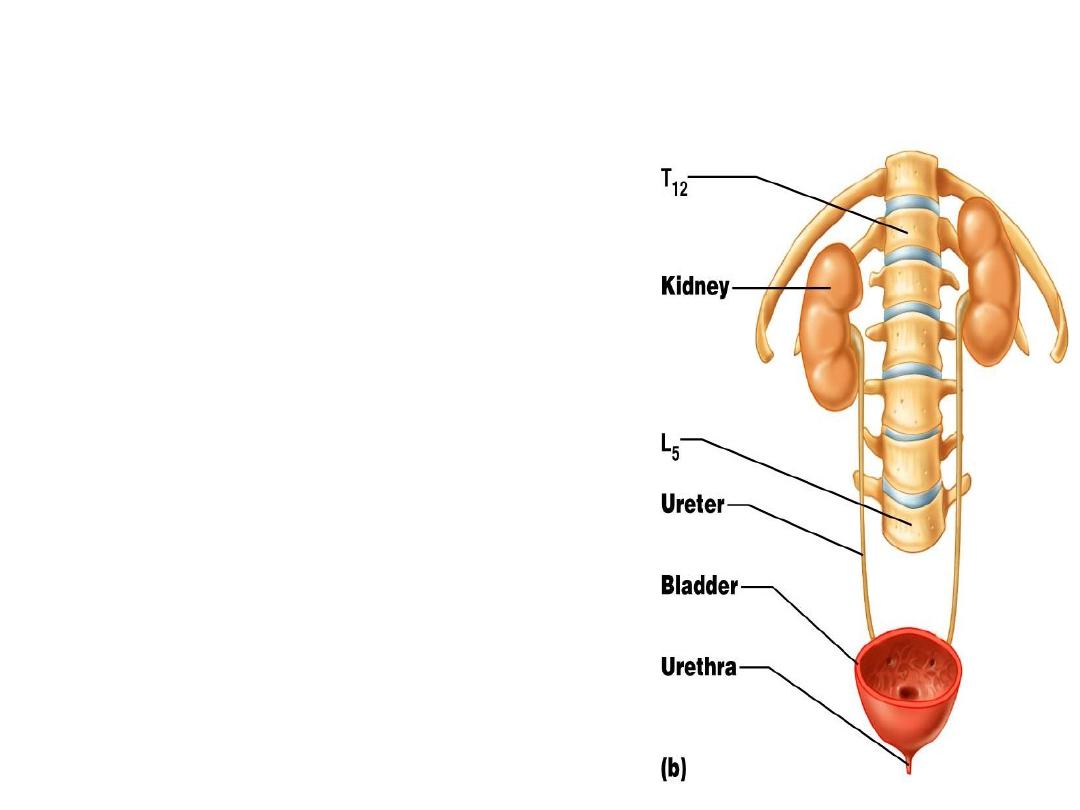
Anatomy of Kidney
• Position, weight and size
– retroperitoneal,
– level of T
12
to L
3
– about 160 g each
– size
10 cm long,
5 cm wide,
2 cm thick
– The left kidney is always
higher and nearer to the median
plane than the right
.

• Shape
– lateral surface - convex; medial - concave
• CT coverings
– renal fascia: binds to abdominal wall
– adipose capsule: cushions kidney
– renal capsule: encloses kidney like cellophane wrap
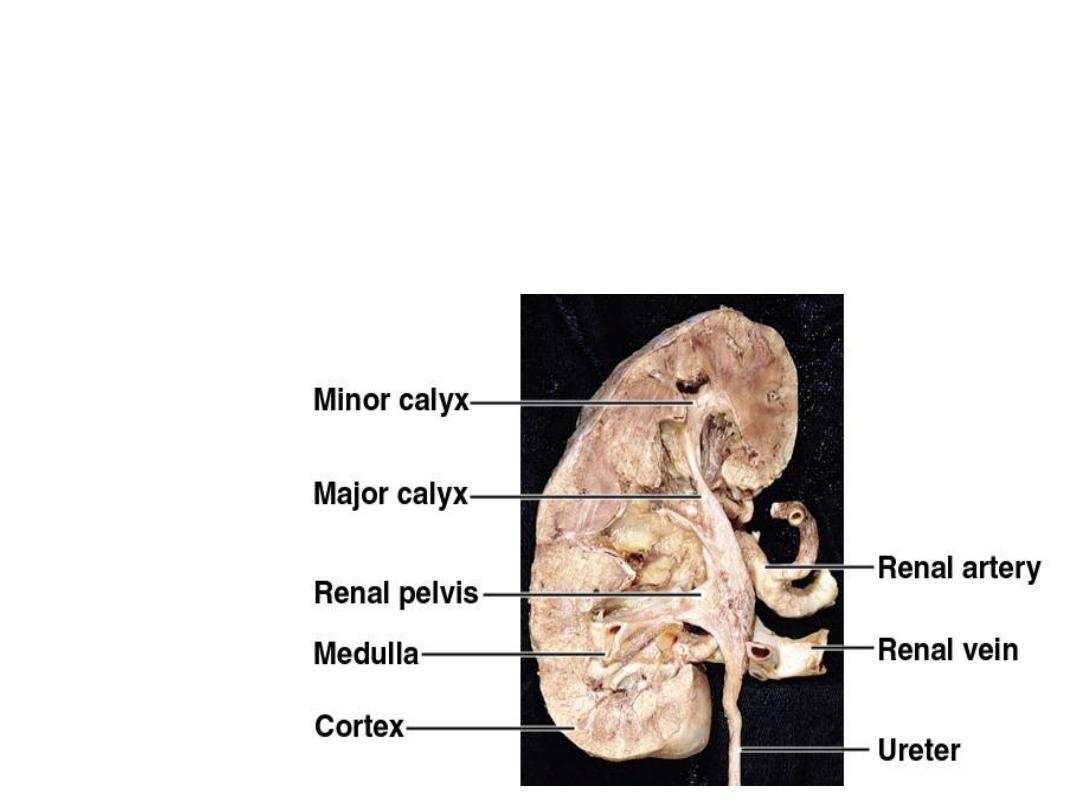
• Concave medial
hilum
leads to concave
renal sinus
containing renal vessels, lymphatics, sympathetic nerves, fat
and
renal pelvis
.
• Renal pelvis
(expanded upper end of ureter) is divided into
2-3
major calyces
, each divided into 2-3
minor calyces.
Minor calyx: cup over papilla collects urine
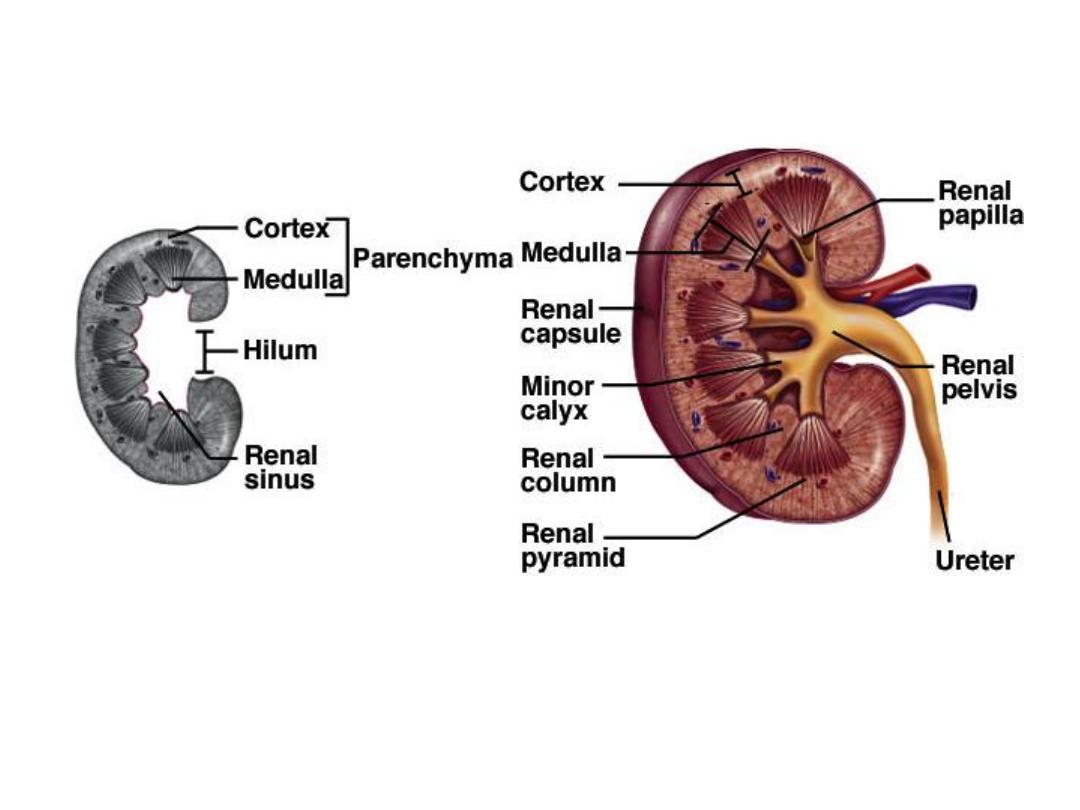
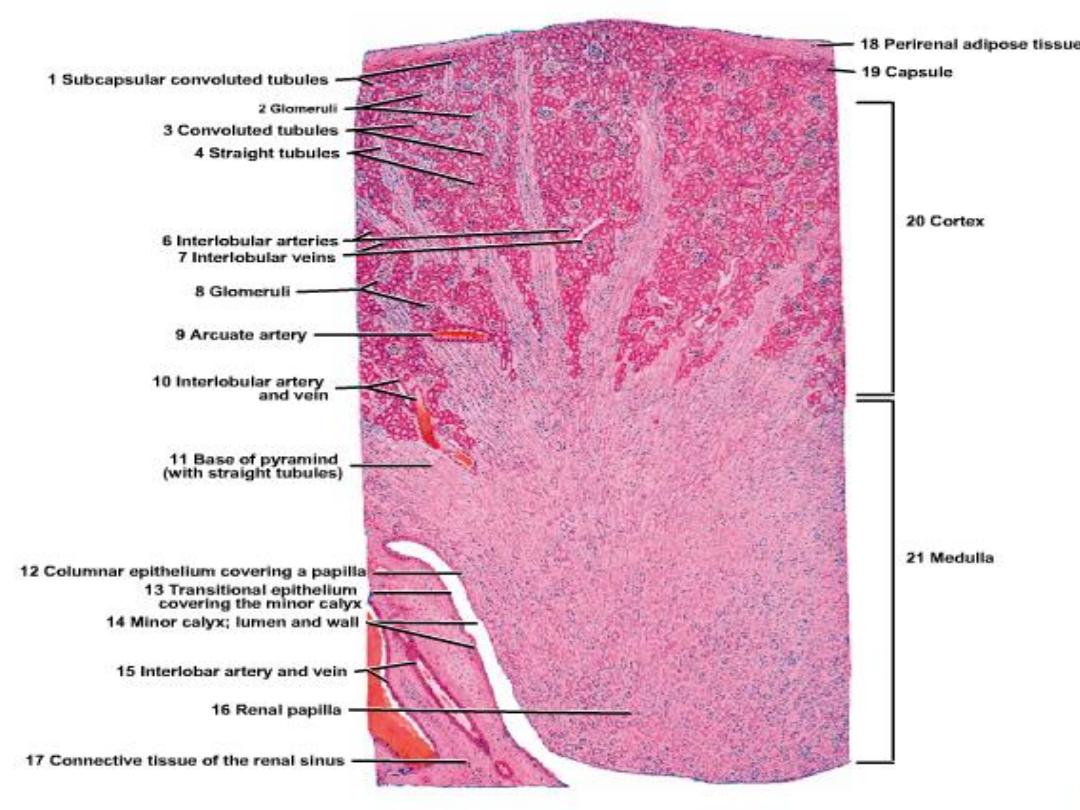
Anatomy of Kidney
• Renal cortex: outer 1 cm
• Renal medulla: renal columns, pyramids - papilla

