Disorders of water and electrolytes imbalance
Abdullah AlyouzbakiLecturer of Medicine/Mosul Medical College
Gastroenterologist and hepatologist
1
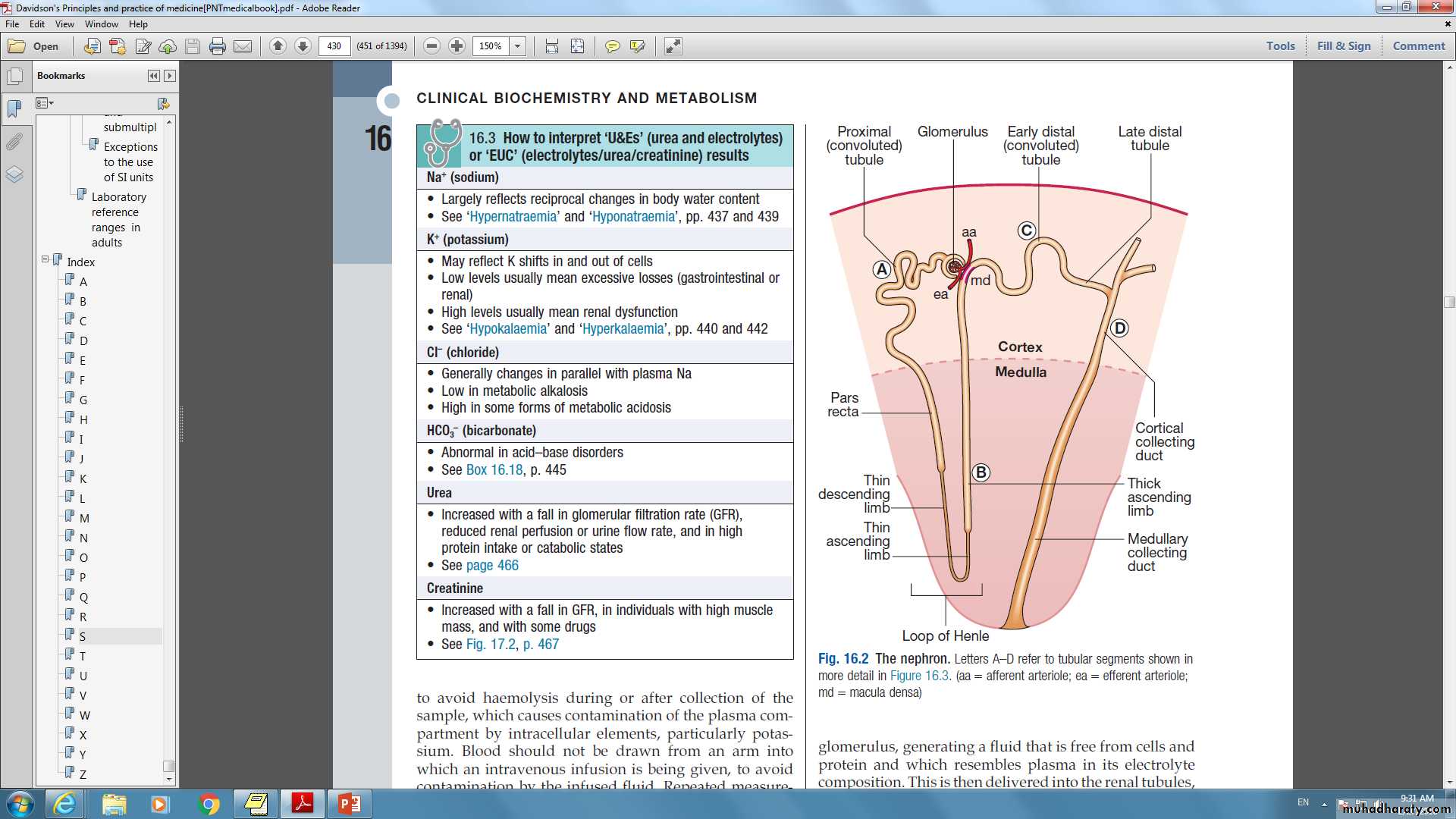
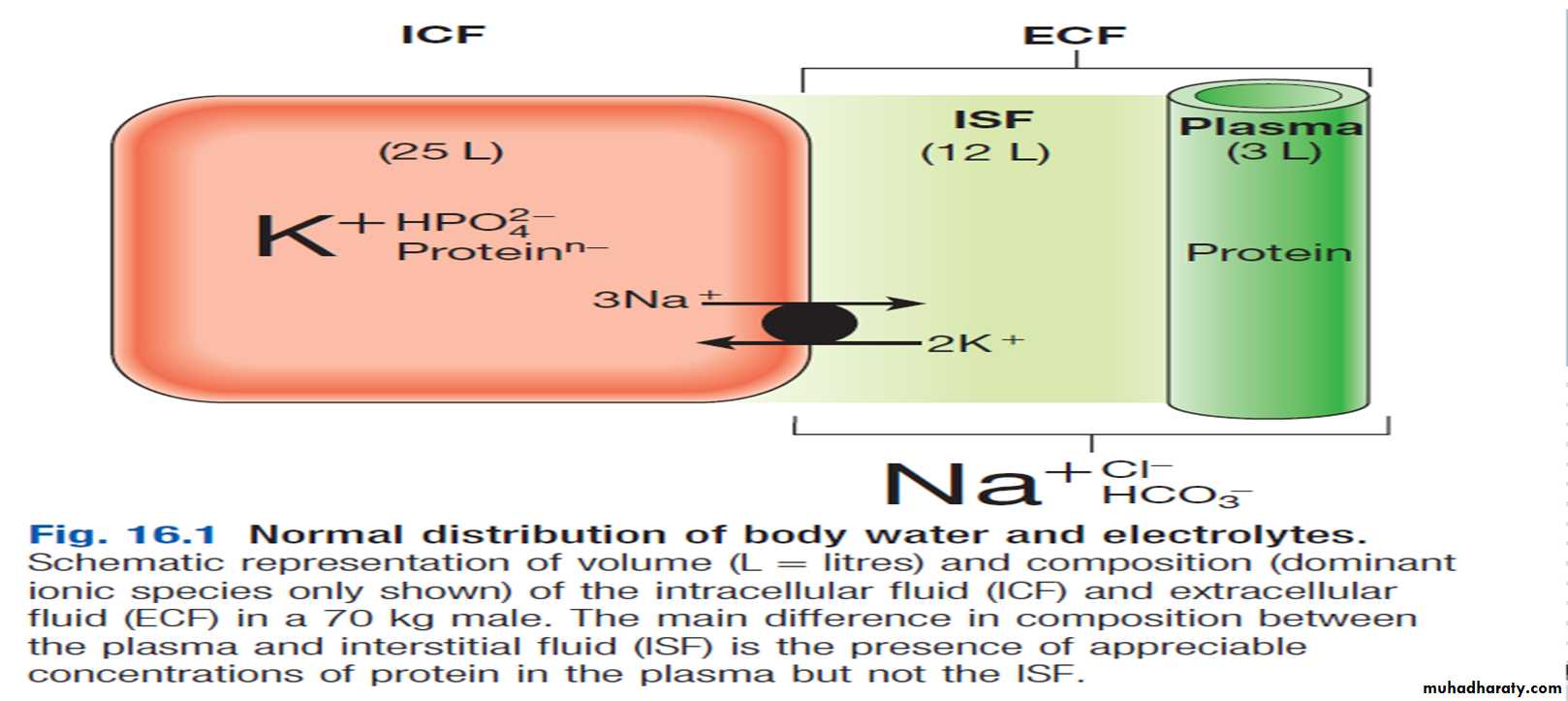
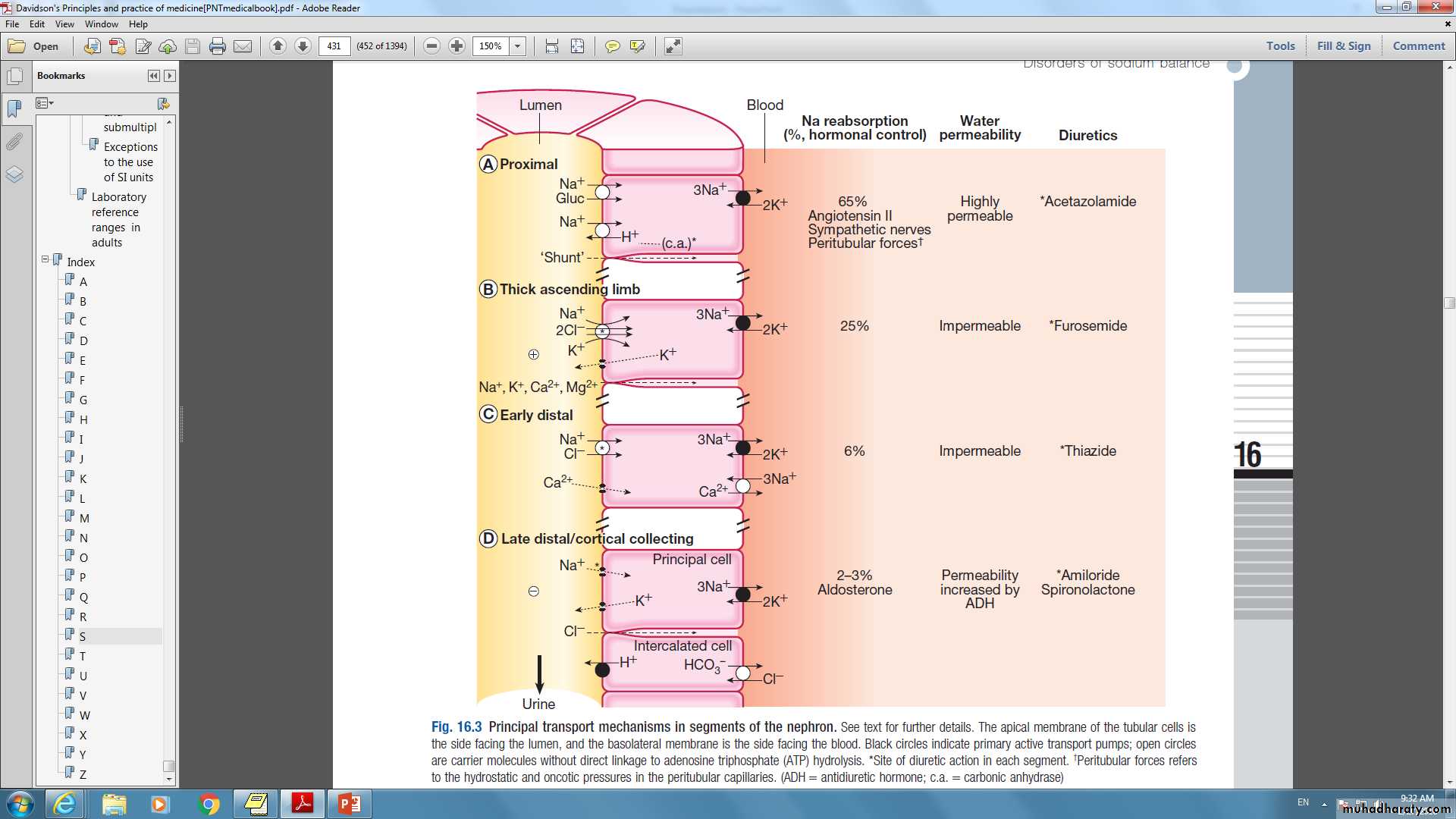
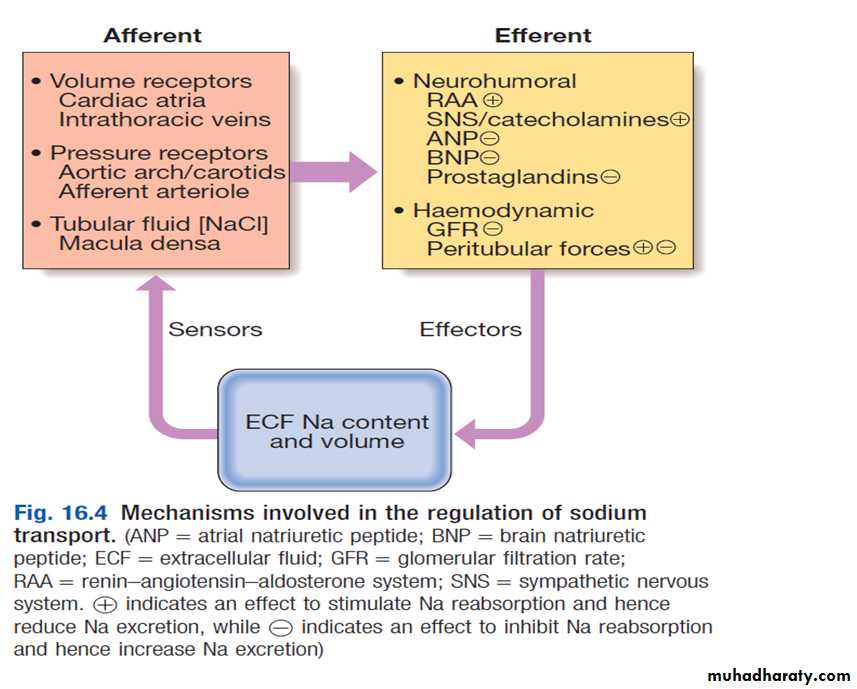
Functional anatomy and physiology ofrenal sodium handling
2
Functional anatomy and physiology ofrenal water and sodium handling
3
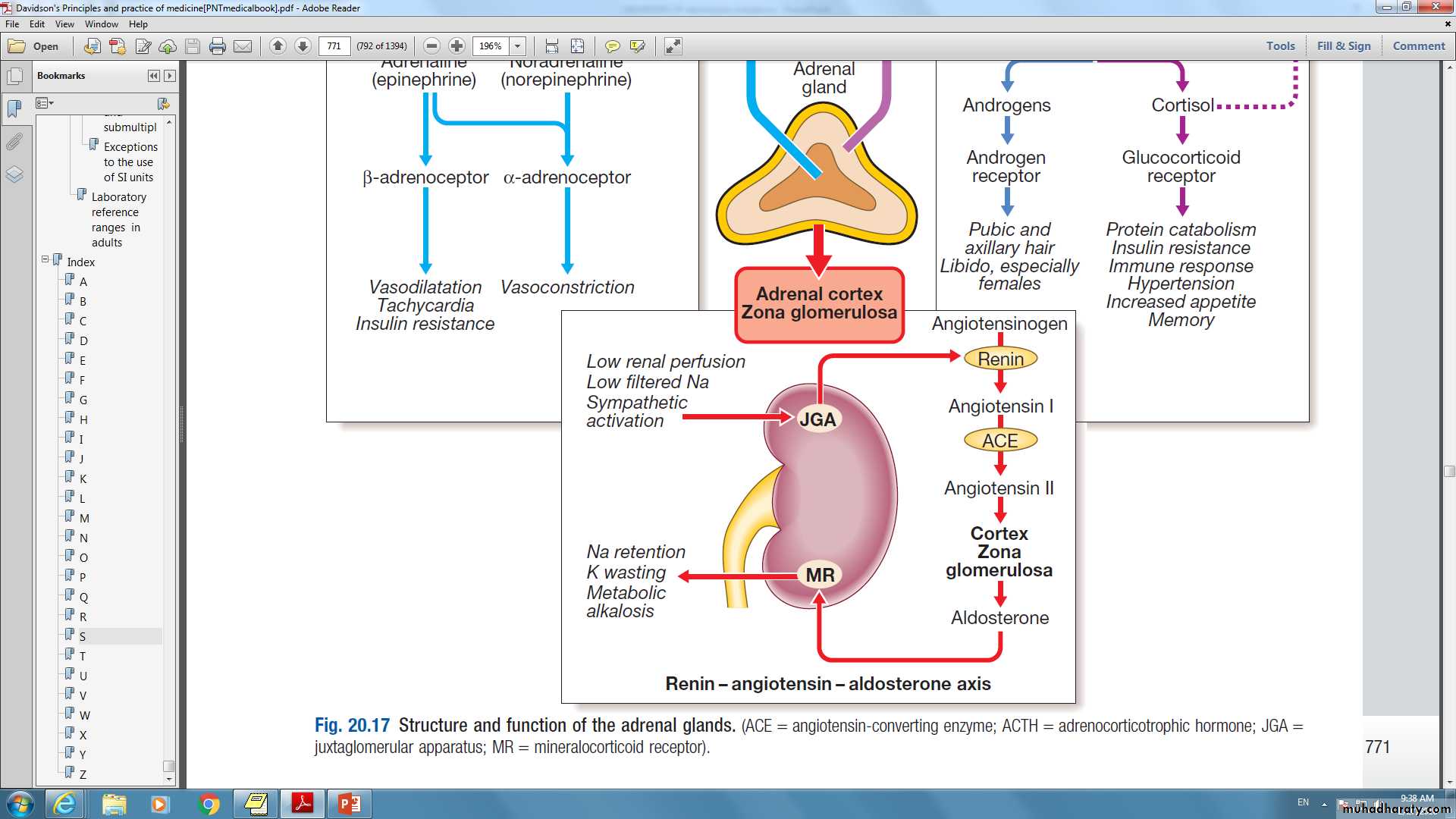
(ACE = angiotensin-converting enzyme; ACTH = adrenocorticotrophic hormone; JGA = juxtaglomerular apparatus; MR = mineralocorticoid receptor).
