Fastidious Gram Negative Coccobacilli
د. زينة مكي عبد الكريم اليوزبكيMs.C. in Microbiology
Fastidious Gram Negative Coccobacilli
Three genera are included in this group of bacteria.• They are the following:
1. Genus: Haemophilus
2. Genus: Bordetella
3. Genus: Brucella
Genus Haemophilus
Haem = bloodPhilus = loving
These m.o are requiring blood for growth as enriched media.
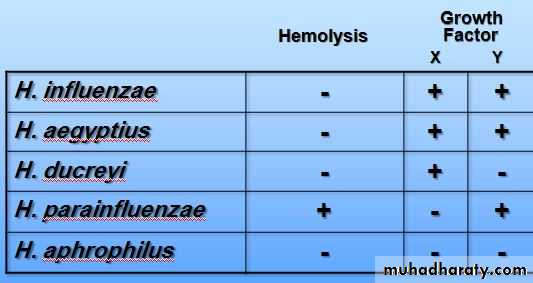
Classification:
There are 2 criteria for the classification of these m.o.:
1. Their ability to haemolyse blood.
2. Their requirments for X and/or V factors
Classification
Haemophilus influenzae (Pfeiffer’s bacillus)
General characteristics:Gram negative coccobacilli.
Facultativly anaerobic.
Organism is sensitive to drying and extremes in temperature
Distinctive “mousy” or “bleach-like” odor
Misnamed – originally thought to cause the “flu”
Now know that flu is caused by viruses
In some cases of flu, H. influenzae is secondary bacterial infection
Haemophilus influenzae
Have encapsulated and non encapsulated serotype.The encapsulated group are pathological types and the non-encapsulated groups are normal flora of upper respiratory tract .
There are 6 serotypes of it from a-f the most important one is type b.
Morphology:
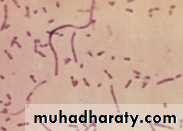
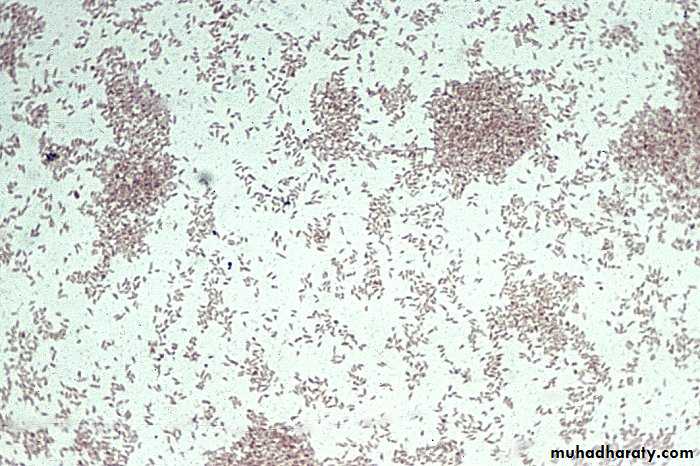
The typical m.o. are short bacilli (coccobacilli), but some times they are long bacilli and even filamentous forms.This characteristic is called pleomorphism.
From young cultures (6-8 hr.), the m.o. are coccobacilli and capsulated, while from old cultures (18-24 hr), they are long bacilli with filamentous forms and are non-capsultated.
The capsule can be typed by anti-sera in a reaction called “Quellung Reaction” which is “capsule swelling test”. The capsular antigen can be identified by counter current electrophoresis (CCE) and immunofluorescent (IF) test.