Cortex & Medulla
• Cut section reveals
outer cortex and inner medulla
.
• Cortex
is granular due to
RC,PCT & DCT.
• Medulla
is striated
due to
LOH, CT
&
CD.
Medullary pyramids:
• 10-18.
• Bases towards cortex & apices towards hilum forming
renal
papillae
.
• Separated by cortical tissues called
columns of Bertini
.
Medullary rays
:
extend from bases of pyramids to cortex.
9
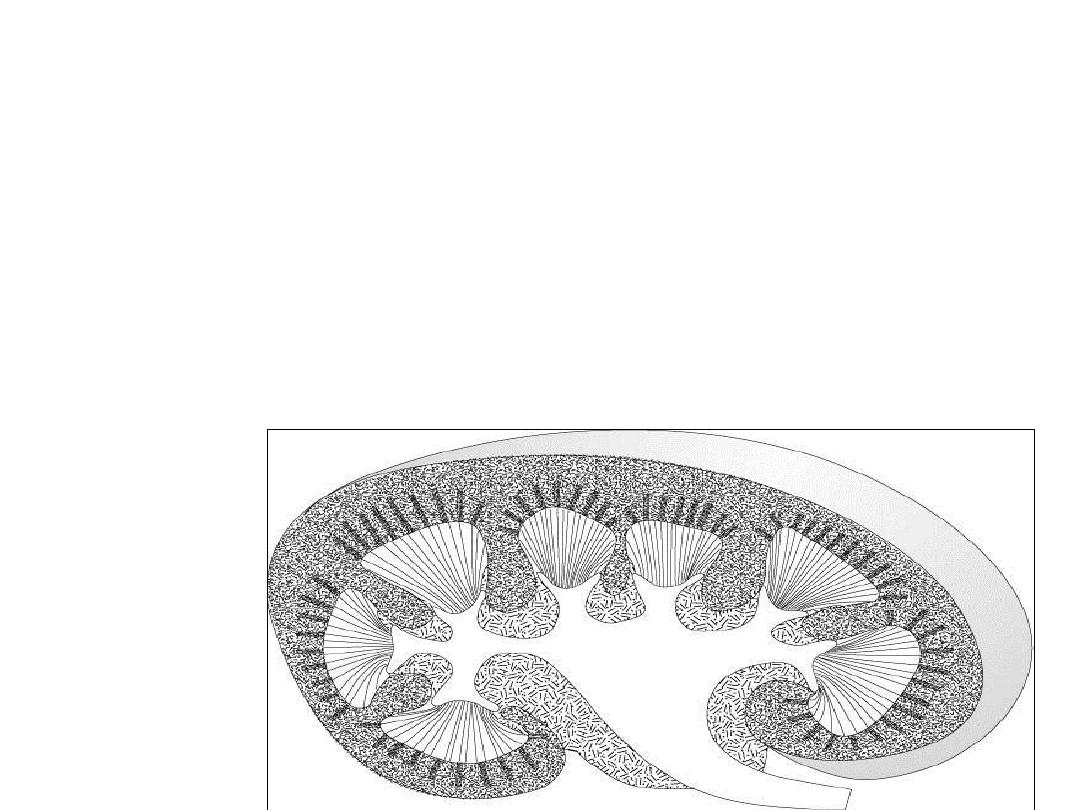
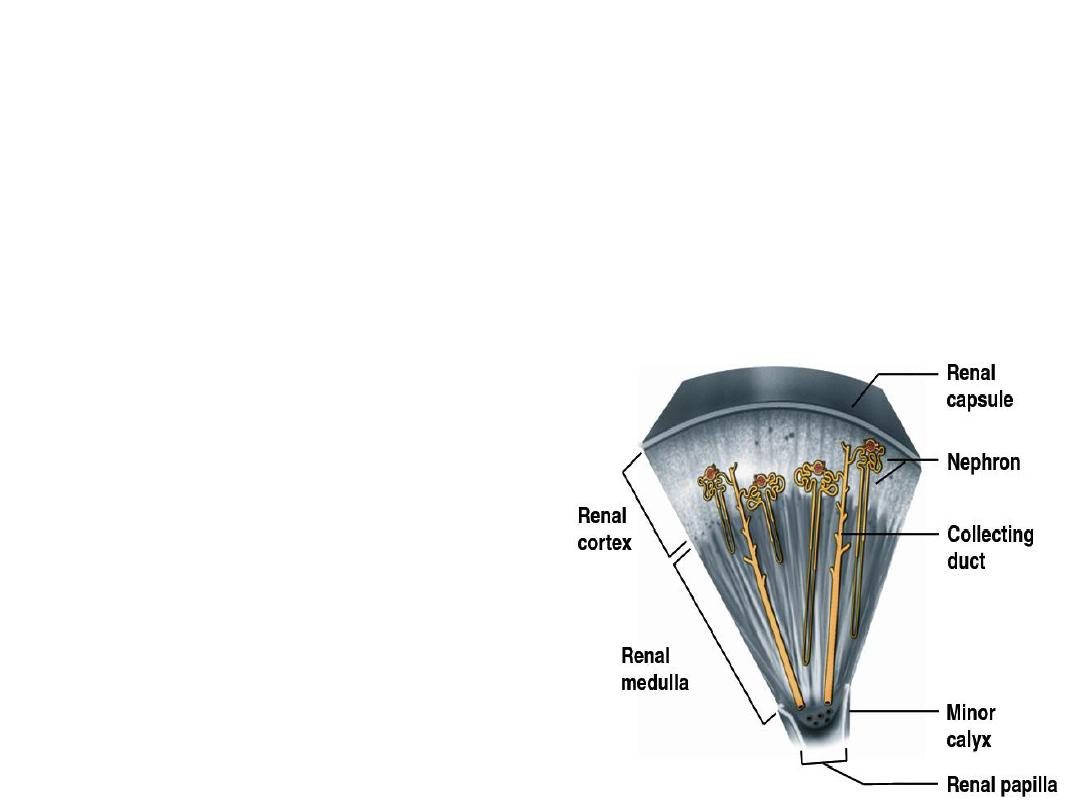
lobes & lobules
• Each kidney is divided into
lobes & lobules.
Renal lobe:
1 medullary
pyramid
+ associated cortical
tissue .
Renal lobule:
1 medullary
ray
+ associated cortical
tissue
No C.T.
septa between renal lobe & lobules.
10
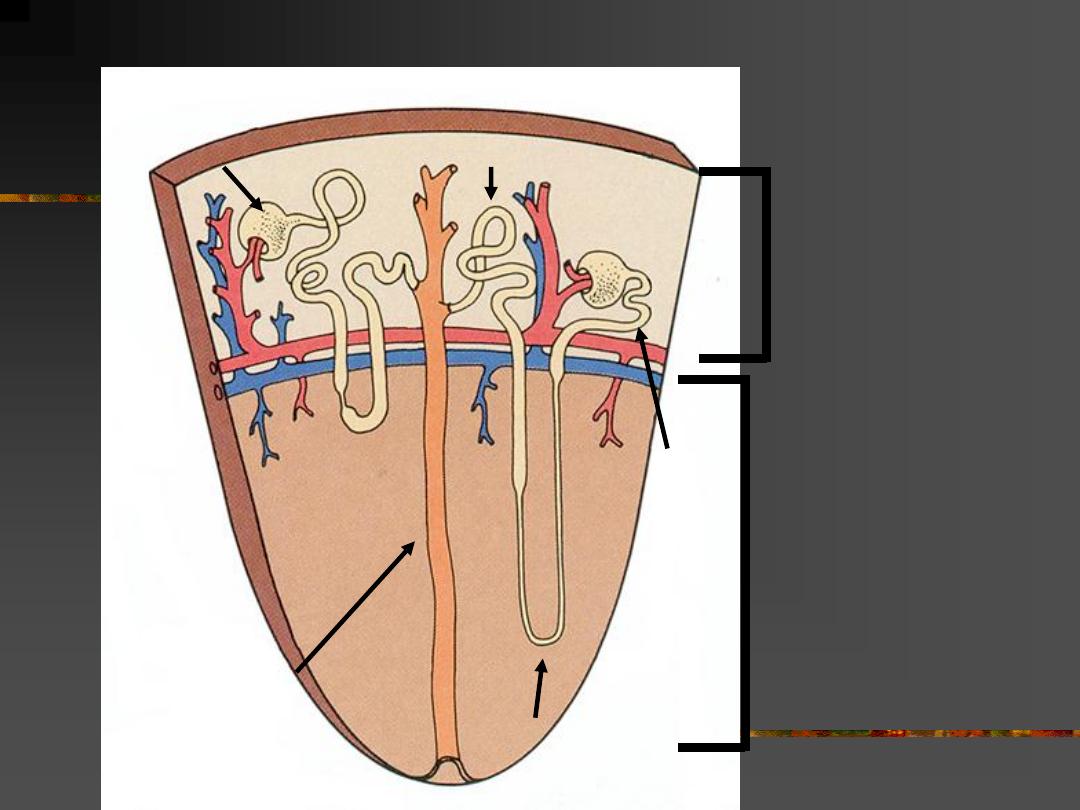
renal
cortex
renal
medulla
Each kidney contains over 1 million nephrons and thousands of collecting ducts
Collecting duct
Loop of Henle
PCT
DCT
Glomerulus
11
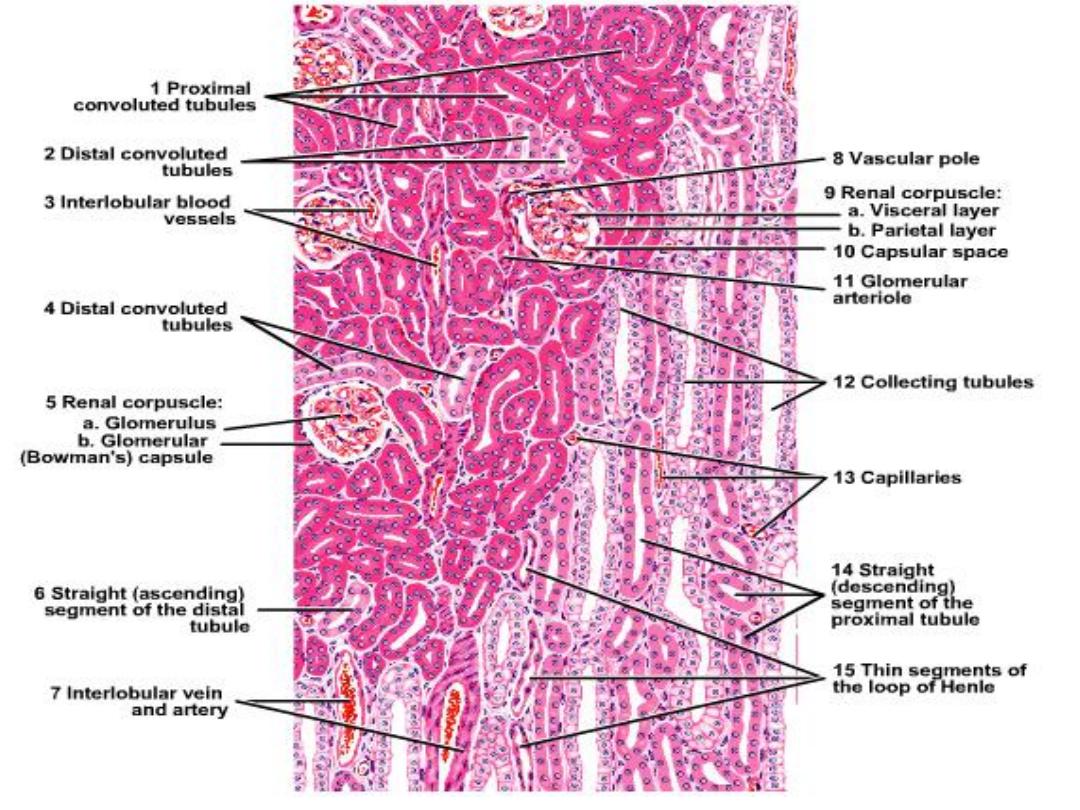
Histological aspects
Stroma
• C.T
capsule
surrounded by
fat
.
• Very little CT around BV
& reticular tissue between parenchyma
.
Parenchyma
Uriniferous tubules
:
–
Nephron
– Collecting tubule & duct
12