4
Presenting problems in disorders of water and sodium balance
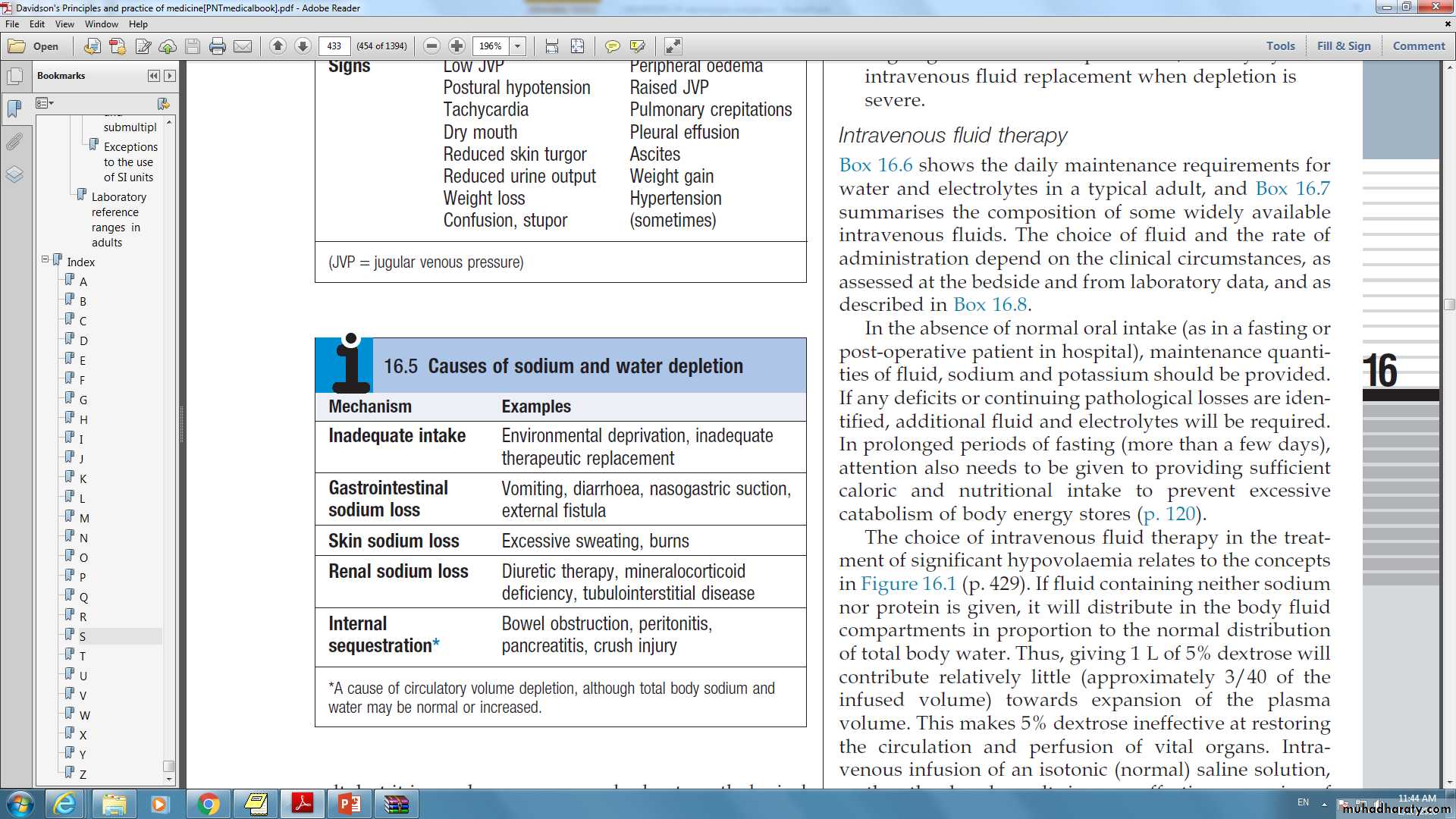
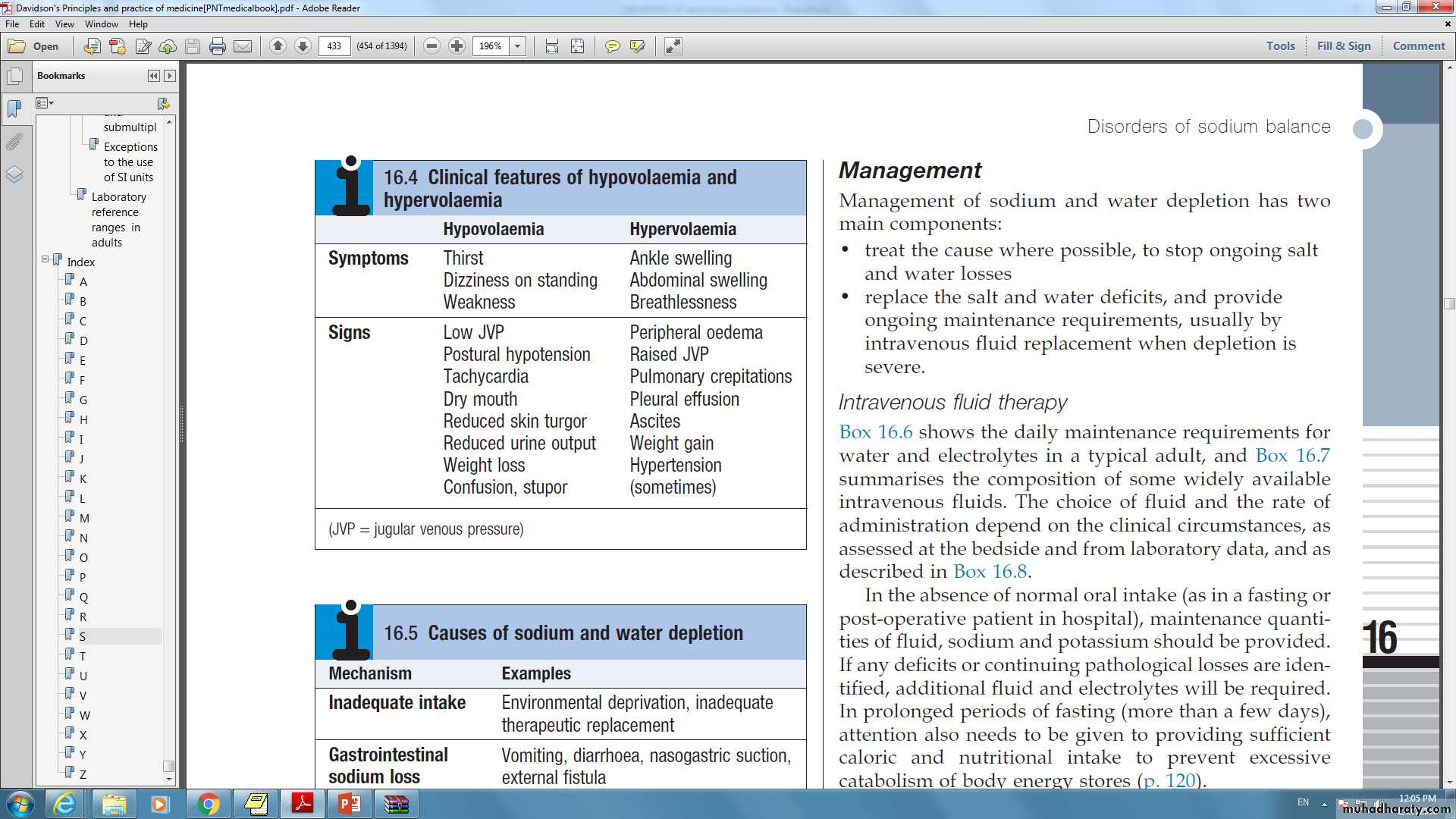
Sodium depletion:Aetiology and clinical assessment
5
Presenting problems in disorders of water and sodium balance
6
Sodium and water depletion
Supportive evidence may be obtained from the clinical biochemistry laboratory. Although plasma sodium concentration may not be reduced if salt and water are lost in equal proportions, a number of other parameters are altered during appropriate renal, hormonal and hemodynamic responses to hypovolemia.