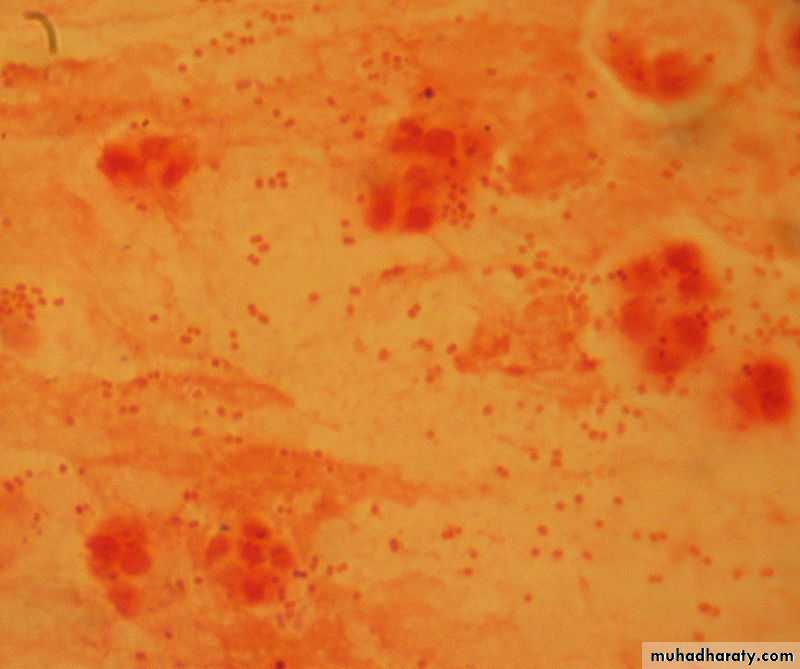
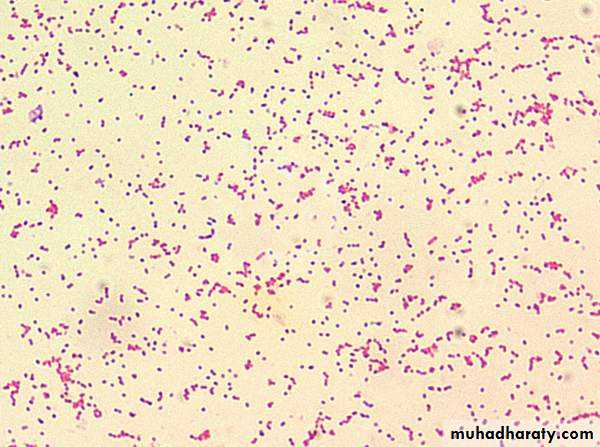
H. influenzae, in a Gram stain of a sputum sample, appear as Gram-negative coccobacilli
new culture H. influenzae, in a Gram stain from
new culture H. influenzae, in a Gram stain from
H. influenzae, in a Gram stain from old culturesgram negative long bacilli and even filamentous form and non capsulated
Culture media:
Have to contain blood from rabbits or horses and not from human or sheep because it contains anti-Haemophilus antibodies.The most important media used are:
A. Brain- heart infusion supplemented with blood.
B. Chocolate agar.
C. Levinthal’s agar which is nutrient agar supplemented with blood
Cultural Requirements
• 1. Both X and V factors are required for growth of H. influenzae.
• X = Heam or heamatin factor
Heat-stable substance
Present in RBC and released with degradation of hemoglobin
• important for respiratory enzymes of the m.o. including cytochrome oxidase, catalase.
V = (NAD: nicotinamide adenine dinucleotide)
Heat- labile
Found in blood or secreted by certain organisms
• 2. Temperature: These m.o. tolerate temperatures of 25 - 40 C, but the optimum is 37 C.
3. CO2: These m.o. require 10% CO2 for their growth
which is provided by candle jar.4. Isovitalex (1%): Added to the culture media can enhance the growth of the m.o.
Colony MorphologyOn choclate agar the m.o appear semi-opaque, gray-white, convex, mucoid
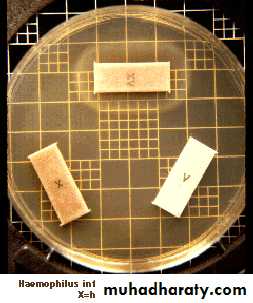
This organism would be identified as H. influenzae because it is using both X and V factors.
This organism would be identified as H. parainfluenzae because it is using V factor only.
Haemophilus influenzae b identification:
Gram stainGram negative cocco-baccillus
Catalase +ve
Oxidase +ve
X and V factor strips or disks.
Facultatively anaerobic need 10% CO2 (candle jar)
Culture on eneriched media
Isolation of this bacteria:
• Bacitracin: Can be added to the media and make more selective .
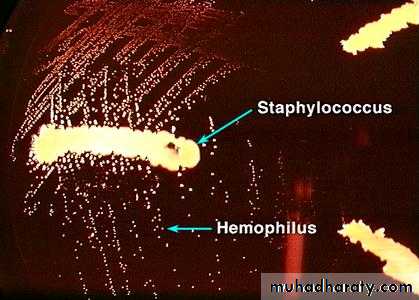
• Satellite phenomenon (Satellitism):
• around the growth of Staphylococcus aureus (or Strep. pneumoniae or Neisseria gonorrhoeae) the colonies of H. influenzae will be larger. This is because the former growth provides an extra amount of V factor which enhances the size of the colonies of the latter m.o.