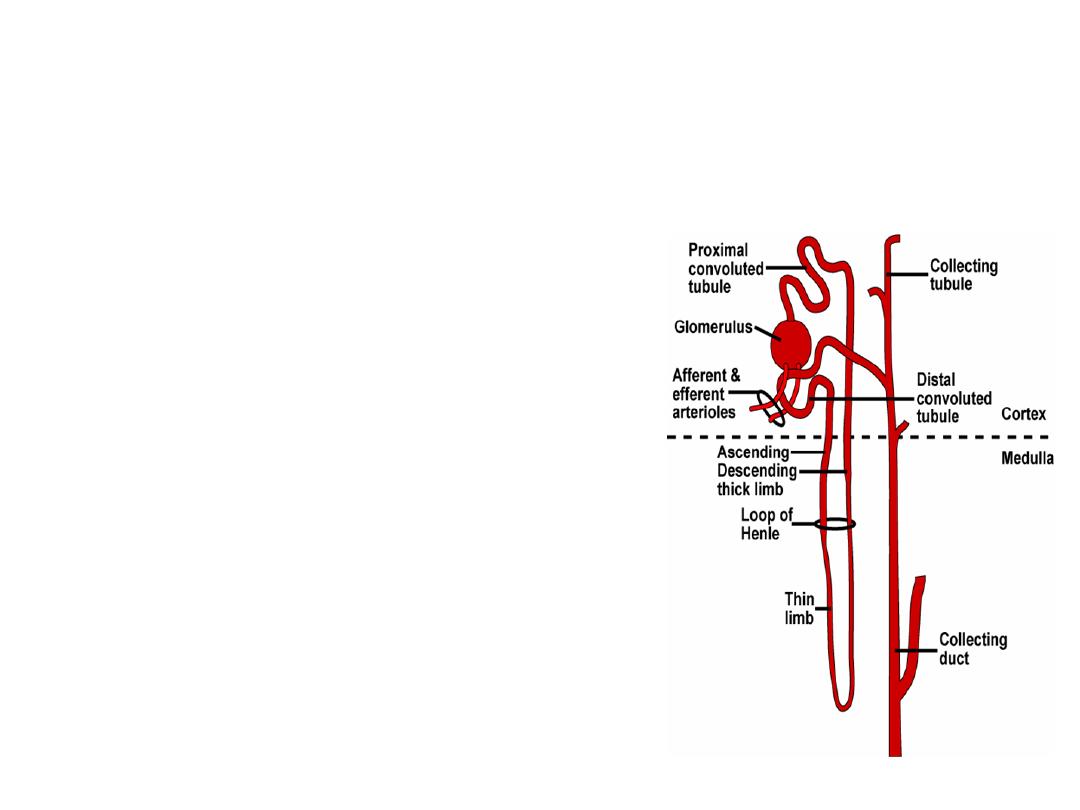
NEPHRON
• Structural and functional unit
of kidney
.
• Each kidney formed of
1-4 million nephrons
.
• 2-3 nephrons drain by 1 CT that join forming
duct of Bellini
.
Types
:
• Cortical
under capsule.
• Juxtamedullary
near medulla.
Parts
:
1-
Renal corpuscle
(Malpighian corpuscle
(
2-
Proximal convoluted tubule
(PCT)
3-
Loop of Henle
(LOH)
4-
Distal convoluted tubule
(DCT
(
13
14

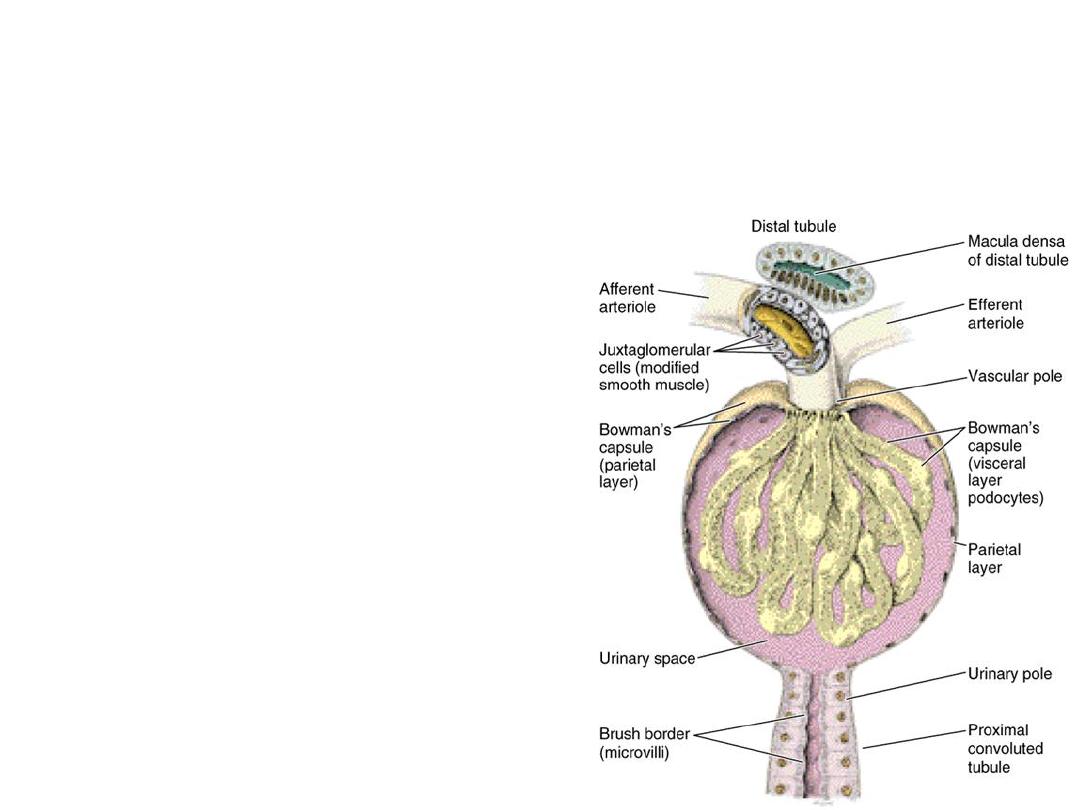
Renal corpuscle (RC)
•
Present in:
cortex.
•
Formed of:
a) Glomerulus
(tortuous tuft of capillaries).
b) Bowman's capsule
(double layer epithelial capsule
(
•
Has two poles:
a)
Vascular pole:
afferent arteriole enters & efferent
leaves.
b)
Urinary pole:
PCT begins.
•
Diameter:
200 um
.
•
Function:
filtrate blood and form urine.
15
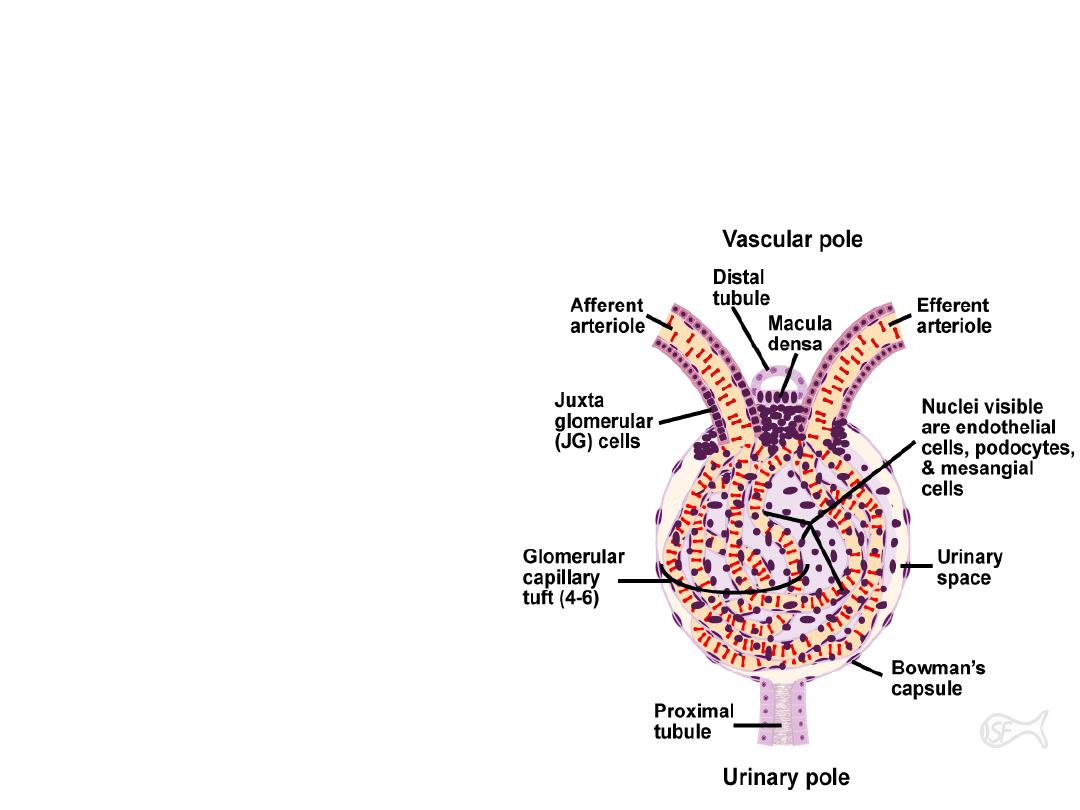
a) Glomerulus
• Tuft of anastomosing capillaries.
• Afferent arteriole
• enters
RC at vascular pole
• gives
glomerulus
• unite
forming
• Efferent arteriole
Glomerular capillaries
• lined by
fenestrated endothelium
• no diaphragm
• rest on
basement membrane
16

Basement membrane
- 300 nm thick.
- Formed of 3 layers:
• Middle lamina
densa
(collagen IV)
• Outer and inner laminae
rarae
-less
electron dense.
-
glycoproteins:
laminin+fibronectin
-
proteoglycans
.
17
Afferent & Efferent arterioles
• Lumen width is the
same
but diameter of
afferent is
larger
due
to
thicker
muscle
layer to
regulate
hydrostatic pressure
in
glomerular
capillaries.
18

