Urinary Tract InfectionsUTI
Dr. Mohammed Hannon Al Sodani C.A.B.M., F.I.C.M.S.Consultant Nephrologist
For 5th year students 2015-2016
College of Medicine , University of BaghdadMarch,14th,2016
UTI definition
-Multiplication of organisms in the urinary tract.
It is usually associated with the presence of neutrophils
and > 100 000 organisms/ml in a midstream sample of urine
The most common bacterial infection in medical practice
- Incidence 50 000 / million persons / year
1-2 % of patients in primary care
- Common in women ( 50% ) , 3% at the age of 20,
- Uncommon in males , except in first year of life & over 60.
- Common source of life-threatening G - ve septicemia
- Recurrent infection causes considerable morbidity;
- If complicated , it can cause ESRD
UTI Etiology and pathogenesis
When the UT is anatomically and physiologically normal with intact local and systemic defense mechanisms , bacteria are confined to the
lower end of the urethra.
local and systemic defence mechanisms
Neutrophil Activation is essential for bacterial killing.
Urine osmolality and pH > 800 mOsm/kg and low or high pH reduce bacterial survival.
Complement activation with IgA production uroepithelium.
Commensal organisms – ( lactobacilli, bacteroides) Eradication by antibiotics or by spermicidal jelly or results in overgrowth of E. coli.
Urine flow and normal micturition wash out bacteria..
Uroepithelium –Tamm-Horsfall proteins (in the mucus ) covering uroepithelium, have antibacterial properties. Disruption of this by trauma (e.g. sexual intercourse or catheterization) predisposes to UTI
UTI Etiology and pathogenesis
UTI is most often due to bacteria from the patient's own bowel flora , Transfer to Urinary Tract :
- Ascending transurethral route most often
- Bloodstream & Lymphatics
- Direct extension (e.g. vesicocolic fistula),
-
.
UTI Etiology and pathogenesis
- In women > men- relatively short urethra and
- absence of bactericidal prostatic secretions.
- Sexual intercourse may cause minor urethral trauma
-Instrumentation of the bladder
urine catheter
cystoscopy
may also introduce organisms.
UTI Etiology and pathogenesis
Organisms causing UTIOrganism Approximate frequency (%)
E. coli and other 'coliforms‘’ from GIT 75 %Proteus mirabilis 12%
Pseudomonous
Klebsiella aerogenes *
Enterococcus faecalis *
Staphylococcus 10%
†
UTI Etiology and pathogenesis
Natural history- Commonly it is an isolated
- In normal UT , seldom results in serious kidney damage
(uncomplicated UTI).
- Abnormal UT (with stones) & DM made worse with infection (complicated UTI).
- UTI, particularly (Proteus), may predispose to stone formation.
- The combination of infection and obstruction results in severe, rapid kidney damage (obstructive pyonephrosis) and is a major cause of Gram-negative septicaemia
UTI Risk Factors
- Incomplete bladder emptying;-
- Bladder outflow obstruction, e.g BPH
- Neurological problems (e.g. multiple sclerosis, diab.neuropathy) - Gynaecological abnormalities(e.g. uterine prolapse)
- Vesico-ureteric reflux
- Foreign bodies - Urethral catheter - Ureteric stent - Cystoscopy
- Loss of host defenses- Atrophic urethritis & vaginitis in post-menopausal women
- Diabetes Mellitus
- Others PKD, Renal stones
UTI The Spectrum Of Presentations
- Asymptomatic bacteriuria- Acute urethritis and cystitis
- Acute pyelonephritis
- Acute prostatitis
- Septicemia (usually Gram-negative bacteria
Acute urethritis and cystitis Lower UTi
Clinical Presentation- Frequency Abrupt onset
- Dysuria Scalding pain in the urethra during micturition
- Suprapubic pain during and after voiding.
- Urgency intense desire to pass more urine after micturition, due to spasm of the inflamed bladder wall &urethra))
- Urine cloudy and have an unpleasant odour
- Haematuria microscopic or visible.