plasma creatinine, which reflects GFR, may be relatively normal, but the plasma urea concentration is typically elevated, since urea excretion is affected by both GFR and urine flow rate.
Plasma uric acid may also rise, reflecting activation of compensatory proximal tubular reabsorption.
With avid retention of sodium and water, the urine osmolality increases while the urine sodium concentration falls.
7
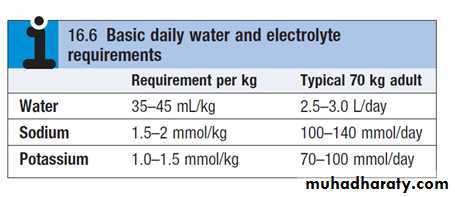
Sodium and water depletion :Management
Management of sodium and water depletion has two main components:• treat the cause where possible, to stop ongoing salt and water losses
• replace the salt and water deficits, and provide ongoing maintenance requirements, usually by intravenous fluid replacement when depletion is severe.
8
9
Sodium and water depletion: Management
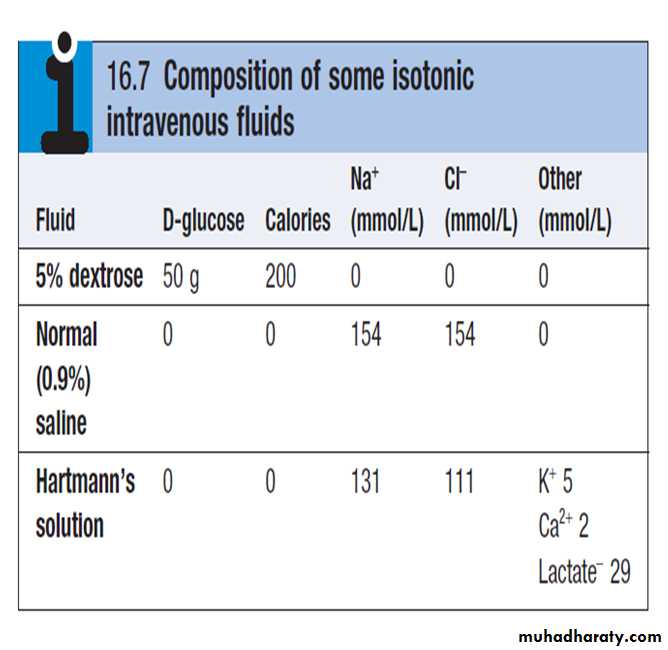
If fluid containing neither sodium nor protein is given, it will distribute in the body fluid compartments in proportion to the normal distribution of total body water. Thus, giving 1 L of 5% dextrose will contribute relatively little (approximately 3/40 of the infused volume) towards expansion of the plasma volume. This makes 5% dextrose ineffective at restoring the circulation and perfusion of vital organs.10
Sodium and water depletion: Management
Intravenous infusion of an isotonic (normal) saline solution, on the other hand, results in more effective expansion of the extracellular fluid, although a minority of the infused volume (some 3/15) will contribute to plasma volume.