Intraglomerular mesangial cells
• Present
inbetween loops of capillaries
• to support them
where a basement
membrane is lacking.
19

b) Bowman's capsule
Two layers
:
A-
Outer parietal layer:
simple squamous epithelium
.
B-
Inner visceral layer:
podocytes
adherent to
glomerular capillaries.
The capsular space
• between parietal & visceral layers
• receives
glomerular filtrate
• continuous with
PCT
.
20
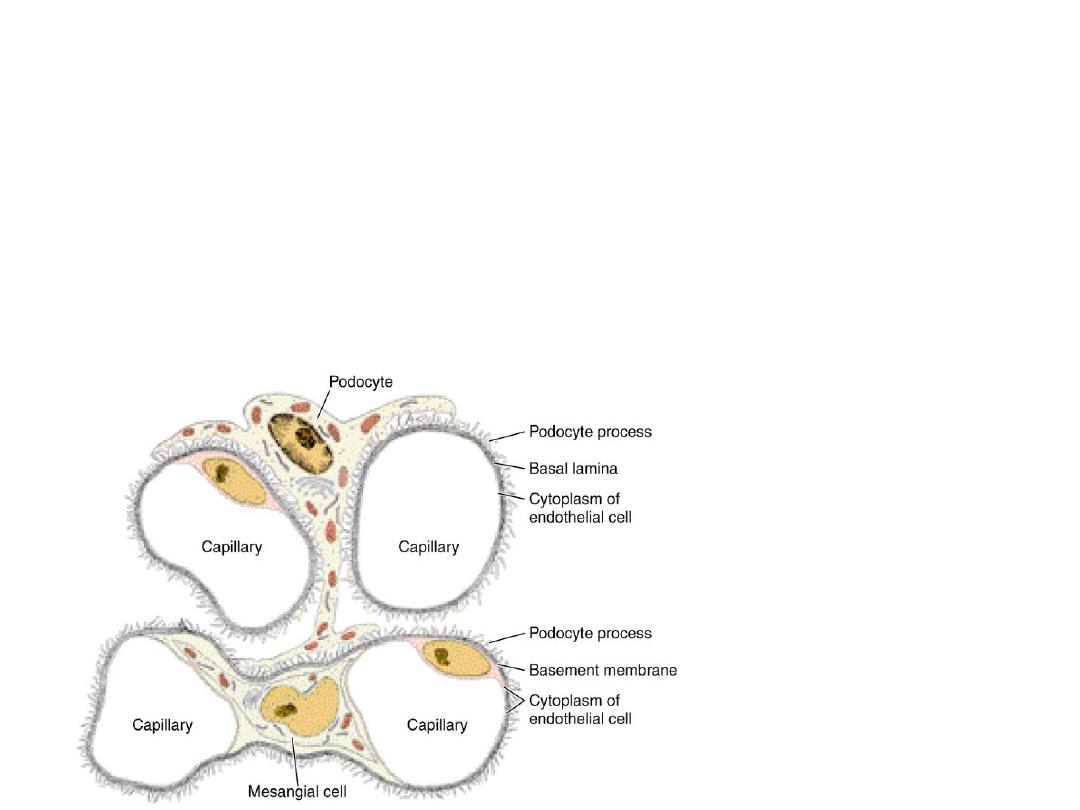
Podocyte L/M
• Star shaped
• multiple processes.
21
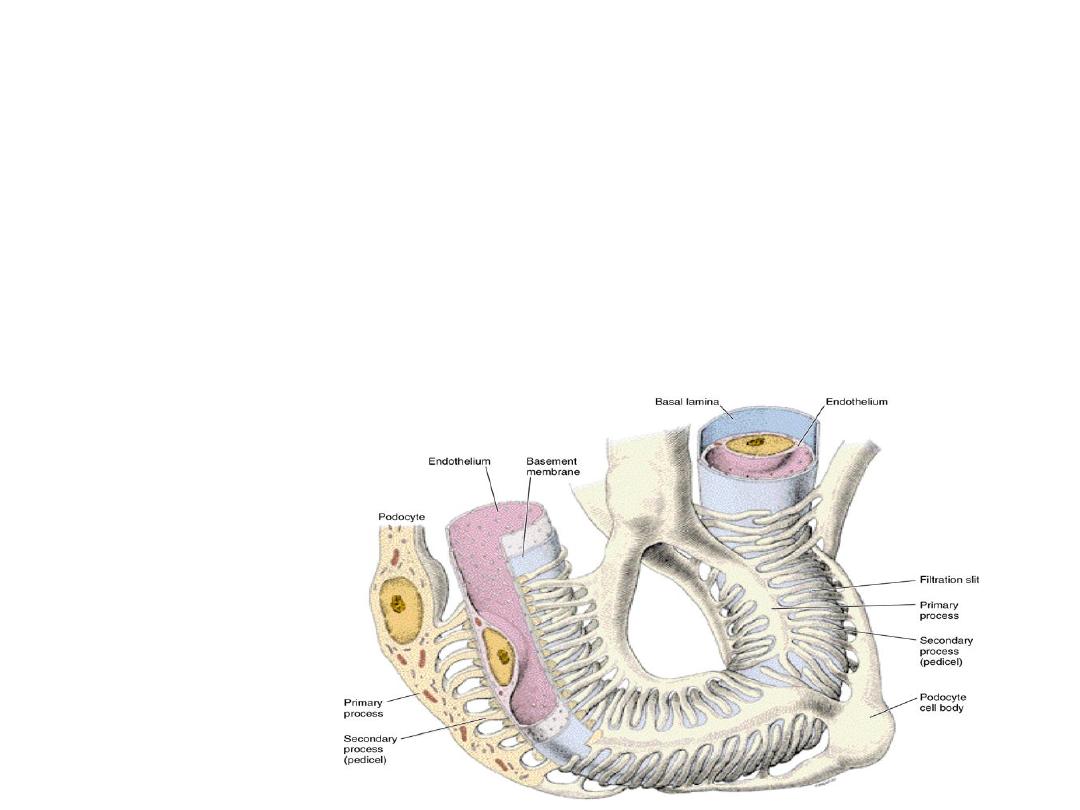
Podocyte
E/M
Large cell:
• Body
• 1ry processes (major)
• 2ry processes (minor)
22

• Cell body
:
• Central nucleus (extended chromatin),
• Cytoplasm: mitochondria, Golgi, RER, microtubules
& microfilaments.
• Processes:
microtubules & microfilaments
1ry process:
• parallel to long axis of blood capillary.
• gives rise to numerous
2ry processes.
.
2ry processes:
• end in
feet like structures
on basement membrane
of glomerular capillaries and
hence name of cell
.
23

• Inbetween the feet
, there are filtration slits
covered with diaphragm.
• Podocyte
Function
• Blood renal barrier.
• Regeneration of basement membrane.
24
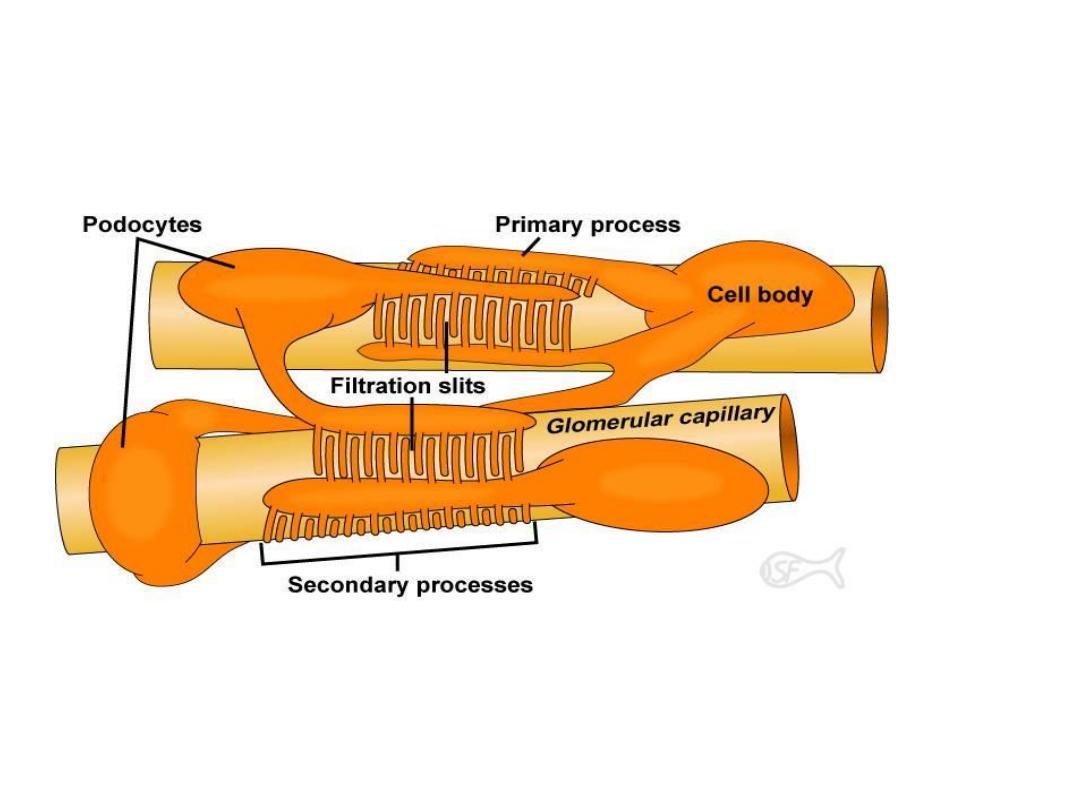
Podocytes team up to make filtration slits
25

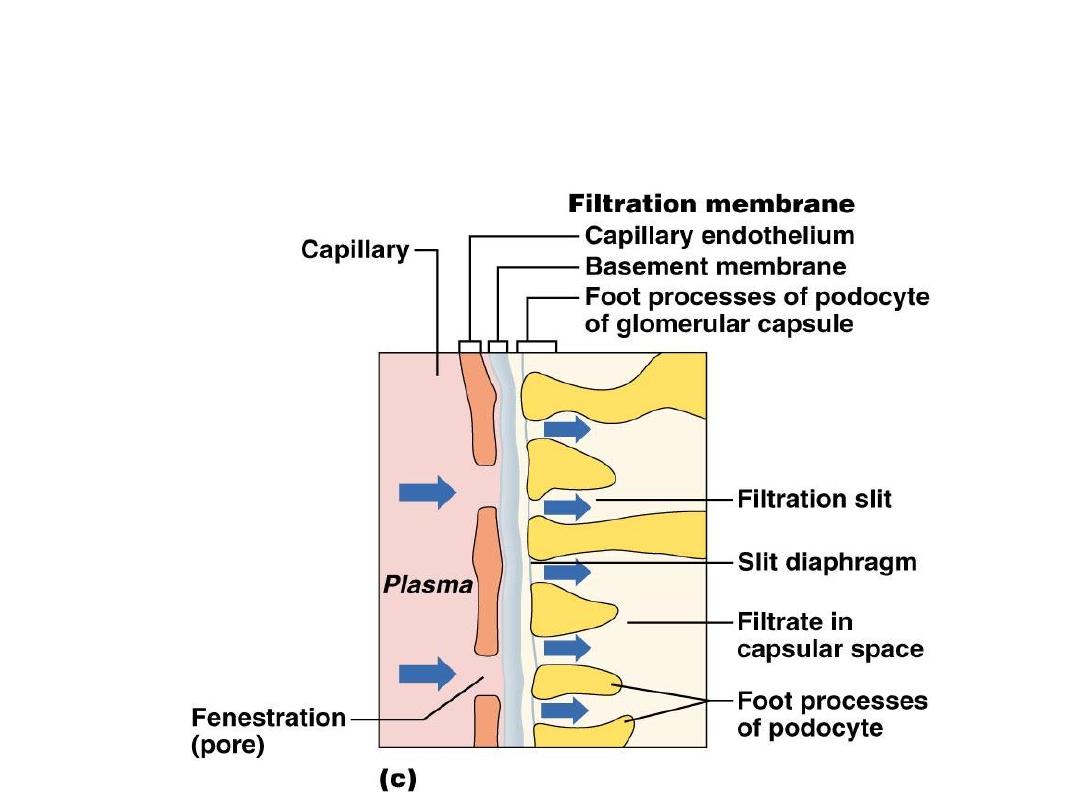
Blood-renal barrier
Formed of
:
1- Fenestrated endothelium of glomerular capillaries:
Hold back RBCs, WBCs & platelets.
2- Thick basement membrane:
(the only continuous layer).
High molecular weight
protein (> 68,000) can not pass.
Small molecular weight
sugar, amino acids & protein can pass.
3- Filtration slits
(60-100nm)
& overlying diaphragms:
Prevent molecules according to their
electrostatic charge.
Function:
Formation of glomerular filtrate
.
26
Renal Corpuscle and the
Filtration Membrane
27