Satellitisim phenomena of H. influanzae around and between the large, white, hemolytic staphylococci
Satellitisim phenomena of H. influanzae around and between the large, white, hemolytic staphylococci
Antigenic structures (virulent factors)
• Capsule• Which is of polysaccharides in nature. It is composed of polyribose ribitol phosphate (PRP). According to the serological types of PRP , the m.o. can be typed into 6 serotypes (a – f). It has Antiphagocytic
IgA Protease
Cleaves IgA on mucosal surfacesLipid A
Effects ciliated respiratory epithelium
Pili
AttachmentClinical conditions caused by H.infuanzae
• Acute epiglottitis or laryngotracheal infection in small children• Can cause airway obstruction needing immediate tracheostomy
• Cellulitis/arthritis
• cheek and upper extremities
• Meningitis
• Children under 6 years
• Contagious, vaccine has decreased incidence
• Pneumonia/septicemia
• In children
• Conjunctivitis “pink eye”
• very contagious
•
Diagnostic laboratory tests
1. Specimens: Nasopharyngeal swabs, pus, blood, and spinal fluid.2. Direct identification; by immunofluorescent (FA), Quellung reaction for capsule swelling test, or commercial kits for identification of H. influenzae antigens in the CSF.
3. Culture
Treatment
Mortality rate from H. influezae meningitis may reach up to 90%. Many strains of this m.o. are sensitive to:• ampicillin and 25% of them are beta lactamases producer.
• Most strains are susceptible to chloramphenicol. So, combined use of ampicillin and chloramphenicol in the treatment of meningitis is important to prevent neurological complications and intellectual impairment.
• Moreover, cefotaxime may also give excellent results . Subdural fluid accumulation after meningitis requires surgical drainage
Genus: Bordetella
There are 3 important species of Bordetella:1. B. pertussis.
2. B. Parapertussis.
3. B. Bronchiseptica.
B. pertussis is the causative agent of a highly infectious disease which is called pertussis (whooping cough).
B. parapertussis can cause a disease similar to whooping cough, but ofter subclinical of mild.
B. bronchisepica is important in canines, produces smaller m.o., and infrequently is responsible for chronuic RTI in humans.
General characteristics
Very small gram negative cocco –bacilli with toludine blue appear as bi chromatic granules .
Strictly aerobic.
Strictly human pathogen.
Transmission by aerosolized droplets
Heamolytic m.o.
Catalase and oxidase positive
Ferment glucose with acid and no gas production.
Do not require X and V factor for growth.
Require a special media for growth with prolonged incubation.
Culture media :
• For primary isolation; an enrichment media is used. This medium is called Bordet-Gengou (potato-blood-glycerol agar). The medium contains 20-30 % sheep blood cells and penicillin -G or methicillin to make more selective.• Buffered charcoal yeast extract agar (BCYE): this medium can also be used for the isolation of Legionella pneumophila .
• Blood Charcoal Agar (BCA) to which an antibiotic may be added as cephalexin to make more selective ( inhibits respiratory flora).
• Lowe-Regan agar which is similar to BCA, but contains a half strength of charcoal.
• Charcoal and cephalexin
• All media should be kept in moist environment (sealed plastic bag).
Cultural characteristics
The colonies appear as rounded, convex,1-2 mm in diameter, and look like mercury drops or pearl-appearance. The colonies have iridescence and surrounded by narrow zones of haemolysis
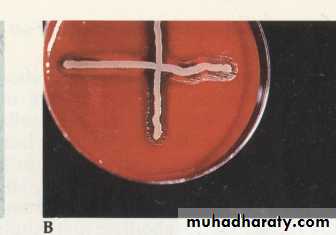
B. pertussis Small, transparent hemolytic colonies on Bordet-Gengou medium
Gram stain of B. pertussis
Antigenic structures:
• Capsule.• Pertussis toxin which have the following affects:
A. Prolonged immunity because it is an immunogenic factor.
B. Anaphylactic –like reaction due to histamine sensitization.
C. Paroxysmal cough that is followed by deep inspiration .
D. enhances insulin secretion
E. It reduces the migratory and phagocytic activity of macrophages and neutrophils.
F. Absolute lymphocytosis may reach up to 30000 /cmm.
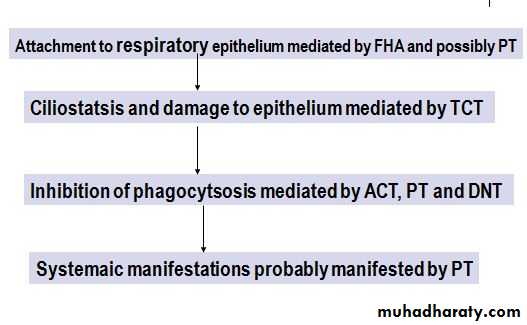
3. Filamentous haemagglutinin that mediates adhesion to ciliated epithelial cells.
4. Leucocytes promoting factor that promote lymphocytosis.5. Lethal toxin that causes local necrosis.
6. Tracheal cytotoxin which affects the activity of epith. and cilia of respiratory tract.
7. Adenylate cyclase complex that can impair phagocytosis.
Pathogenesis
Clinical manifestation of pertussis disease:
Spread by aerosol/direct contact with infected and carrier personsEarly symptoms - nonspecific- seldom diagnosed until paroxysmal stage- most contagious early
Stages- Incubation period: 7-10 days
Catarrhal stage:
Symptoms like common cold, lasts 1-2 weeks
Paroxysmal stage:
dry nonproductive cough, paroxysmal
excess mucus production, vomiting, convulsions, cyanosis, paroxysms separated by inspiratory whoop
Lasts 4-6 weeks
Children who are too young to be fully vaccinated and those who have not completed the primary vaccination series are at highest risk for severe illness
Diagnostic tests
1. Specimens: A saline nasal wash is the preferred specimen. Nasopharyngeal swabs or cough droplets expelled onto a “ cough plate” held in front of the patient’s mouth during a paroxysm are some times used.2. Direct fluorescent antibody (FA) test to examine nasopharyngeal swab specimens with sensitivity of 50%. Also, it is most useful in identifying B. pertussis after culture on solid media
3. Cultures: Mentioned previously.
4. Polymerase chain reaction (PCR): It is the most sensitive method for the diagnosis of pertussis.
5. Serology: Serological tests are of limited value because specific antibodies ( agglutinating or precipitating) rise does not occur until the third week of illness
Treatment
B. pertussis is sensitive to many drugs in vitro. During the catarrhal stage erythromycin promotes the elemination of the m.o. and may have prophylactic value. Treatment during the paroxysmal stage rarely alters the clinical picture.Prevention:
1. Vaccination (part of DTP): 3 doses in the first year of life, followed by booster of a total of 5 injections.2. New acellular vaccine of 5 antigens is also available.
3. Prophylactic erythromycin for 5 days is given for unimmunized infants or heavily exposed adults
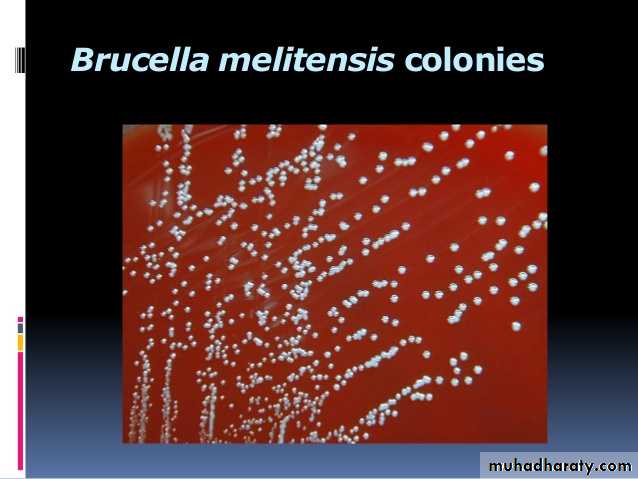
Genus: Brucella
Gram-negative coccobacillusFacultative intracellular parasites
Six species
B. abortus - cattle
B. suis - pigs
B. melitensis - goats
B. canis - dogs
B. ovis - sheep
B. neotomae - desert wood rats
Cause zoonoses worldwide
Disease in human: Brucellosis, Malta fever, Undulant Fever
Mediterranean Fever, Rock Fever of Gibraltar, Gastric Fever
Sir David Bruce (1855-1931) isolated
the bacterium of Malta fever in 1887Morphology :
The typical m.o. are predominantly gram negative coccobacilli, and from young cultures they vary from cocci to short bacilli and are capsulted , and stain irregularly. They are aerobic and nonmotile m.o.Culture media
1. Trypticase soy agar.2. Castaneda biphasic medium (broth & agar). This medium is prepared in bottles and has two portions; solid one (bottom), and liquid (top). The m.o. can grow on the surface of the solid portion and in the liquid rendering it turbid.