Resuscitation fluids containing albumin or synthetic colloids such as carbohydrate polymers should not be used in the acute resuscitation of volume-depleted patients since they offer no benefit over crystalloids and are associated with increased mortality.
11
Sodium excess : Aetiology and clinical assessment
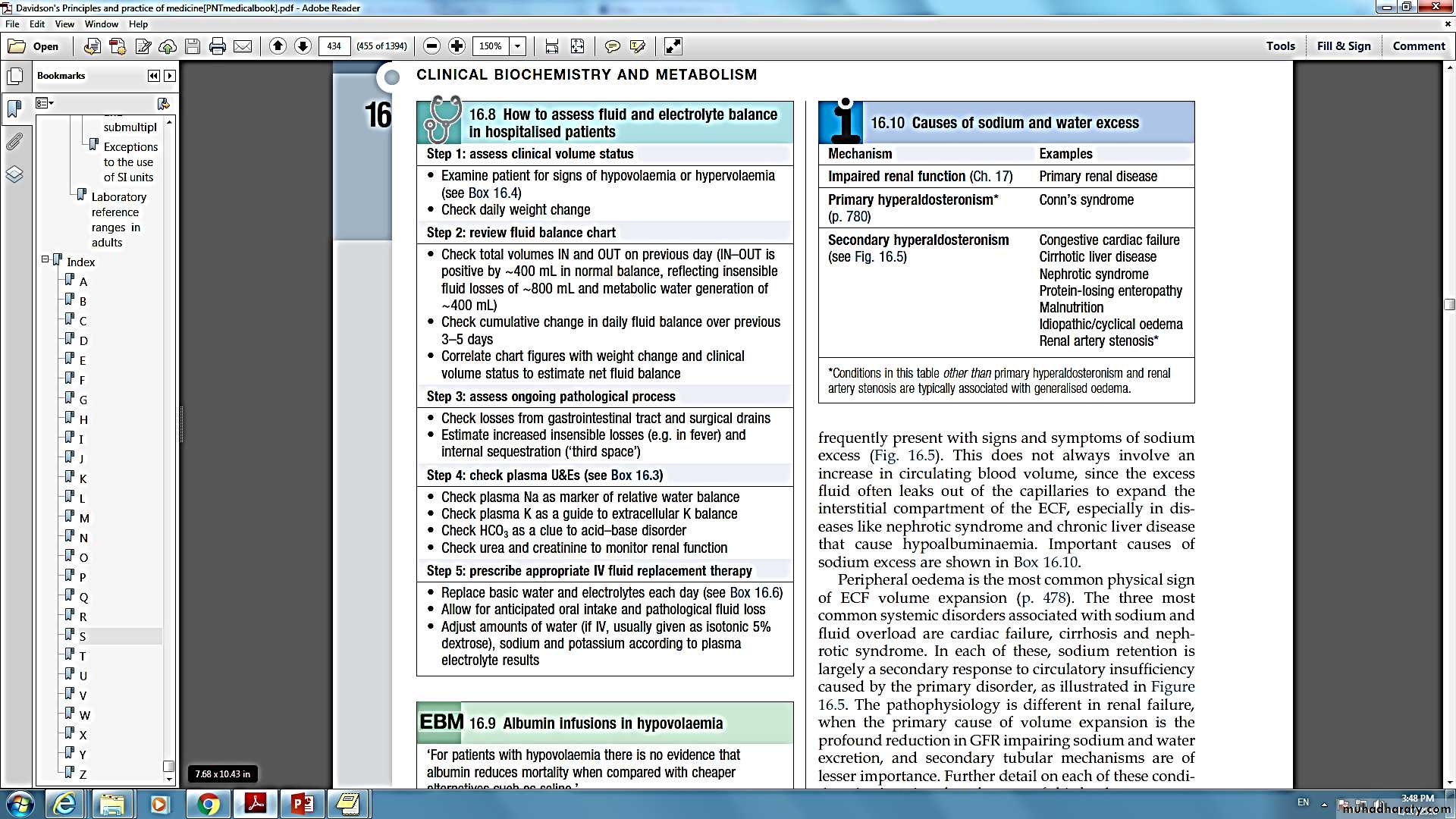
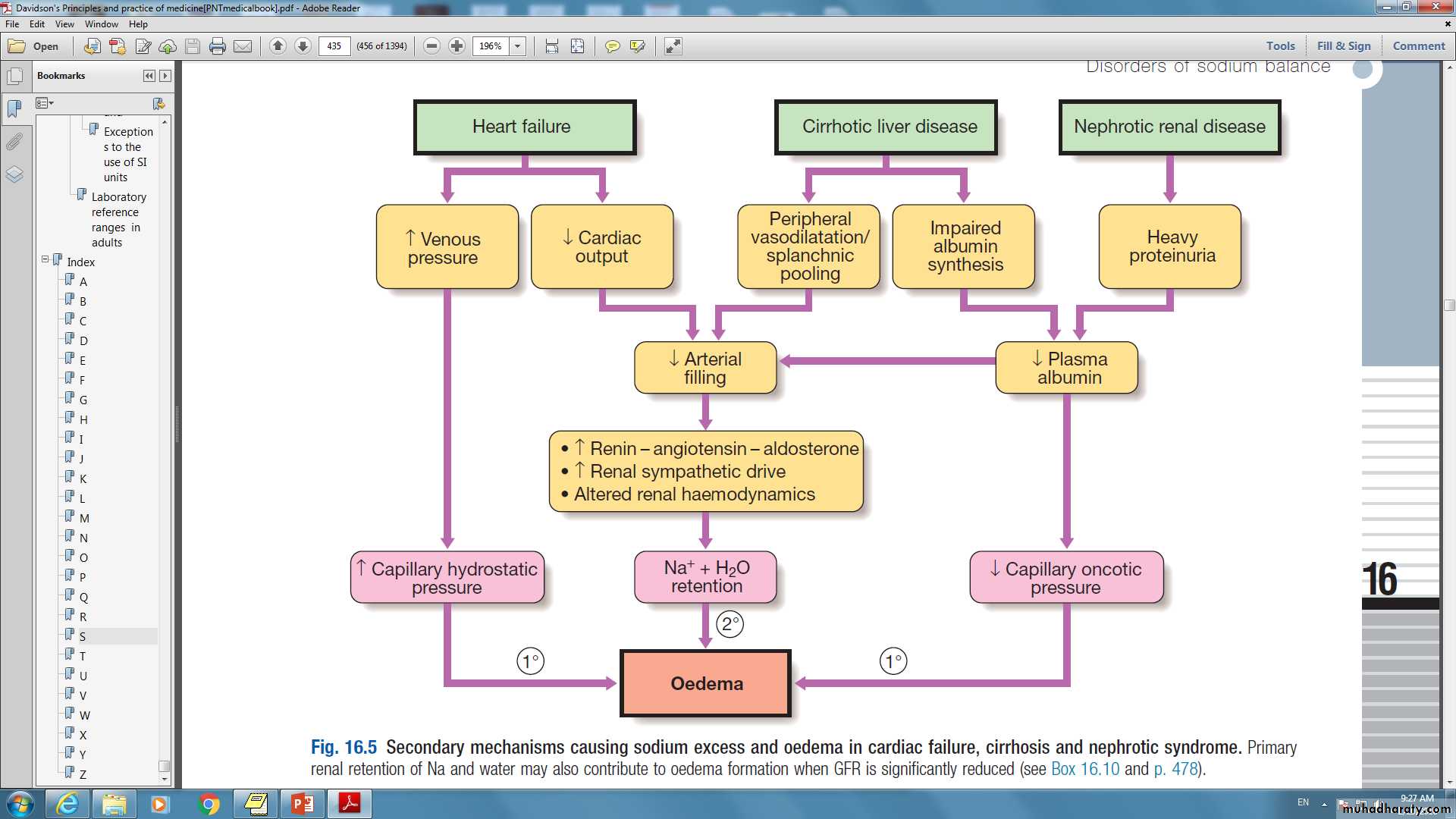
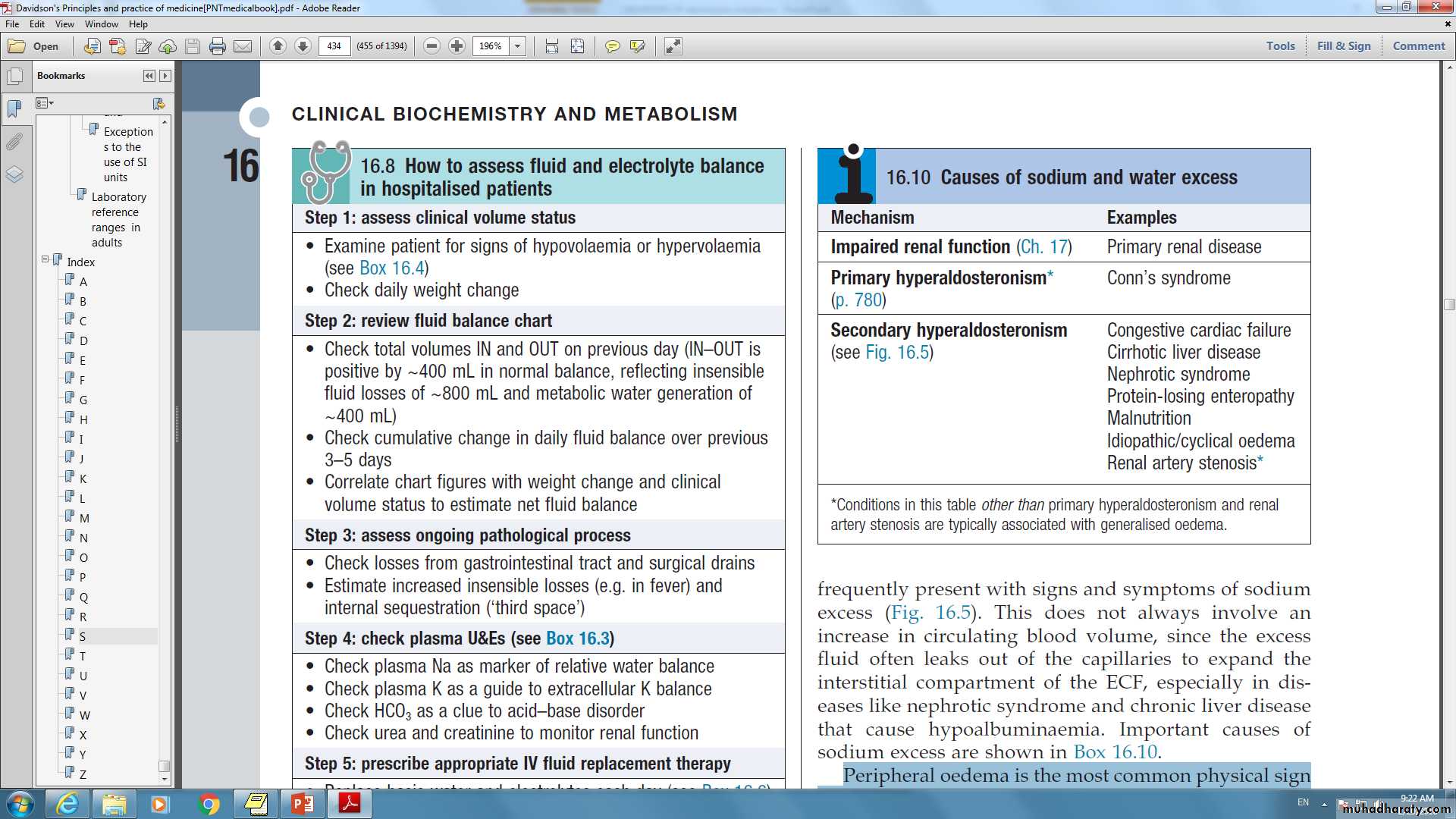
In patients with normal cardiac and renal function, excessive intakes of salt and water are compensated for by increased excretion and do not lead to clinically obvious features of sodium and water overload.However, patients with cardiac, renal or hepatic disease frequently present with signs and symptoms of sodium excess.
Peripheral edema is the most common physical sign of ECF volume expansion.
The three most common systemic disorders associated with sodium and fluid overload are cardiac failure, cirrhosis and nephrotic syndrome.
12
13
The management of ECF volume overload
Involves a number of components:
• specific treatment directed at the underlying cause.• restriction of dietary sodium (to 50–80 mmol/day) to match the diminished excretory capacity
• treatment with diuretics.
14
Hyponatremia :Aetiology and clinical assessment
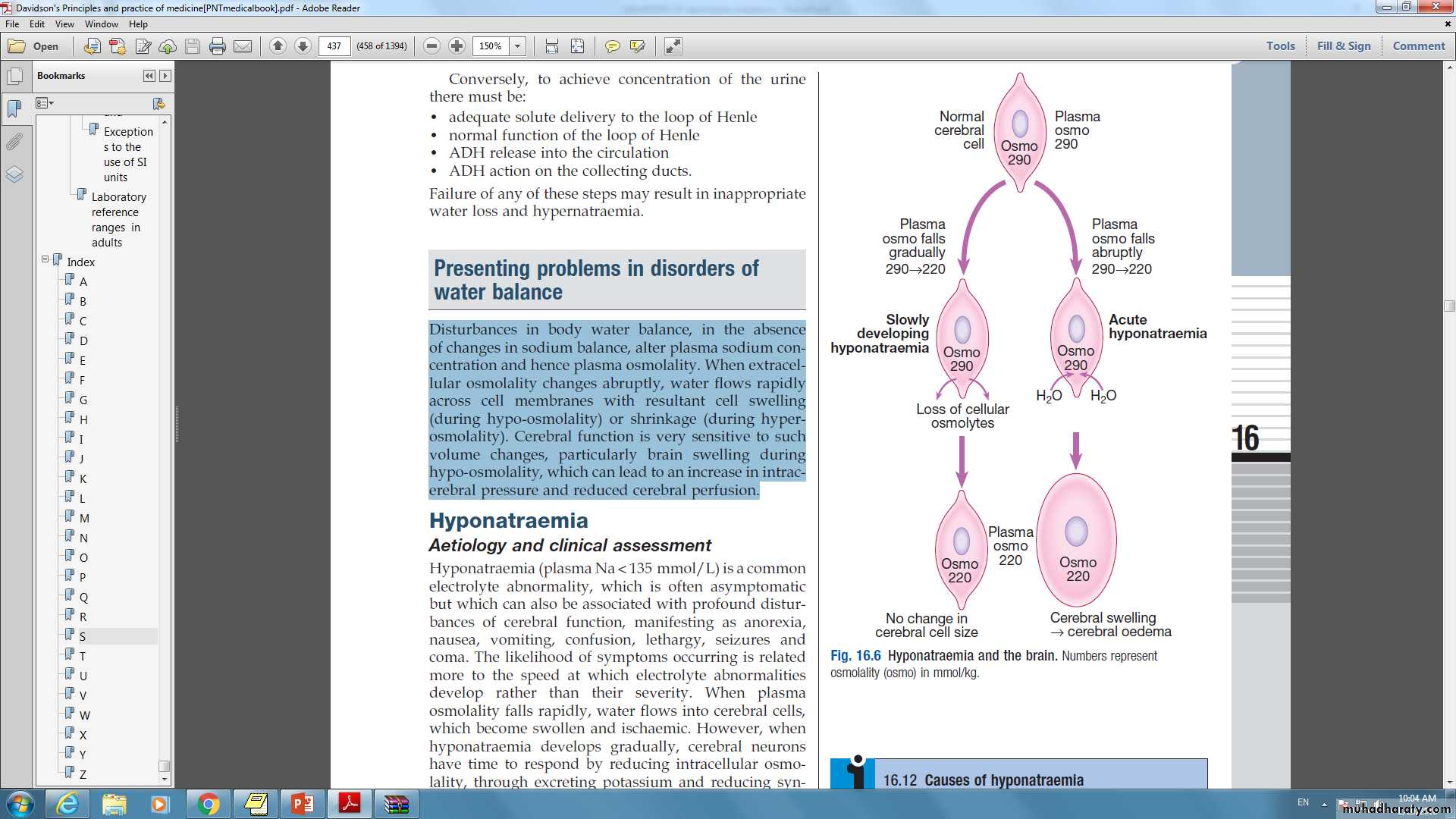
Hyponatremia (plasma Na < 135 mmol/L) is a common electrolyte abnormality, which is often asymptomatic but which can also be associated with profound disturbances of cerebral function, manifesting as anorexia, nausea, vomiting, confusion, lethargy, seizures and coma.