Dr. Mareb
Lecture 2
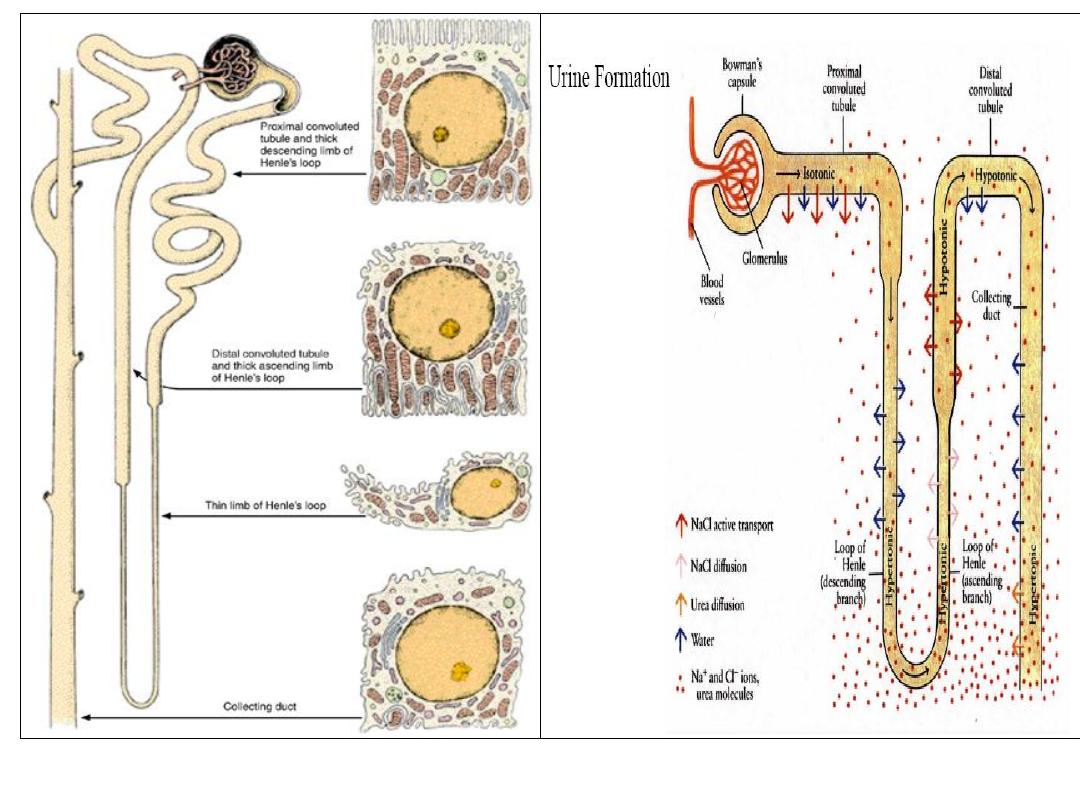
Proximal convoluted tubules
• Begins in
cortex at urinary pole of renal corpuscle.
• At first
highly convoluted
then
straightens
to
continue
with descending thick segment of LOH in medulla.
• Small lumen
with 60 um diameter and 14 mm long.
• Lined with
single layer of pyramidal cells
• Rest on
basement membrane.
28
29
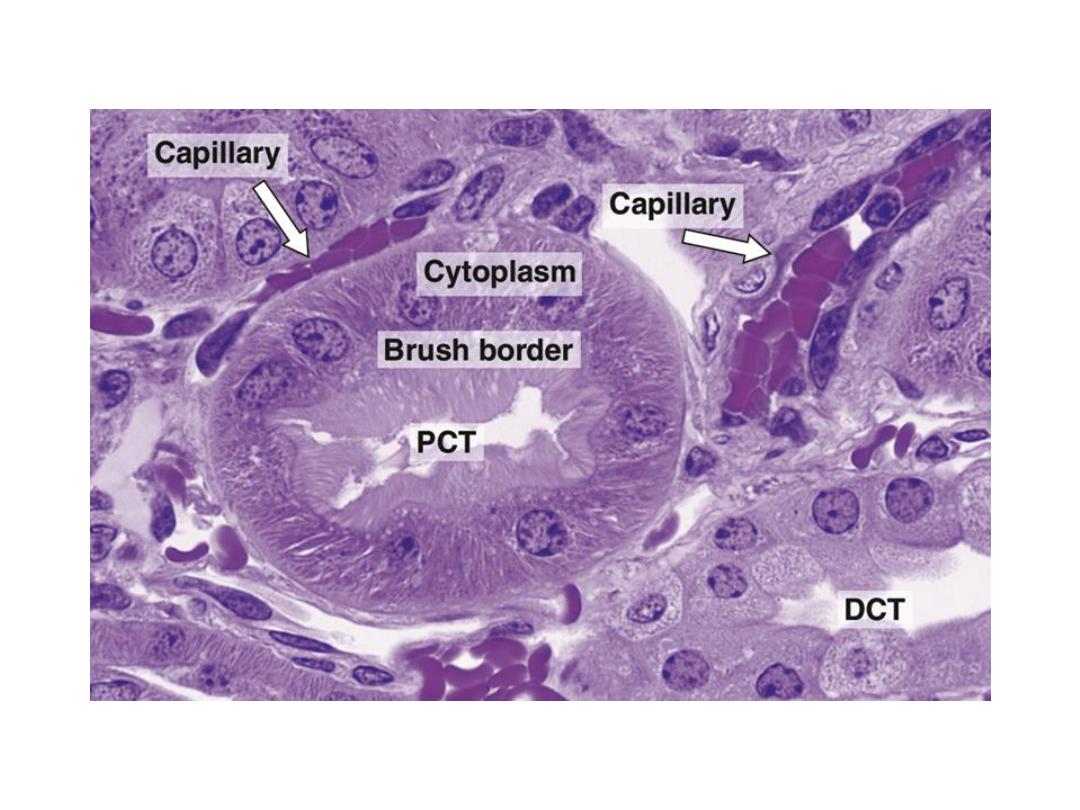
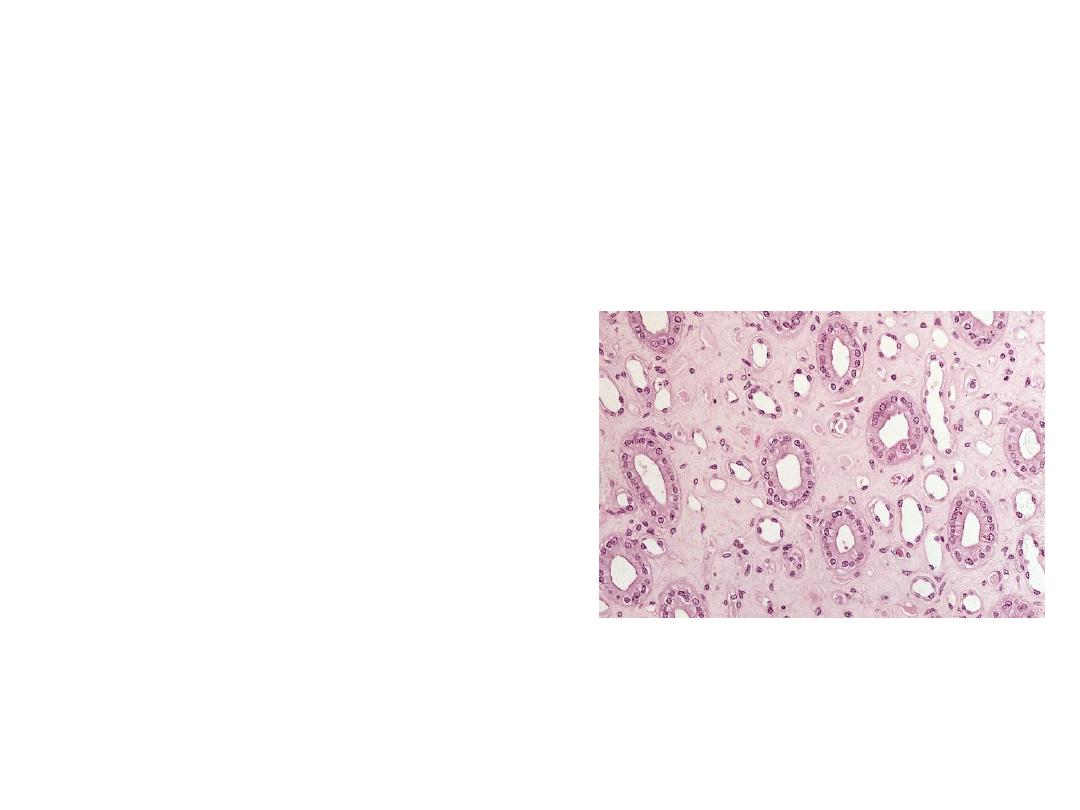
L/M & E/M
• Cells
4-5 pyramidal acidophilic.
• Lumen
narrow.
• Boundaries
indistinct
(Lateral interdigitations).
• Nuclei
rounded central.
• Apical
brush border
(microvilli ).
• Basal
acidophilic striations
(Mitochondria inbetween
infoldings).
30

Functions
-
Reabsorption of:
• 85% of sodium
activly
and 85% of water
passivly.
• all
glucose & amino acids.
• low molecular weight protein by pinocytosis →
endosomes
→ amino acids.
-
Excretion of:
• metabolites, dyes,drugs, urea and uric acid.
- The end result is
isotonic solution
.
31
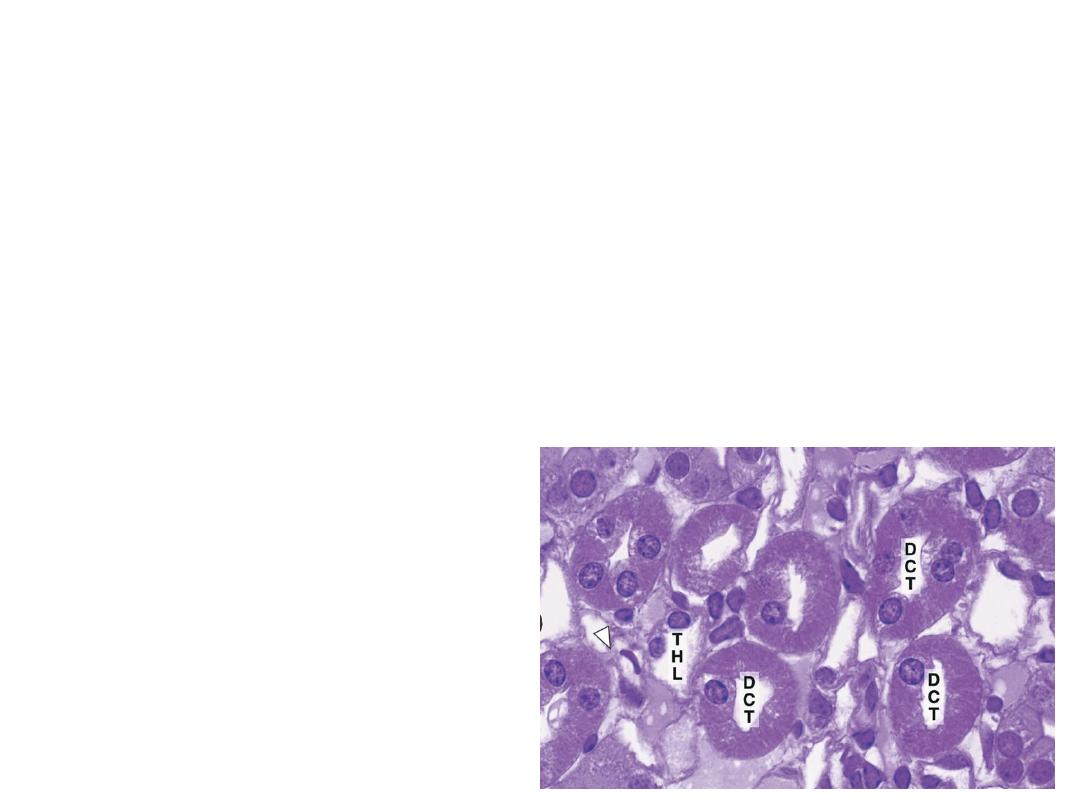
Loop of Henle
• U shaped tube present mainly in medulla .
Four parts
:
• Thick & thin
descending.
• Thin & thick
ascending
.
32

