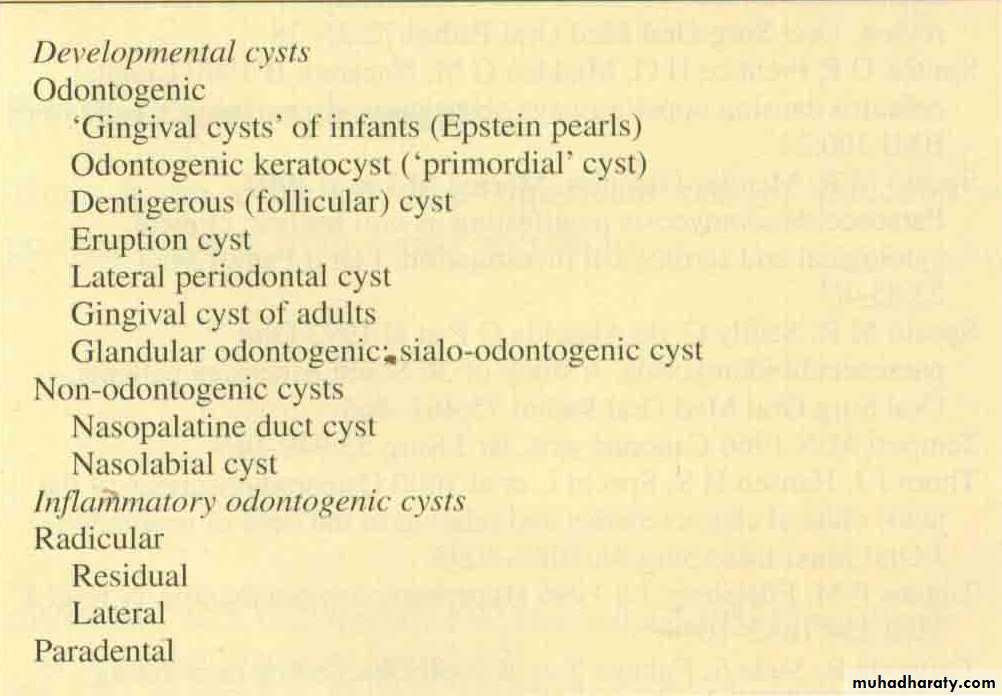
Odontogenic cyst
Introduction
Cysts : are pathological cavities filled with fluid or semi-fluid contents lined by epitheliumOdontogenic cysts (OC) are cysts whose epithelial lining is derived from the remnants of the tooth-forming Organ.
OC derived from one of the following tissue
Rests of Malassez (rests of the root sheath of Hertwig)glands of Serres (rests of the dental lamina)
reduced enamel epithelium (remnants of the enamel organ).Slowly grwoing show no major or threaten effect on patient life
However, they may cause bone or tooth resorption, bone expansion, fracture or tooth migration.
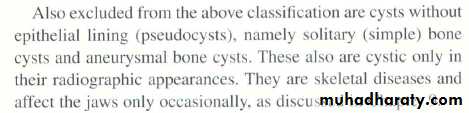
D.D of cyst like areas of radiolucency
1- anatomical structures2- psuedocyst
3- neoplasm like ameloplastoma
4- giant cell granuloma of the jaw
5- hyperparathyrodism
6- cherubism
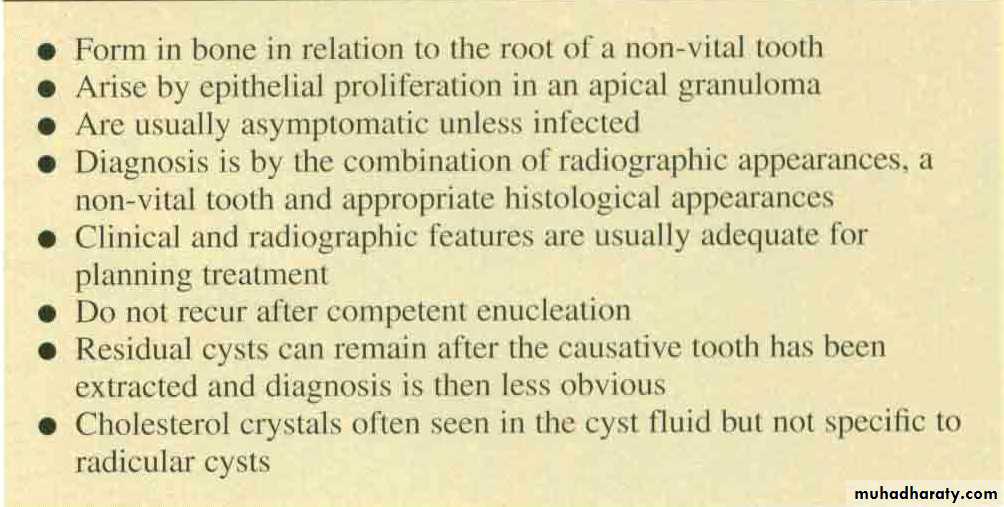
Radicular cyst
Radicular cysts originate from proliferation of epithelial residues. These epithelial cells re-main quiescent throughout life, however, cell mediators and signalling molecules releasedduring an inflammatory process may trigger their proliferation
CLINICAL PICTURE
RADICULAR CYST
Pathogenesis and Pathology
The most common factors responsible for cyst development are1- Proliferation of epithelial lining and fibrous capsule
2- Hydrostatic pressure of cyst fluid3- Resorption of surrounding bone
Proliferation of epithelial lining and fibrous capsule
infection of the pulp chamber can induce proliferation of epithelial rest of Malazess. The epithelial proliferation (hyperplasia) within a periapical granuloma may reach a critical size at which the diffusion of nutrients within the epithelial mass cannot keep pace with the metabolic utilisation of the nutrients that diffuse from the surrounding stroma.The lack of nutrients results in degeneration and death of the central cells in the proliferating mass with subsequent liquefaction which results in a new cavity in the epithelial mass. However epithelial cells closer to the stroma remain vital.