The likelihood of symptoms occurring is related more to the speed at which electrolyte abnormalities develop rather than their severity.
15
Hyponatremia :Aetiology and clinical assessment
16
Hyponatremia :Aetiology and clinical assessment
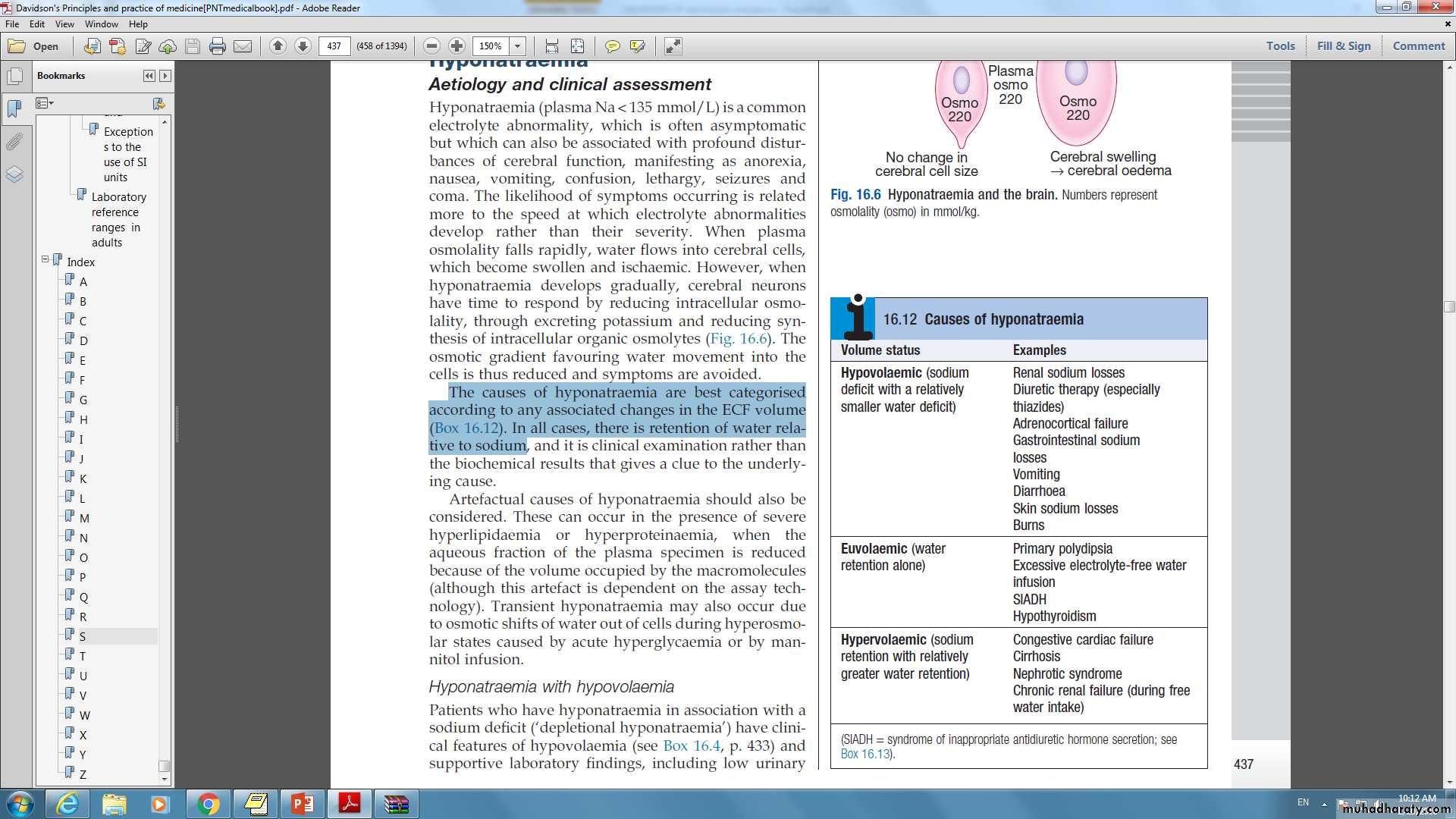
The causes of hyponatremia are best categorized according to any associated changes in the ECF volume. In all cases, there is retention of water relative to sodium.Artefactual hyponatremia occur in the presence of severe hyperlipidemia or hyperproteinemia, when the aqueous fraction of the plasma specimen is reduced because of the volume occupied by the macromolecules.
17
Hyponatremia with hypovolemia
Patients who have hyponatremia in association with a sodium deficit have clinical features of hypovolemia and supportive laboratory findings, including low urinary sodium concentration (< 30 mmol/L) and elevated plasma renin activity.18
Hyponatremia with euvolemia
Water retention also occurs in the syndrome of inappropriate secretion of ADH (SIADH). In this condition, an endogenous source of ADH (either cerebral or tumor-derived) promotes water retention by the kidney in the absence of an appropriate physiological stimulus.
The clinical diagnosis requires the patient to be euvolemic, with no evidence of cardiac, renal or hepatic disease potentially associated with hyponatremia.
Other non-osmotic stimuli that cause release of ADH (pain, stress, nausea) should also be excluded.
19
Syndrome of inappropriate antidiuretichormone secretion (SIADH): causes and diagnosis
Causes:• Tumors
• CNS disorders: stroke, trauma, infection, psychosis, porphyria
• Pulmonary disorders: pneumonia, tuberculosis, obstructive lung disease
• Drugs: anticonvulsants, psychotropics, antidepressants, cytotoxics, oral hypoglycaemic agents, opiates
• Idiopathic
20
Syndrome of inappropriate antidiuretichormone secretion (SIADH): causes and diagnosis
Diagnosis• Low plasma sodium concentration (typically < 130 mmol/L)
• Low plasma osmolality (< 270 mmol/kg)
• Urine osmolality not minimally low (typically > 150 mmol/kg)
• Urine sodium concentration not minimally low (> 30 mmol/L)
• Low-normal plasma urea, creatinine, uric acid
• Exclusion of other causes of hyponatremia
• Appropriate clinical context
21
Hyponatraemia with hypervolaemia
In this situation, excess water retention is associated with sodium retention and volume expansion, as in heart failure, liver disease or kidney disease.
22
Hyponatremia : Management
The treatment of hyponatremia is critically dependent on its rate of development, severity and underlying cause.If hyponatremia has developed rapidly (over hours to days), and there are signs of cerebral edema such as obtundation or convulsions, sodium levels should be restored to normal rapidly by infusion of hypertonic (3%) sodium chloride.
23
Hyponatremia : Management
On the other hand, rapid correction of hyponatremia that has developed slowly (over weeks to months) can be hazardous, since brain cells adapt to slowly developing hypoosmolality by reducing the intracellular osmolality, thus maintaining normal cell volume Under these conditions.An abrupt increase in extracellular osmolality can lead to water shifting out of neurons, abruptly reducing their volume and causing them to detach from their myelin sheaths.
24
Hyponatremia : Management
The resulting ‘myelinolysis’ can produce permanent structural and functional damage to mid-brain structures, and is generally fatal. The rate of correction of the plasma Na concentration in chronic asymptomatic hyponatremia should not exceed 10 mmol/L/day, and an even slower rate is generally safer.The underlying cause should be treated. For hypovolaemic patients, this involves controlling the source of sodium loss, and administering intravenous saline if clinically warranted.
25
Hyponatremia : Management
Patients with dilutional hyponatraemia generally respond to fluid restriction in the range of 600–1000 mL/day, accompanied where possible by withdrawal of the precipitating stimulus (such as drugs causing SIADH).If the response of plasma sodium is inadequate, treatment with deme -clocycline may be of value by enhancing water excretion, through its inhibitory effect on responsiveness to ADH in the collecting duct. An effective oral urea therapy or oral vasopressin receptor antagonists such as tolvaptan.
26
Hyponatremia : Management
Hypervolemia patients with hyponatremia need treatment of the underlying condition, accompanied by cautious use of diuretics in conjunction with strict fluid restriction.
Potassium-sparing diuretics may be particularly useful
27
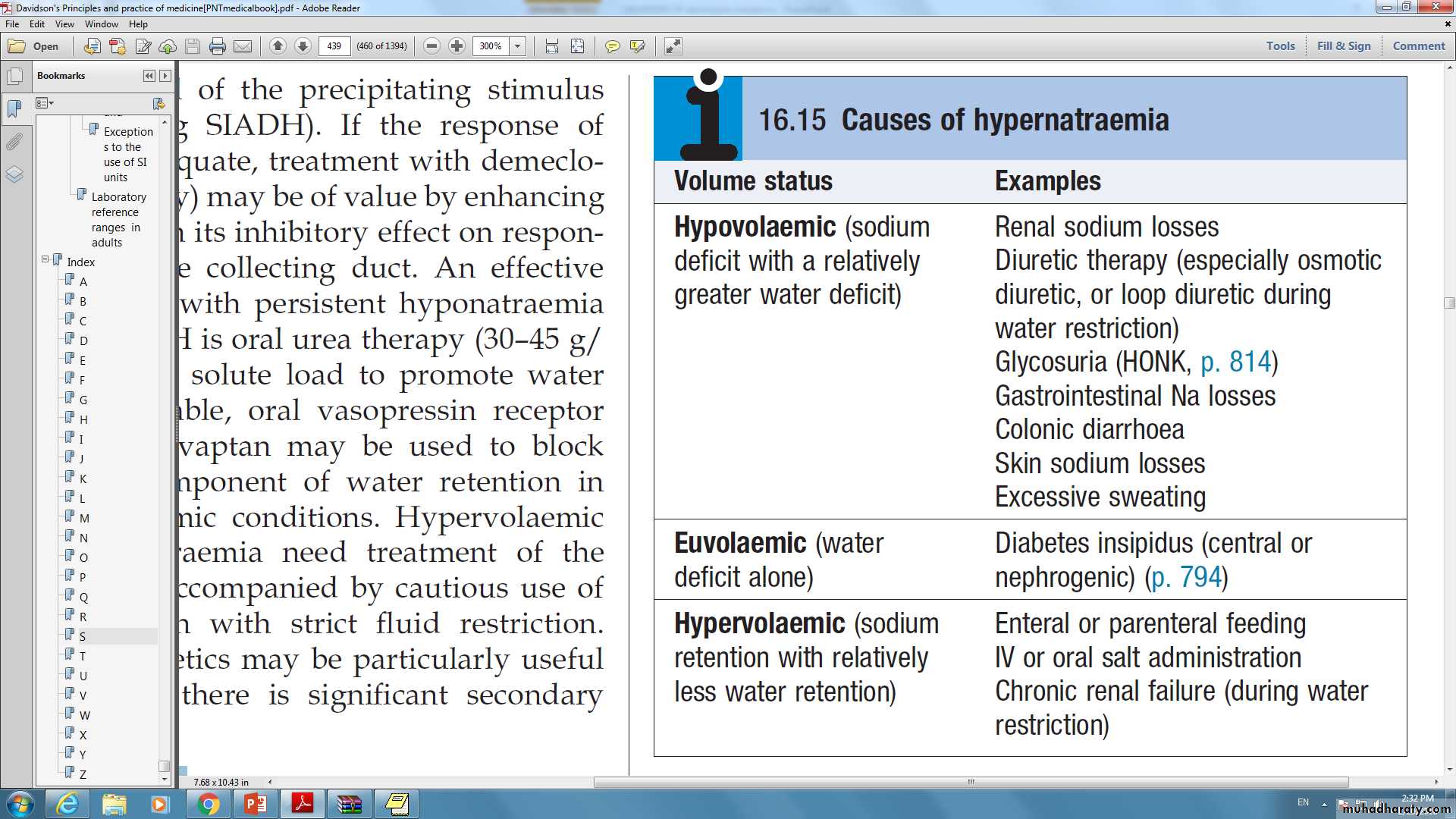
Hypernatremia:Aetiology and clinical assessment
28
Hypernatremia:Aetiology and clinical assessment
In the presence of an intact thirst mechanism and preserved capacity to obtain and ingest water, hypernatremia may not progress very far. If adequate water is not obtained, dizziness, confusion, weakness and ultimately coma and death can result.29
Hypernatremia : Management
Treatment of hypernatremia depends on both the rate of development and the underlying cause. If there is reason to think that the condition has developed rapidly, neuronal shrinkage may be acute and relatively rapid correction may be attempted. This can be achieved by infusing an appropriate volume of intravenous fluid (isotonic 5% dextrose or hypotonic 0.45% saline)If hypernatremia developed slowly, then extreme caution should be exercised in lowering plasma sodium to avoid the risk of cerebral edema.