1-Thick descending part
• Starts in cortex and extends to medulla.
• Similar to
PCT
in structure and function.
33
2-Thin descending part
• In
medulla.
• Lined
with simple squamous epithelium
• Similar to
capillary wall but with no blood cells in lumen.
• Permeable
to water.
• Impermeable
to sodium.
• Urine becomes
hypertonic.
34

3-Thin ascending part
• In
medulla.
• Lined
with simple squamous epithelium.
35

4-Thick ascending part
• Starts in
medulla and extends to cortex.
• Similar to
DCT in structure and function.
• Permeable
to sodium.
• Impermeable
to water.
• Urine
becomes
hypotonic.
36

•
Subcapsular nephrons
(short LOH)
→ turn
of LOH in
thick ascending
part.
•
Juxtamedullary nephrons
(long LOH)
→ turn
of LOH in
thin descending
part.
37

Distal convoluted tubules
• In corticomedullary zone:
continuation of thick
ascending LOH.
• In cortex:
joins collecting tubules.
Three parts
:
1-Straight part:
continuous with ascending thick
limb of LOH
.
2-Macula densa:
close to afferent and efferent
arterioles. A part of juxtaglomerular apparatus
.
3-Convoluted part:
opens in collecting tubules
.
38
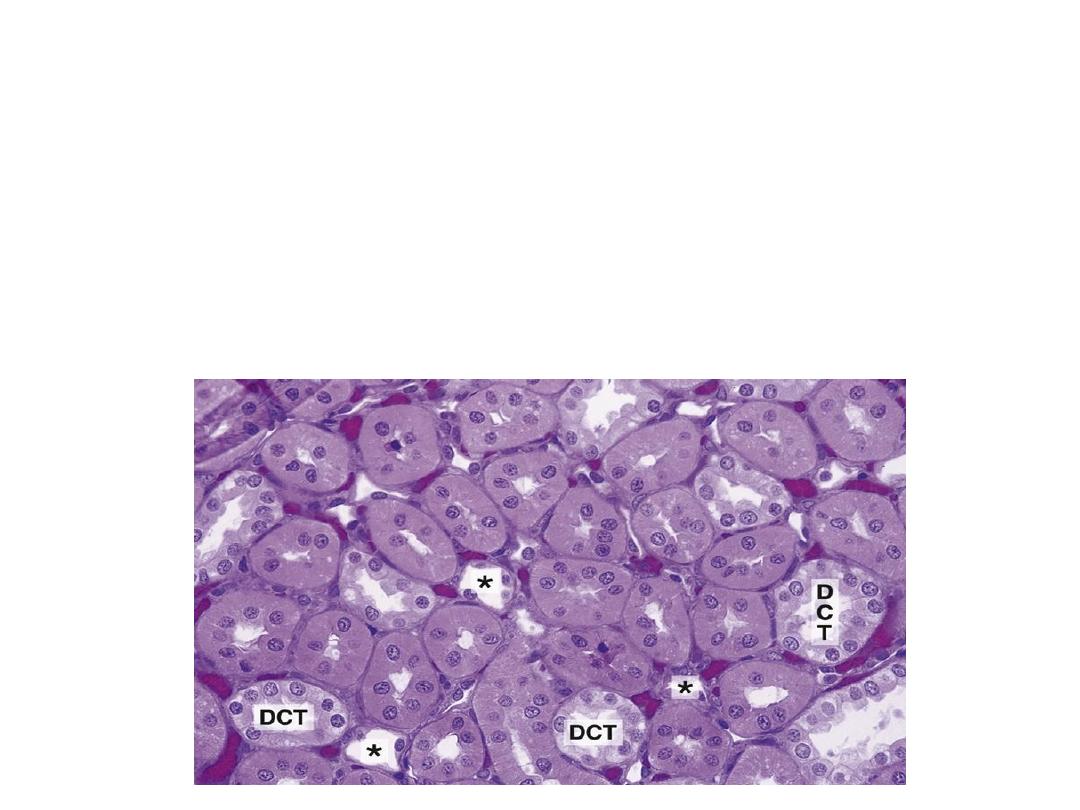
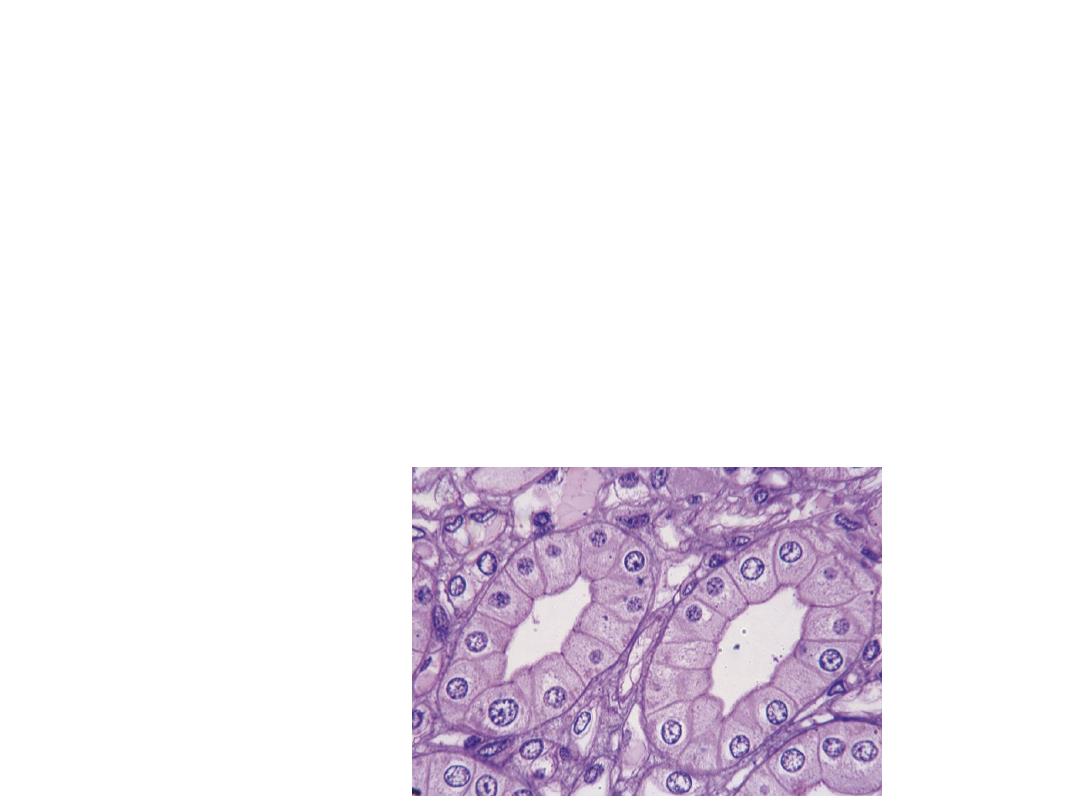
L/M & E/M
• Cells:
5-8 cubical small acidophilic.
• Lumen:
wide
.
• Boundaries:
distinct
(Less lateral interdigitations).
39
• Nuclei:
rounded central.
• Apical surface:
no brush borders
(few short
microvilli).
• Basal
acidophilic striation
(mitochondria
inbetween infoldings).
40

Functions
• Reabsorb 15%
sodium (activly) under control of
aldosterone.
• Reabsorb 15%
water (convoluted part) under control of
ADH.
• Excrete
hydrogen, ammonium & potassium ions.
• Maintain
acid-base balance of body.
41
42

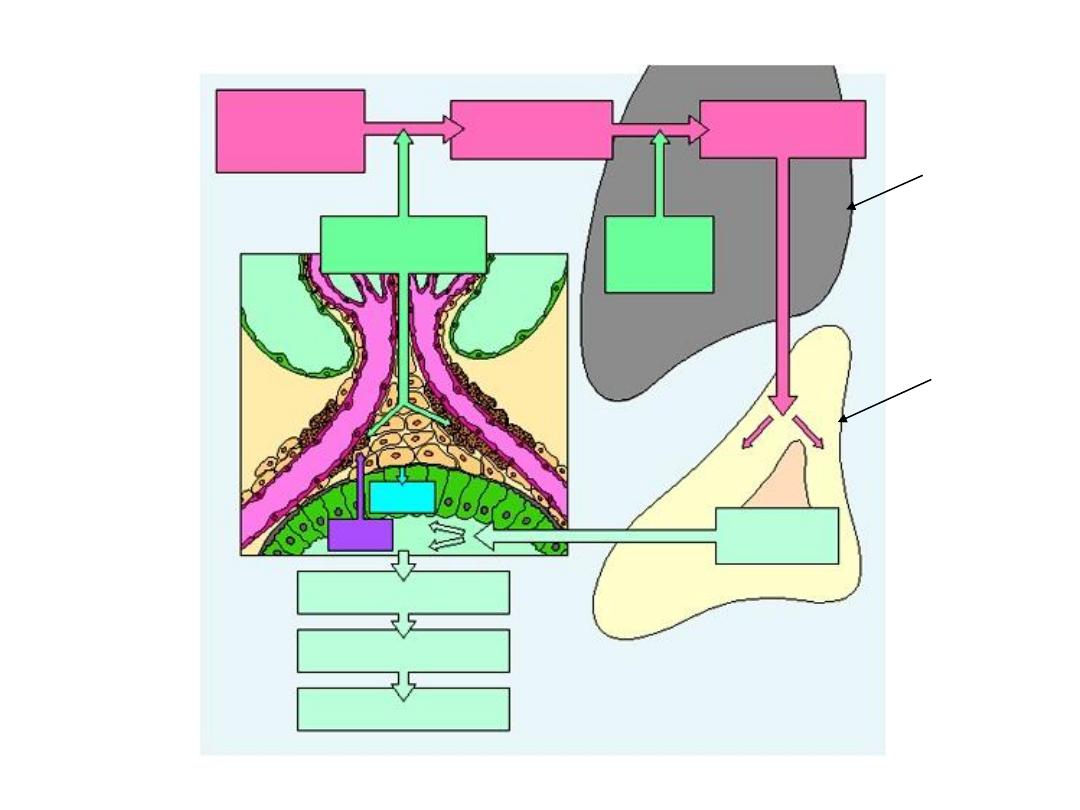
Juxtaglomerular apparatus
Is formed at the site of the contact between
the distal convoluted tubules with the
afferent arterioles
Composed of
:
1-Juxtaglomerular cells
.
2-Macula densa
.
3-Polar cushion
.
43

Afferent arteriole
• Tunica intima:
endothelium + C.T. + internal
elastic lamina.
• Tunica media:
smooth muscle cells.
• Tunica adventitia
44

1- Juxtaglomerular cells
• Modified smooth muscle cells
of tunica media of afferent
arterioles.
• Cells:
large cubical cells + rounded nuclei + cytoplasm
containing many PAS+ve secretory granules.
• EM:
RER, Golgi and mitochondria.
• Internal elastic lamina is absent,
• so juxtaglomerular cells are in contact in one side with
blood and endothelium
• and in other side with macula densa due to absence of its
basement membrane.
45