3. Blood agar or blood culture media.
4. MacConkey’s agar supplemented with 5% of heated horse or rabbit serum.
5. Brucella selective medium (good medium but expensive).
Cultural characteristics
Colonies are small, convex, smooth, translucent, nonhaemolytic, slightly yellowish in young cultures but brownish in old ones, and appear in 2- 5 days (may be delayed up to 3 weeks).Clinical picture and pathogenesis of Brucellosis
Method of transmission:1. Ingestion of raw or un boilled milk or milk products in particular white cheese.
2. Mucous membrane (droplets).
3. Skin (contact with infected animals or tissues as meat for workers in slaughter houses, butchers ,veterinarians, or house wives).
4. Conjunctiva rarely.
5. Breast milk lactating woman
the organisms are phagocytosed by macrophages and monocytes phagocytosed bacteria are carried to the spleen, liver, bone marrow, lymph nodes. the bacteria secrete proteins that induce granuloma formation
Incubation period 1-6 weeks
Insidious onset start as flue like symptoms.The fever usually rises in the afternoon; its fall during the night is accompanied by drenching sweat. There may be GI and nervous symptoms. L.N. enlarge, and the spleen palpableThe manifestations may subside in weeks or months , although localized lesions and symptoms may continue.
chronic stage may develop; characterized by weakness, aches and pains, low grade fever, nervousness or depression.
Brucellae usually can not be isolated from such patients except in only 2% of them. The diagnosis of “chronic brucellosis” is difficult to established.
Diagnostic tests:
A. Specimens: Blood and biopsy material
B. Culture: Mentioned above. Subcultures are made from at intervals from blood culture or broths.
C. Serology:
IgM antibody levels rise during the FIRST week of acute illness, peak at 3 months, and may persist during chronic disease.
IgG antibody levels rise 3 weeks after onset of acute disease, peak at 6- 8 weeks and remain high during chronic disease.
IgA levels parallel the IgG levels; could be blocking antibody (causes prozone pheno.).
Serological tests:
1. Agglutination test (tube or slide); using:a. Heat-killed phenolized smooth
standerized brucella antigens.
b. Rose bengal antigens (stained red).
The significant titre = 1/160 or higher.
Cross reaction may occur with cholera vaccine, S.typhi /paratyphi , or Yersinia.
2. 2-Mercaptoethanol test; 2-ME can destroy IgM and leaves IgG. This may be used to differentiate between current /recent brucellosis from previous /old brucellosis. Also, is useful in chronic active brucellosis
3.Blocking antibodies: These are IgA antibodies that interfere with agglutination by IgG & IgM and cause false negative result (prozone phenomena). These antibodies appear during the subacute stage of infection tend to persist for many years, and are detected by Coomb’s antiglobulin method. Also, high dilution agglutination test can overcome the problem of prozone phenomena.
4. Skin test (Brucellergen or Brucellin): it is DHS reaction to I.D. Injection of a protein brucella extract. Erythema, oedema, and induration develop within 24 hours. It is unreliable test & is rarely used.
5. ELISA , RIA or Immunofluorescent ; for Ab detection.
Treatment:
Combined anti-microbial drugs are used, taking in consideration that the m.o. is an intracellular one:
1. Ampicillin or tetracycline with Streptomycin give good result. Cotrimoxazole may be added.
2. Refampcin (900 mg once daily) with doxycycline (200 mg once daily) gives 97% cure rate. Also, an aminoglycoside drug could be added.
Treatment should be continued for at least 6 weeks and for bone or joint infections the treatment continues for at least 8 weeks.
For neuro-Brucellosis chloramphenicol or ampicillin could be used with other drugs
Francisella tularensis
Fastidious gram negative bacilliIntracellular pathogen
Strictly aerobic
Transmitted from animals to human
Cause ulceroglandular disease
Grow on media contain cystein-supplemented as sensitive and specific for their growth with prolonged incubation
Dx: By culture and serological methods.
Rx: Streptomycein