Where possible, the underlying cause should also be addressed.
30
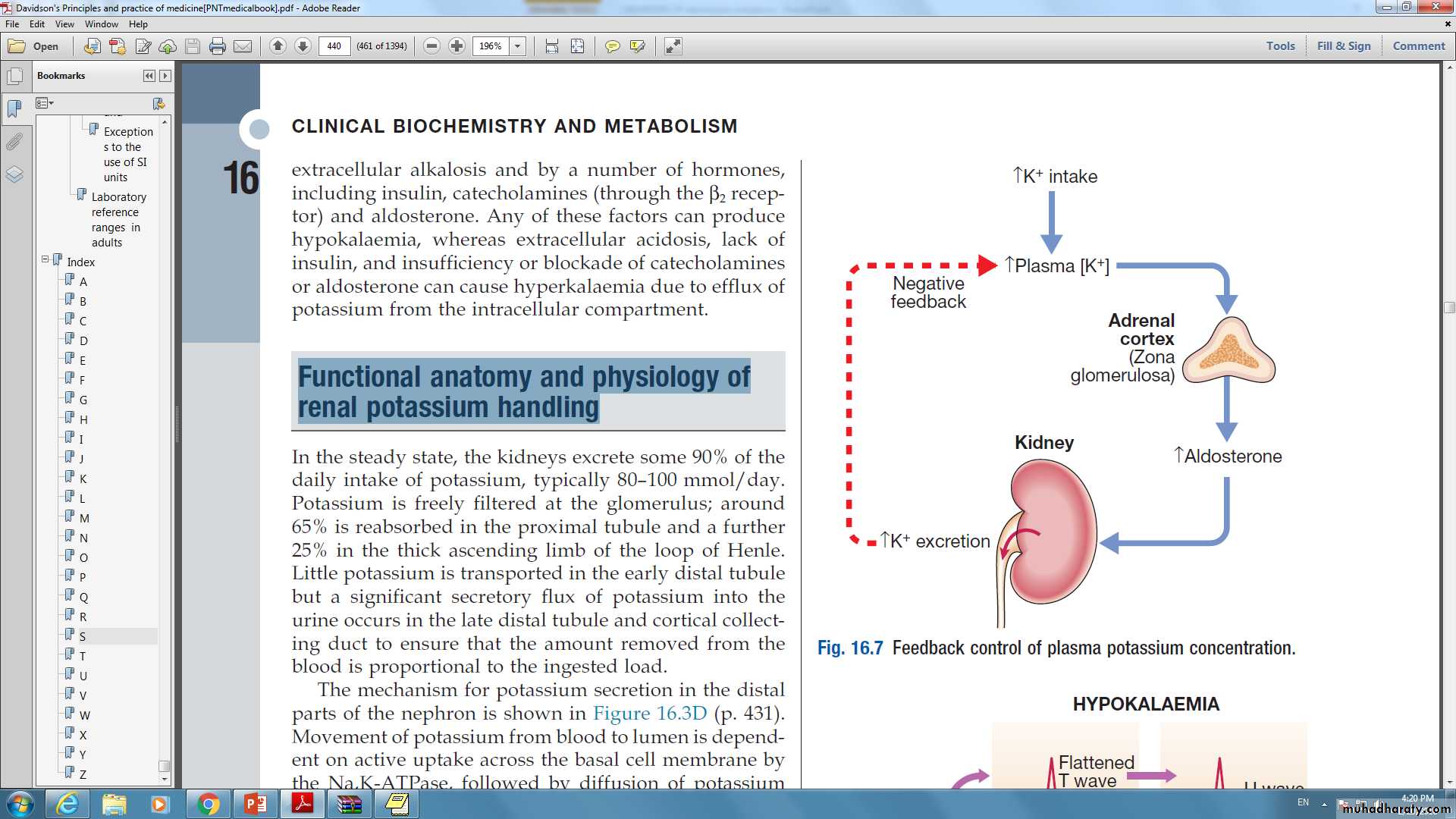
Functional anatomy and physiology ofrenal potassium handling
31
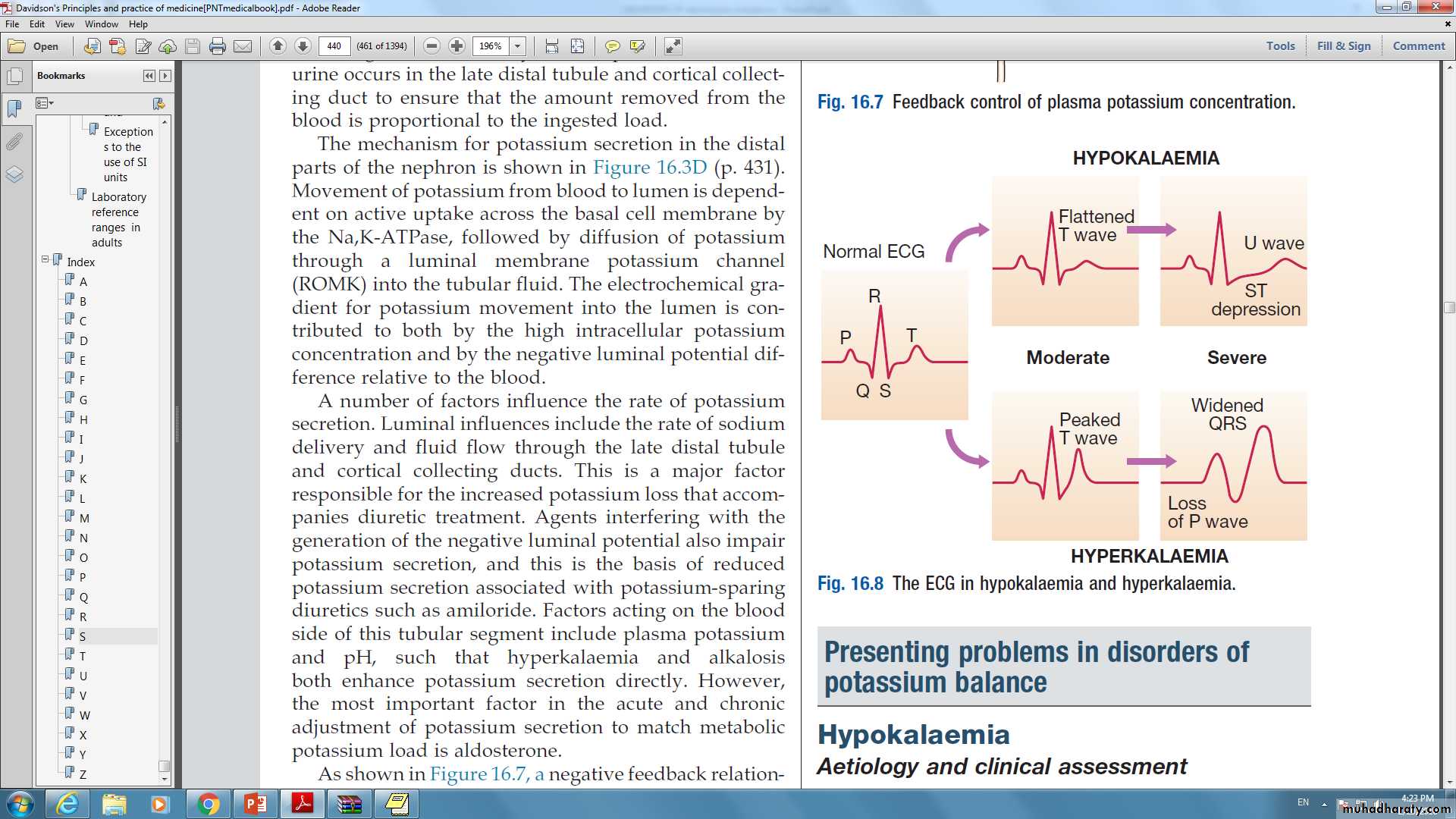
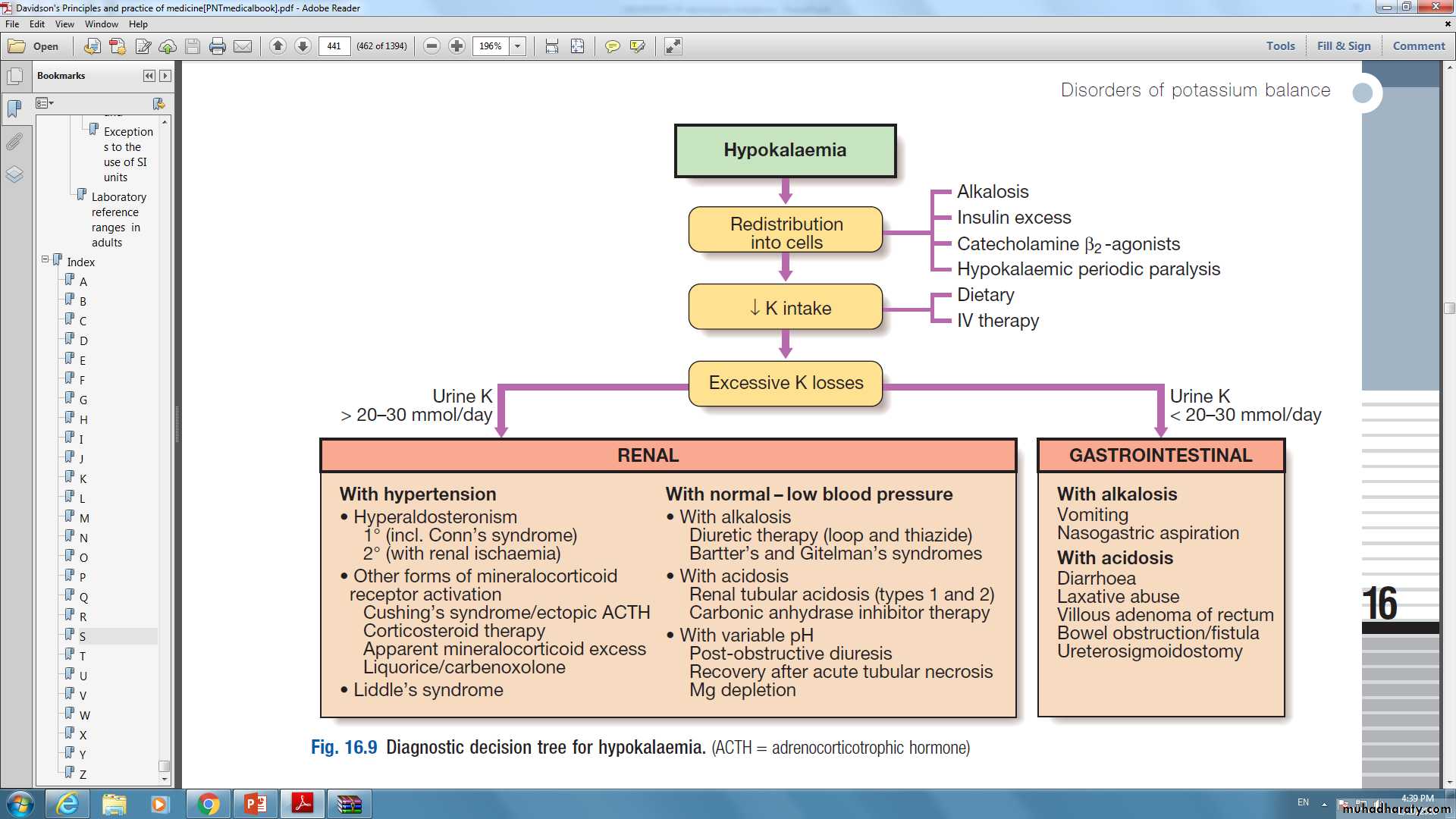
Presenting problems in disorders ofpotassium balance: Hypokalaemia
Aetiology and clinical assessment:Patients with mild hypokalemia (plasma K 3.0– 3.3 mmol/L) are generally asymptomatic, but more profound reductions in plasma potassium often lead to muscular weakness and associated tiredness.