Function
1-Secrete
renin
→
• converts plasma angiotensinogen into angiotensin I →
• by converting enzyme in lung → angiotensin II →
• produce aldosterone by adrenal cortex →
• acts directly on DCT →
• water & sodium retention →
• increase blood pressure.
2-Secrete
erythropoietin
→ formation of erythrocytes
in bone marrow.
46
angiotensin I
angiotensin II
converting
enzyme
aldosterone
Adrenal
cortex
Water retention
sodium retention
↑
blood pressure
DCT
renin
angiotensinogen
Lung
47

Macula densa
• The part of
DCT
in concavity between afferent &
efferent arterioles of same nephron.
• Cells:
columnar with packed nuclei + numerous
microvilli and infranulear Golgi.
Functions
• Sensitive to
chloride ion
content of tubular fluid
→
signals for
constriction
of glomerular afferent
arteriole
→ regulates rate of glomerular filtrate.
48

Dr. Mareb
Lecture 3
COLLECTING TUBULES
• Not part of nephron.
• Different embryonic origin.
• Union of 2-3 DCT
→
collecting tubule
→
medullary
ray in cortex
→ main collecting tubule in medullary
pyramid
→
• Several medullary collecting tubules form straight
papillary
ducts of Bellini
→ apex of renal papillae →
minor calyx.
• 2-4
minor
calyces
→
major
calyx
→
renal pelvis
.
49
L/M & E/M
L/M
:
• Lined with simple
cubical
epithelium (in small tubules) or
simple
columnar
epithelium (in large tubules).
• Cytoplasm pale acidophilic.
• Cell borders distinct.
• Lumen
wide.
• Nuclei dark central.
E/M
:
• Few organelles.
• Interdigitations between cells not marked.
• Few microvilli and basal infoldings.
50
Function
• Water
is reabsorbed under control of
antidiuretic hormone.
• C
ollect,
c
oncentrate and
c
onduct urine
to
c
alyces
.
51
52

Renal interstitial tissue
• The kidney is invested by C.T capsule easily stripped.
• Medullary interstitial CT cells are macrophages, fibroblasts
& interstitial cells.
Interstitial cells:
• more numerous
• elongated nuclei
• numerous lipid droplets
• Synthesize
medullipin I
converted in liver into
medullipin ll
(potent vasodilator lowers blood pressure).
53
Renal Circulation
Segmental arteries
Interlobar arteries
Arcuate arteries
Interlobular arteries
Afferent arterioles
Glomerulus
Efferent arterioles
Peritubular capillaries
Segmental veins
Interlobar veins
Arcuate veins
Interlobular veins
Venules
Renal Artery
Renal Vein
54

Excretory passages
• Minor calyces, major calyces, renal pelvis,
ureter, urinary bladder and urethra
.
• Urine collected from
ducts of Bellini
→
minor
calyces.
• 2-4
minor
calyces
→
major
calyx
→
renal pelvis
.
55
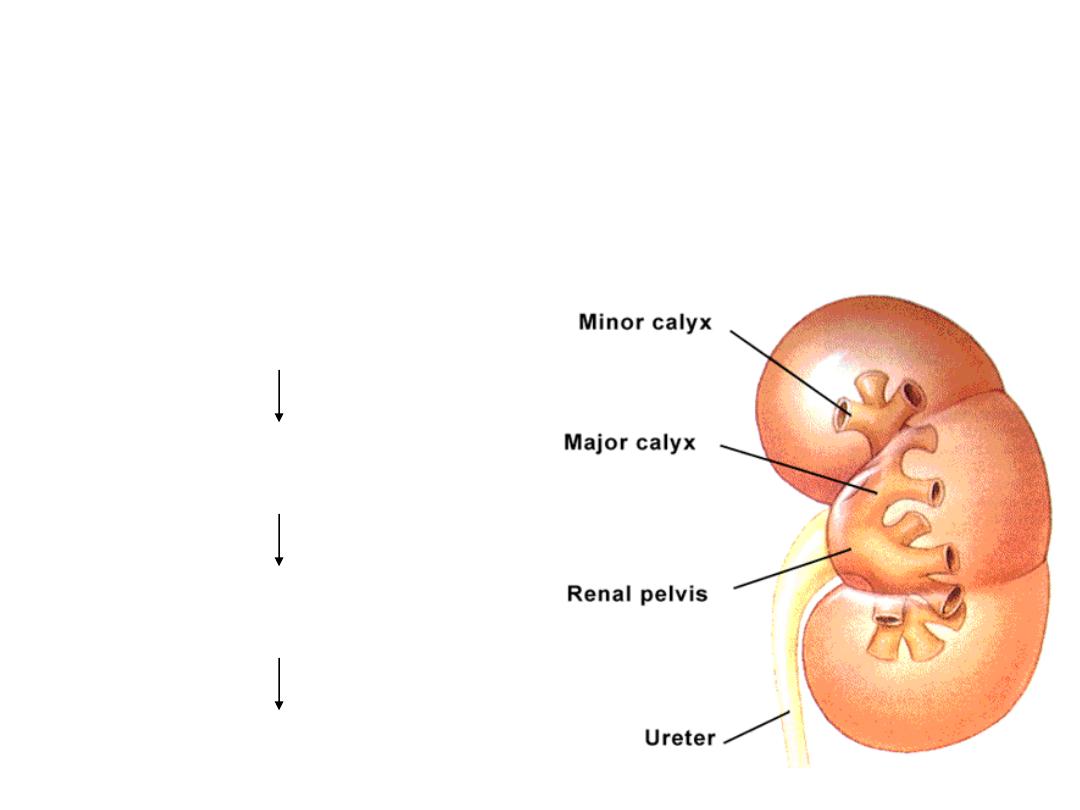
Urine collection:
Ducts within each renal
papilla release urine
into minor calyx
major calyx
renal pelvis
ureter
56

Histological structure
1-Mucosa:
a- Epithelium:
transitional.
b- Lamina propria:
loose C.T.
2-Muscle layer:
Smooth muscle that becomes
thicker from minor
calyces to renal pelvis .
3-Adventitia:
CT covering urinary passage except
upper part of urinary bladder (peritoneum
.
(
57
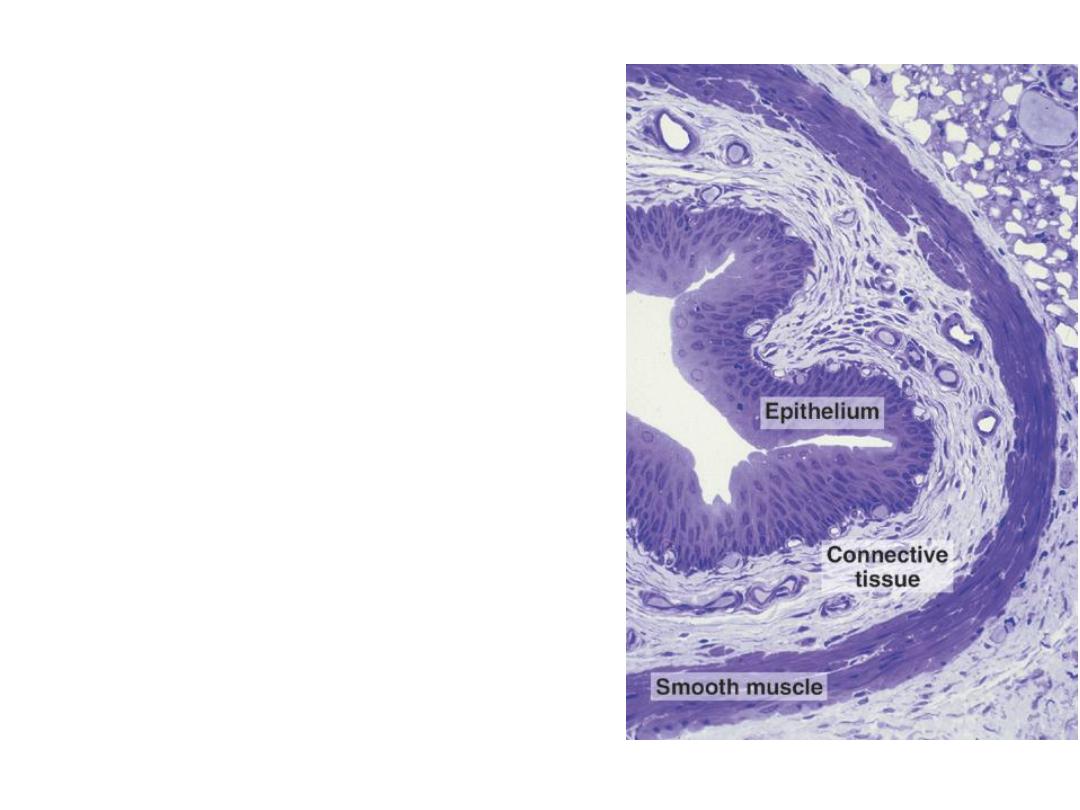
URETER
• 2 ureters
• Starts from renal pelvis.
• Ends in urinary bladder.
• 4 mm in diameter &
30 cm long
.
• Thin wall +
star shaped lumen.
58
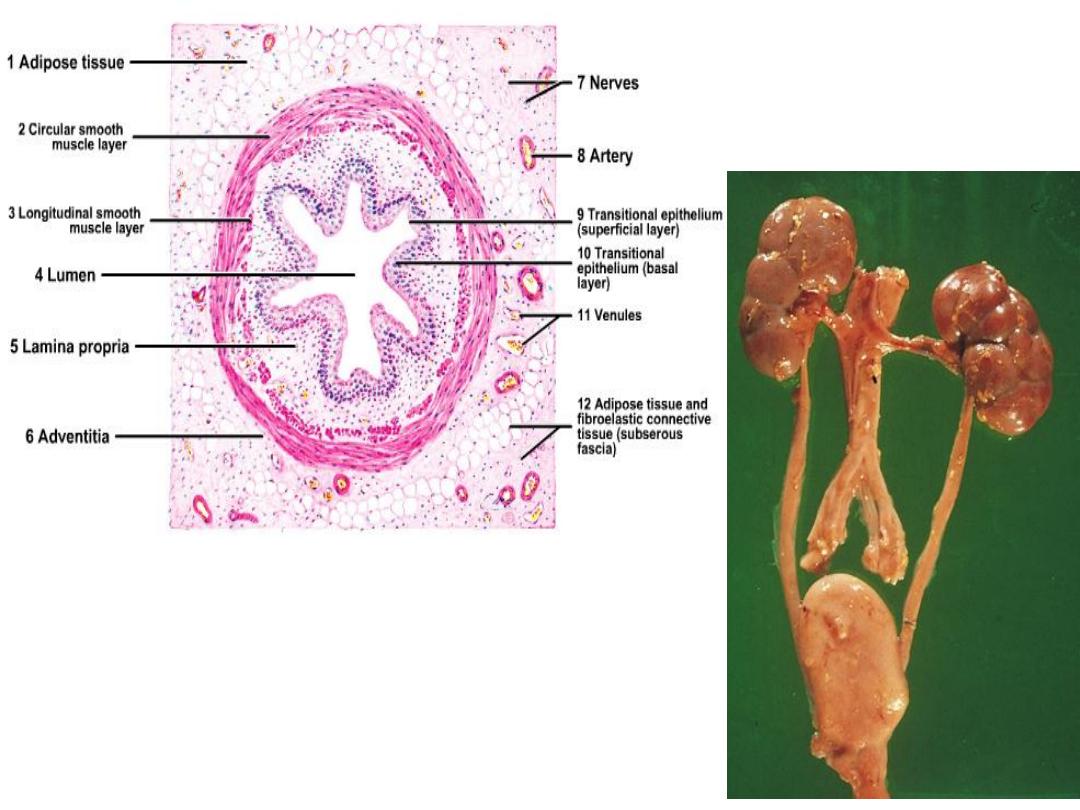
59