Hydrostatic effect of cyst fluid
The degradation of the central cells in the cyst results in an increased osmotic pressure in comparison to the osmotic pressure of the surrounding stroma.
This gradient draws water into the cavity (to balance the osmotic pressure), resulting in an increase in hydrostatic pressure inside the cyst in comparison to the stroma
The volume expansion stretches the epithelial layer inducing division of the epithelial cells in order to maintain the intact epithelial lining.
The surrounding stroma reacts by producing varying amounts of collagen fibres and reorganising them into the so-called cystic capsule.
Bone resorbing factors
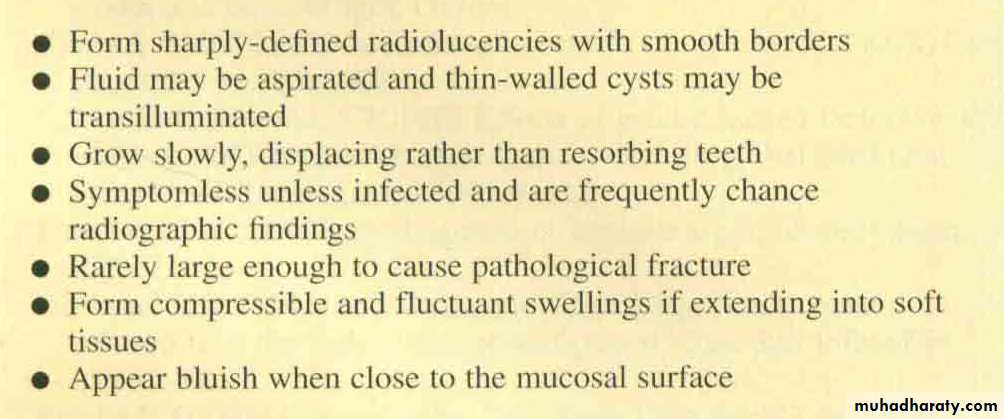
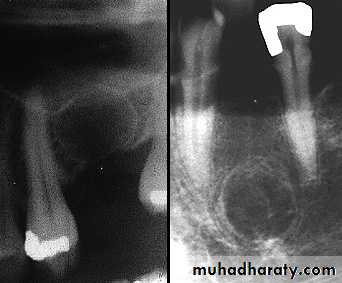
Radiography
RADIOGRAPHICAL FEATURE
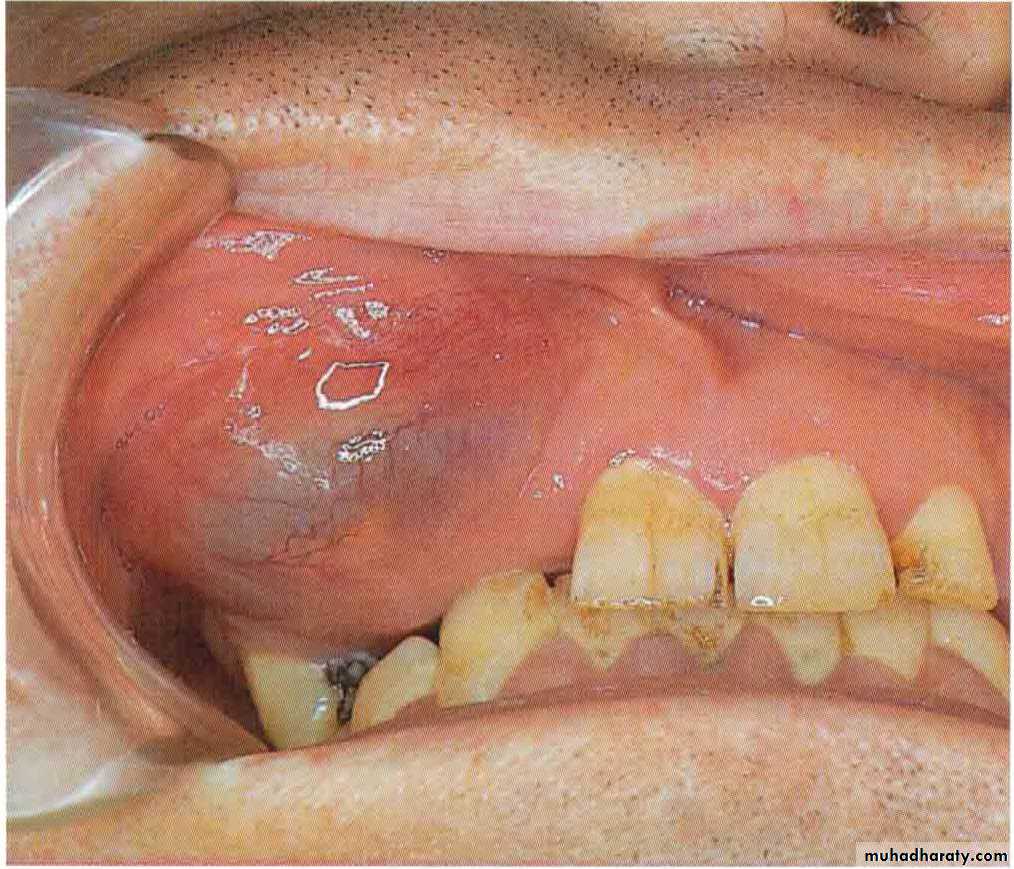
Residual and lateral radicular cyst
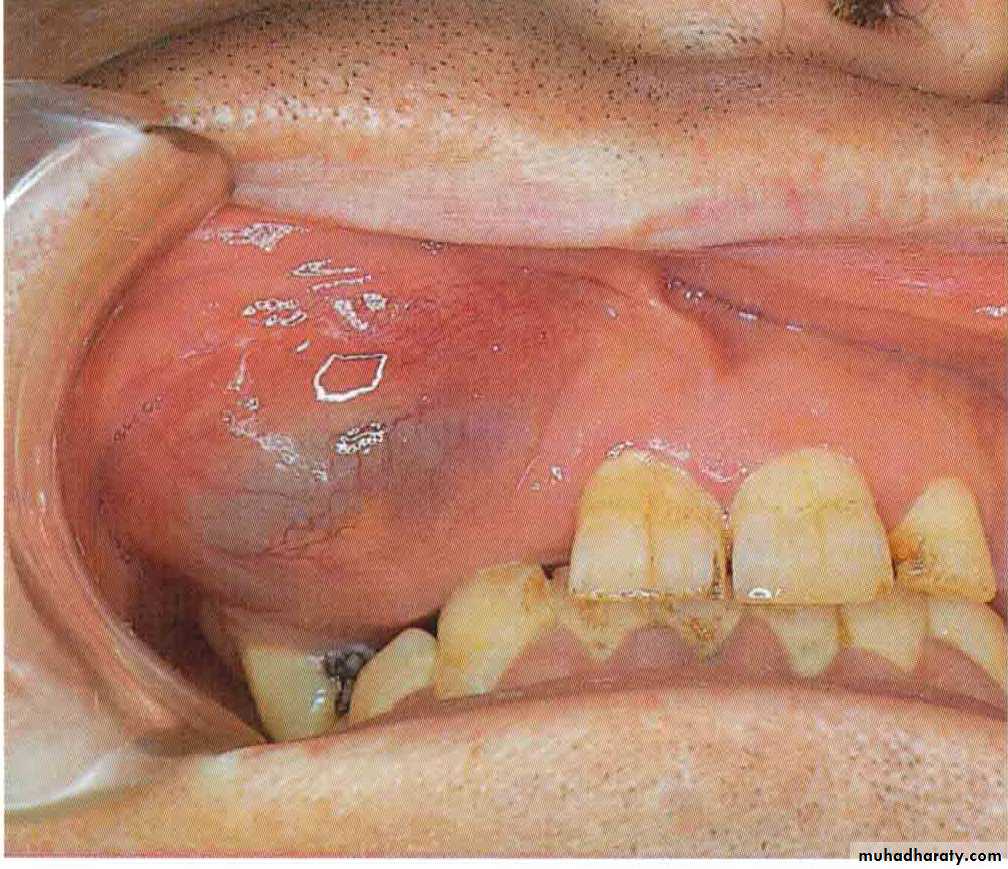
A radicular cyst may persist after extraction of the causative tooth.Residual cysts are the most common cause of swelling of the edentulous jaw in older person.
Can interfere with the fit of the dentures, but may slowly regress spontaneously
Residual Cyst
Residual and lateral radicular cyst
Lateral radicular cysts can occasionally form at the side of non vital tooth as a result of the opening of a lateral branch of the root canal.They are rare and must be distinguished from lateral periodontal cysts which are another pathological entity.
Lateral periodontal cyst
These un common intraosseous cysts are developmental and form beside a vital tooth.They are usually seen by chance in routine radiograph.
Resemble other OC radiographically, apart from its position near the crest of the ridge.
Cause no symptoms but can erode through the bone to extend in to the gingiva.
Respond to enucleation.
The related tooth can be retained if healthy