Ventricular ectopic beats or more serious arrhythmias may occur and the arrhythmogenic effects of digoxin may be potentiated.
32
Hypokalaemia
Functional bowel obstruction may occur due to paralytic ileus.
Long-standing hypokalemia causes renal tubular damage (hypokalemic nephropathy) and interferes with the tubular response to ADH (acquired nephrogenic diabetes insipidus), resulting in polyuria and polydipsia.33
Hypokalaemia
34
Hypokalaemia : Management
Treatment of hypokalemia involves first determining the cause and then correcting this where possible.In most cases, however, some form of potassium replacement will be required. This can generally be achieved with potassium chloride tablets, but in more acute circumstances intravenous potassium chloride may be necessary.
The rate of administration depends on the severity of hypokalemia and the presence of cardiac or neuromuscular complications, but should generally not exceed 10 mmol of potassium per hour.
35
Hypokalaemia : Management
In patients with severe, life-threatening hypokalemia, the concentration of potassium in the infused fluid may be increased to 40 mmol/L if a peripheral vein is used, but higher concentrations must be infused into a large ‘central’ vein with continuous cardiac monitoring.
If magnesium depletion is also present , replacement of magnesium may also be required for hypokalemia to be corrected since low cell magnesium can enhance the mechanism for tubular potassium secretion , causing ongoing urinary losses.
36
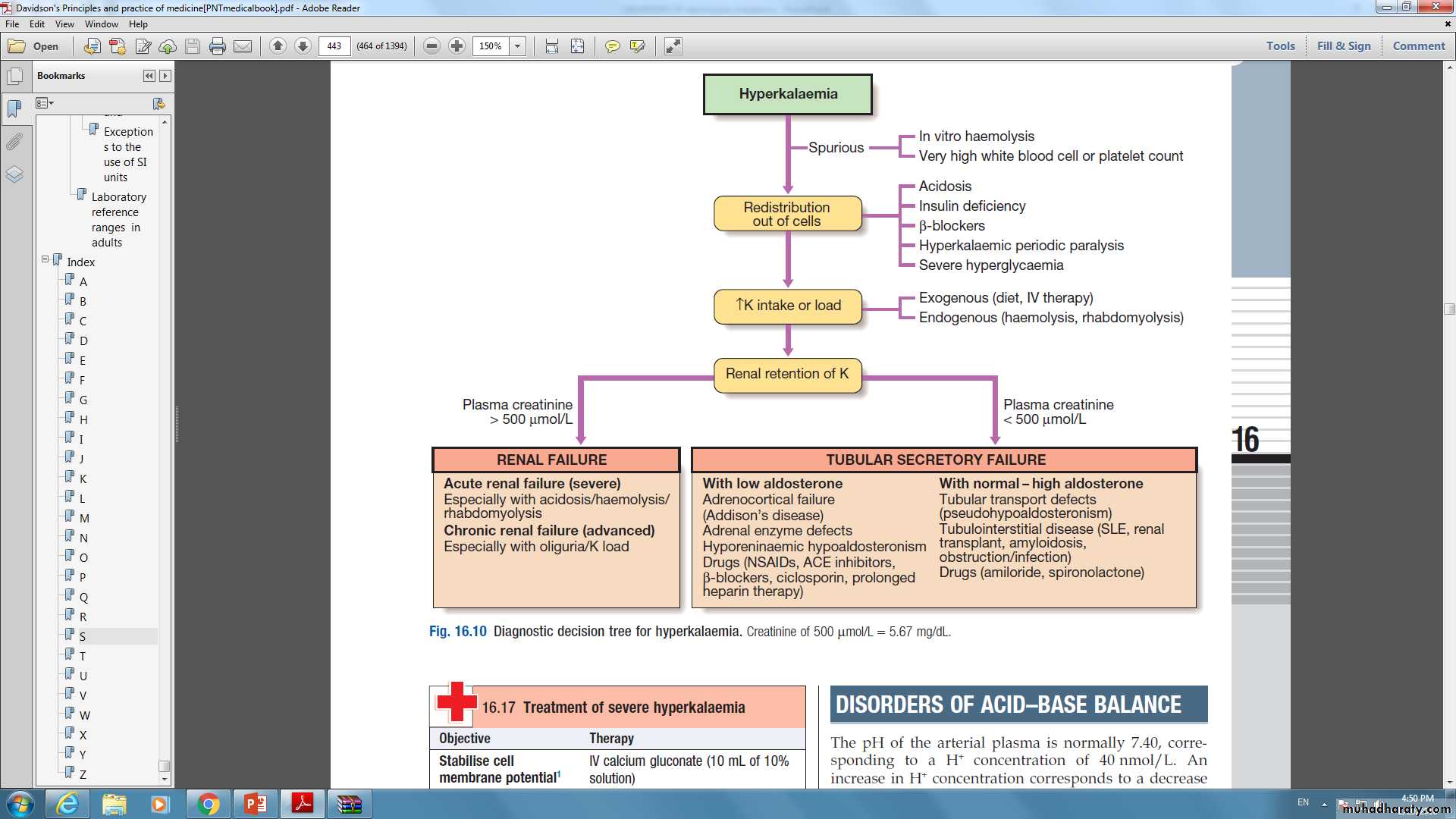
Presenting problems in disorders ofpotassium balance : Hyperkalemia
37
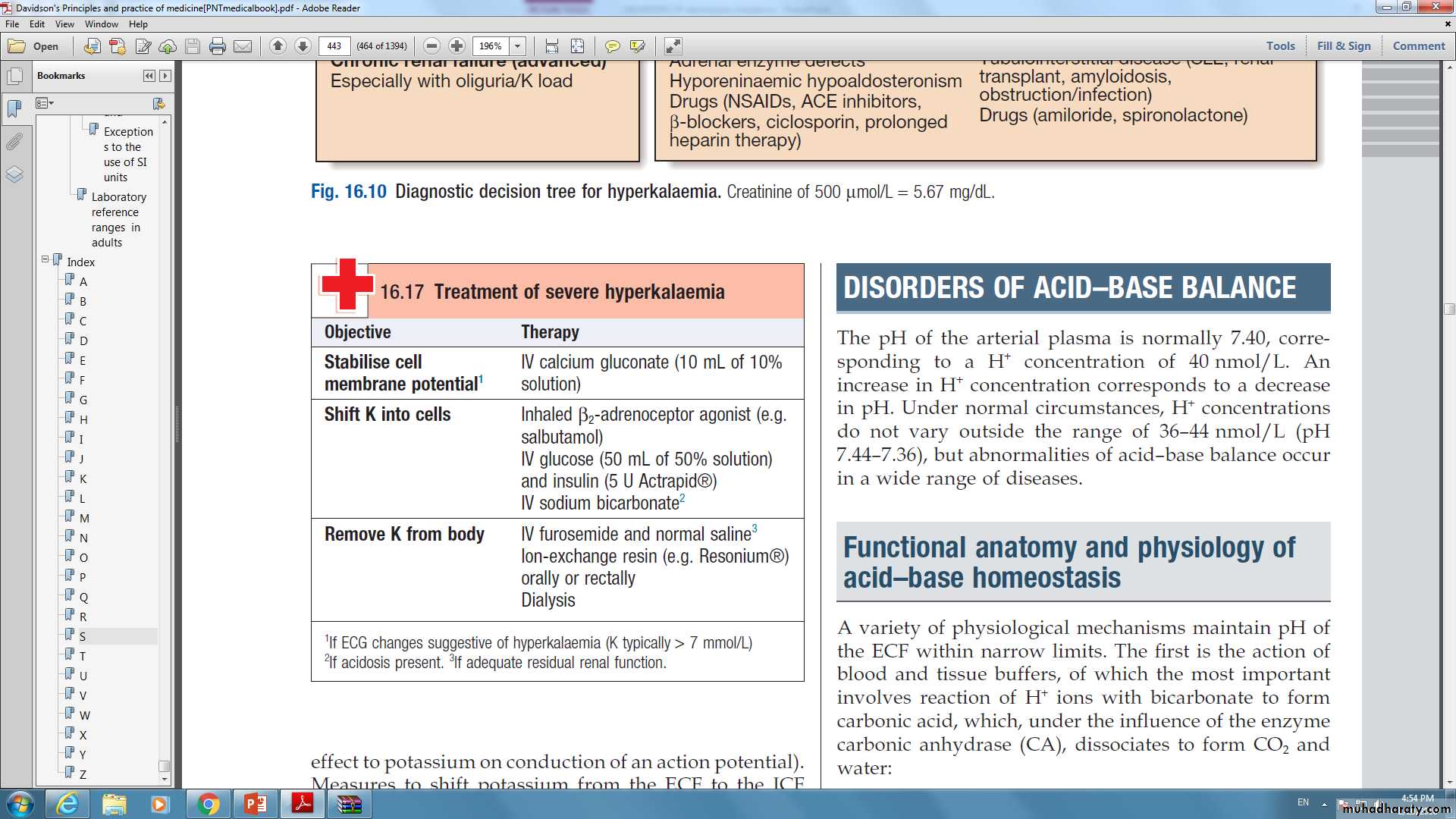
Hyperkalemia:Management
Treatment of hyperkalemia depends on its severity and the rate of development.In the absence of neuromuscular symptoms or ECG changes, reduction of potassium intake and correction of underlying abnormalities may be sufficient. However, in acute and/or severe hyperkalemia (plasma K > 6.5–7.0 mmol/L) more urgent measures must be taken.