Histological structure
1- Mucosa:
longitudinal folds
a- Epithelium:
transitional.
b- Lamina propria:
dense CT, BV and lymphatic nodules.
2- Muscle layer:
smooth muscles
a-
In upper two thirds:
2 layers, inner longitudinal
&
outer
circular
.
b
- In lower third:
3 layers, inner & outer longitudinal &
middle circular.
3- Adventitia
:
C.T.
60
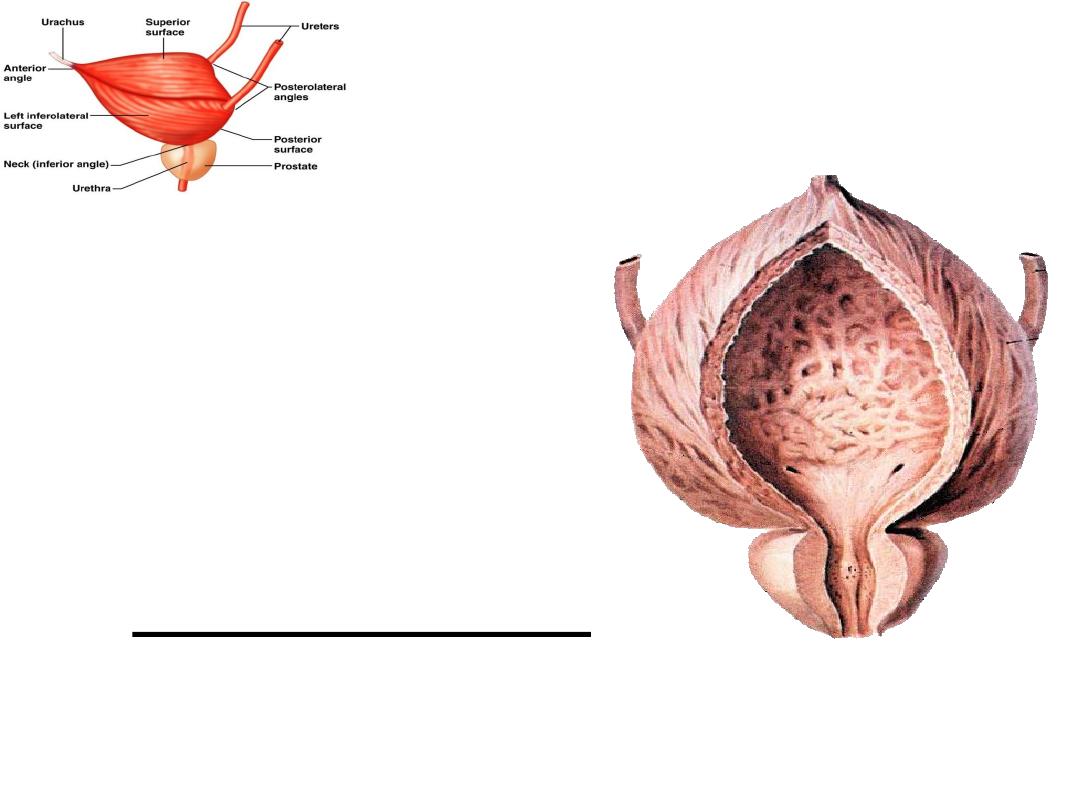
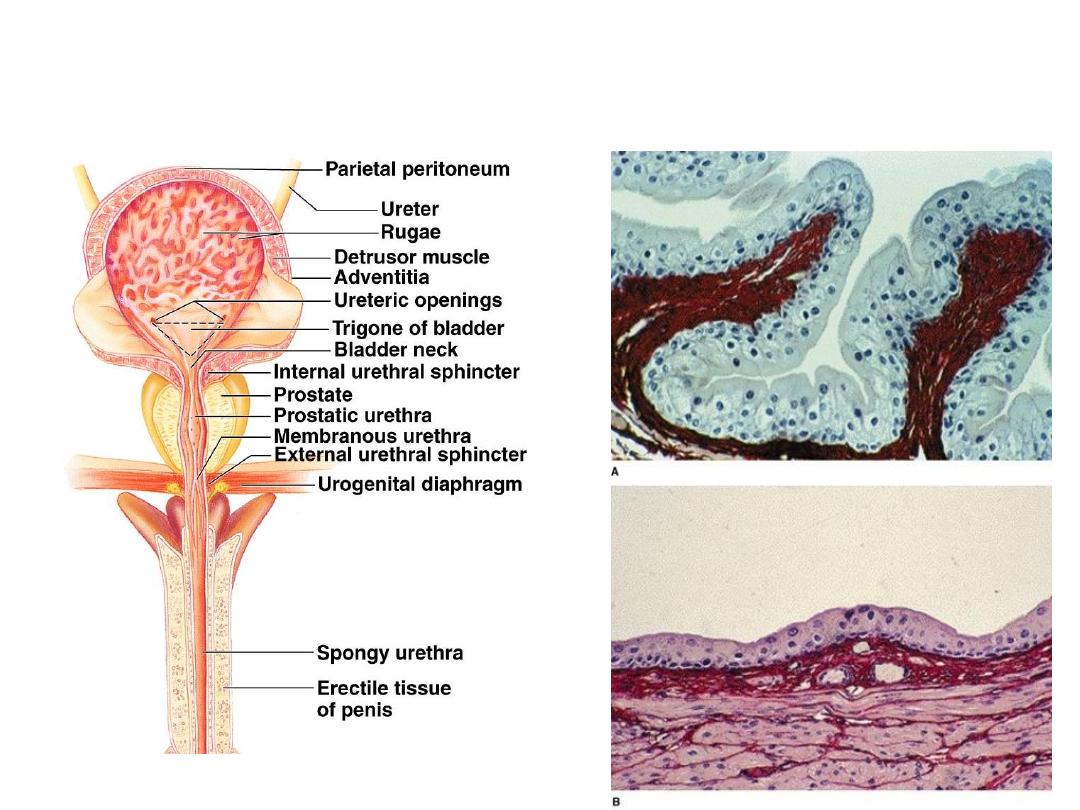
URINARY BLADDER
• a temporary storage
reservoir for urine.
• Thick wall with wide lumen.
• It is located in the pelvic
cavity, posterior to the
symphysis pubis, and below
the parietal peritoneum.
• Empty (Folded).
• Full (Folds disappear).
61
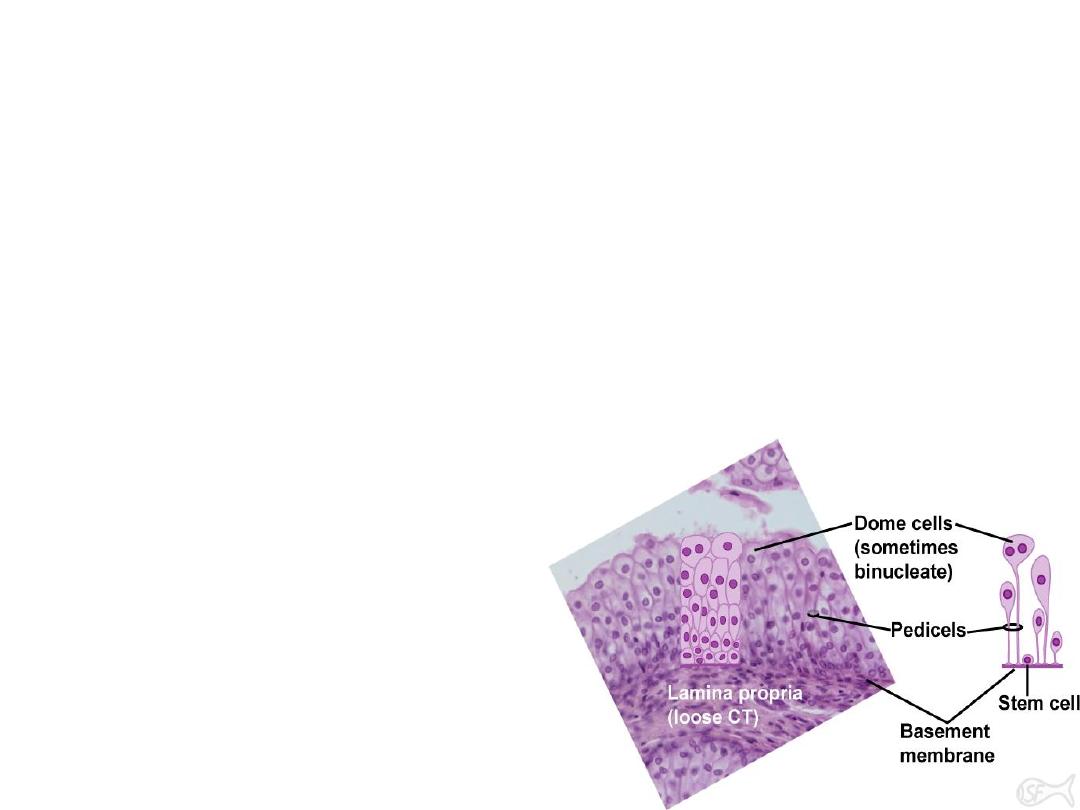
Histological structure
1-Mucosa
:
A-Epithelium
:
transitional
.
• Special stratified epithelium where numbers of layers change according
to state of organ.
• Surface cells are large rounded (dome-shaped) with 1-2 nuclei.
•
In empty bladder
(epithelium has 6-8 layers).
•
In distended bladder
(epithelium has 2-3 layers).
• The surface epithelial layer has thick plasmalemma.
• Cells are attached together by
interdigitation called plaques allowing
cells to overlap each other when bladder
is empty.
B-Lamina propria:
loose to dense C.T.
62
Empty bladder
Full bladder
Empty (Folded).
Full (Folds disappear
).
63

transitional epith.
smooth muscle bundles
serosa
lamina properia
• 2-Muscular layer:
• Thick smooth muscle fibers.
• inner & outer longitudinal. middle
circular
. collectively these are
called the detrusor muscle.
• Contraction of this muscle expels
urine from the bladder.
• 3-Adventitia:
C.T.
• The superior & posterior surface of
the bladder covered by peritoneum
64

URETHRA
• Urethra of female differs from male in
structure and length.
Urethra of female
• 5 cm in length.
• Extends from internal orifice at urinary
bladder
• To external orifice above & anterior to vagina.
65

Histological structure
1-Mucosa
:
a) Epithelium
:
•
Transitional at internal orifice.
•
Stratified squamous at external orifice.
•
Stratified columnar inbetween.
a) Lamina propria:
fibroelastic along its length
.
2-Muscle layer:
smooth muscle
•
Inner longitudinal.
•
Outer circular.
•
As urethra pierces uro-genital diaphragm, skeletal muscle
forms sphincter for voluntary control of micturition
.
66

Urethra of male
• 20 cm tube
• Conducts urine
from urinary bladder &
seminal fluid
from male genitalia to outside body
.
• Many
glands
open in course of male urethra.
These are prostate, bulbo-urethral and littre glands.
• Three parts:
prostatic, membranous & penile
.
67

1- Prostatic urethra
• Present within prostate.
• Lined by transitional epithelium.
• An elevation (verumontanum) projects into its
interior.
• Ejaculatory ducts open at sides of this elevation.
68

2- Membranous urethra
• 1 cm
• Lined by stratified and pseudostratified
columnar epithelium.
• Surrounded by the voluntary external
sphincter.
69

3- Penile urethra
Two portions
:
a) Bulbous
:
– Passes through corpus spongiosum.
– Lined by pseudostratified or stratified
columnar epithelium.
b) Pendulous:
– Passes through glans penis.
– Lined by stratified squamous epithelium.
70

71
71