If ECG changes are present, the first step should be infusion of 10 mL 10% calcium gluconate to stabilize conductive tissue membranes (calcium has the opposite effect to potassium on conduction of an action potential).
38
Hyperkalemia:Management
39
Functional anatomy and physiology ofmagnesium metabolism
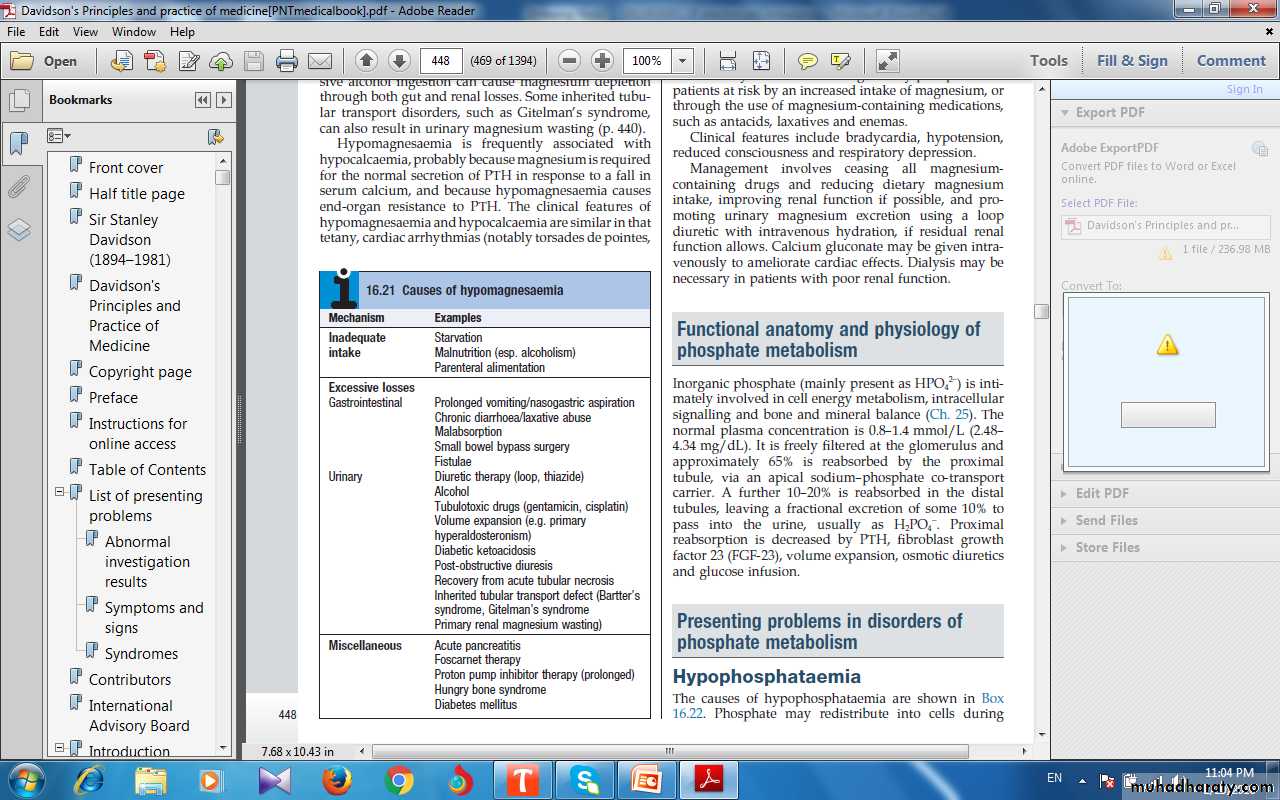
Hypomagnesaemia
Aetiology and clinical assessment
40
• Hypomagnesaemia
Hypomagnesaemia is frequently associated with hypocalcaemia so the clinical features of hypomagnesaemia and hypocalcaemia are similar in that tetany, cardiac arrhythmias (notably torsades de pointes ,central nervous excitation and seizures, vasoconstriction and hypertension may all occur.41
Hypomagnesaemia
ManagementThe underlying cause should be identified and treated where possible.
When symptoms are present, the treatment of choice is intravenous magnesium chloride ,when intravenous access is not available, magnesium sulphate can be given intramuscularly.
Oral magnesium salts have limited effectiveness due to poor absorption and may cause diarrhea.
42
Hypermagnesaemia
This is a much less common abnormality than hypomagnesaemia.Predisposing conditions include acute kidney injury and chronic kidney disease, and adrenocortical insufficiency.
Clinical features include bradycardia, hypotension, reduced consciousness and respiratory depression.
43
Functional anatomy and physiology ofphosphate metabolism
The normal plasma concentration is 0.8–1.4 mmol/L (2.48– 4.34 mg/dL).
It is freely filtered at the glomerulus and approximately 65% is reabsorbed by the proximal tubule and further 10–20% is reabsorbed in the distal tubules.
Reabsorption is decreased by PTH, volume expansion, osmotic diuretics and glucose infusion.
44
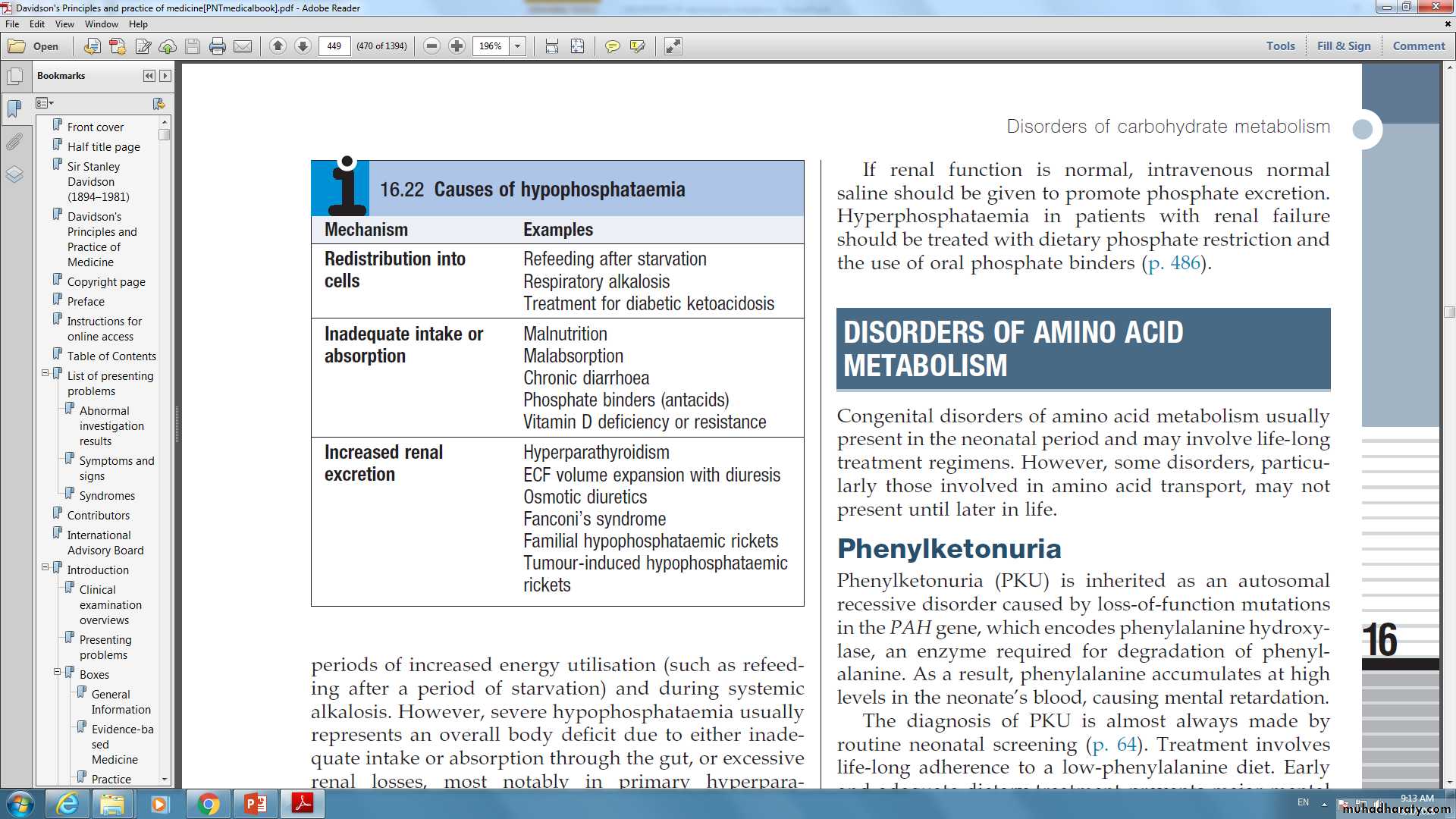
Hypophosphatemia
The clinical manifestations of phosphate depletion are wide-ranging.
Defects appear in the blood (impaired function and survival of all cell lines), skeletal muscle (weakness, respiratory failure), cardiac muscle (congestive cardiac failure), smooth muscle (ileus), central nervous system (decreased consciousness, seizures and coma) and bone (osteomalacia in severe prolonged hypophosphatemia).45
Hypomagnesemia:Management
involves administering oral phosphate supplements and high-protein/high-dairy dietary supplements that are rich in naturally occurring phosphate.Intravenous treatment with sodium or potassium phosphate salts can be used in critical situations.
46
Hyperphosphatemia
Phosphate accumulation is usually the result of acute kidney injury or chronic kidney disease ,phosphate excretion is also reduced in hypoparathyroidism and pseudohypoparathyroidism ,redistribution of phosphate from cells into the plasma can also be a contributing factor in the ‘tumor lysis’ syndrome and in catabolic states.The clinical features relate to hypocalcaemia and metastatic calcification, particularly in chronic renal failure with tertiary hyperparathyroidism (when a high calcium–phosphate product occurs).
47
Hyperphosphatemia
If renal function is normal, intravenous normal saline should be given to promote phosphate excretion.
Hyperphosphatemia in patients with renal failure should be treated with dietary phosphate restriction and the use of oral phosphate binders.
48
Thanks for your listening
4950