- Systemic symptoms are usually slight or absent.
However infection can spread up ( acute pyelonephritis) In 30 %
- may also be present with - Minimal or no symptoms
- Atypical symptoms :- abdominal pain, fever or haematuria in the absence of frequency or dysuria
In small children, febrile sick child who fails to thrive.
The DDX
urethritis due to sexually transmitted disease, notably chlamydia
Reiter’s syndrome.
urethral syndrome
post-menopausal atrophic vaginitis.
Acute urethritis and cystitis Lower UTI
UTI Diagnosis
- Definitive diagnosis ( clinical features with findings in the urine)G U E:-
Macro. Turbid with debris, filaments , bad smell
Micro Pus cells +/- RBC
Urine C/S necessary, in patients with:-
- recurrent infection or
- after failure of initial treatment,
- during pregnancy, or
- serious infection ( Diabetics, immuno compromised ,Indwelling catheter & elderly)
In an otherwise healthy woman with a single lower UTI and no indications of a complicated infection, urine culture prior to treatment is not mandatory..
Gram stain of urine shows numerous Gram-negative rods.E.coli grew from this urine specimen
UTI Investigation
InvestigationCulture of MSU/ suprapubic aspiration
Micro ex, of urine for white and red cell
Dipstick ex. for nitrite and leucocyte esterase
May substitute for micro, C/S in uncomplicated infection.
Dipstick ex. of urine for blood, protein and glucose .
Full blood count
RFT
RBG
Blood culture
Pelvic examination Women with recurrent UTI
Rectal examination Men to examine prostate
UTI Investigation
Renal ultrasound or CT To identify obstruction, cysts, calculiInfants, children, men after single UTI, Women who have
(1) acute pyelonephritis;
(2) recurrent UTI after antibiotic treatment;
(3) UTI or asymptomatic bacteriuria in pregnancy
Intravenous urogram (IVU) :- Alternative to ultrasound, particularly to image the collecting system after voiding
Micturating cysto-urethrogram (MCU) or radioisotope study to identify and assess severity of vesico-ureteric reflux Cystoscopy;-
Patients with haematuria or a suspected bladder lesion
.
UTI Treatment
- Antibiotics are recommended in all cases of proven UTI
-Trt to be started while awaiting the result of c/s.
-Trt for 3 days is the norm and is less likely to induce antibiotic resistance than more prolonged therapy.
-Trimethoprim (200 mg 12 hrly) is DOC for initial Tr t.
Other effective ABC :-
- Nitrofurantoin, 50mg 6 hourly .
- Quinolone (ciprofloxacin / norfloxacin, levofloxacin)
- cefalexin. -
- Co-amoxiclav or amoxicillin should only be used when organism is known to be sensitive.
- Penicillins and cephalosporins are safe to use in pregnancy but trimethoprim, sulphonamides, quinolones and tetracyclines should be avoided.
.
UTI Treatment
- Trt is modified after C/S , &or the clinical response- In more severe infection, ABC/ 7-14 Days , intravenous cephalosporin, quinolone or gentamicin later switching to an oral agent
- A fluid intake of at least 2 L /day during trt & for few wk.
- Urinary alkalinizing (potassium citrate )may help symptomatically
.
Acute pyelonephritis
- Triad of - loin pain, fever with tenderness over kidneys.
- Pathology –etiology ;-- Pelvis; Inflamed, parenchy. small abscesses , PMN infiltration .
- Route ;- Ascending form lower UT (almost always)
- Bacteremia (rarely)- renal / perinephric abscesses
- Staphylococci mostly
- Pre existing renal damage by cyst or stone or scar.
- Medulla> cortex – low O2 tension, high osmolality, high H+
&ammonia , impaired WBC function
- -
Acute pyelonephritis
Clinical features;-- Acute loin(s) pain , radiated to IF or SPA /tender lumbar region
- 30% with cystitis
- Fever, rigor, vomiting &hypotension.
Rarely, complicated by papillary necrosis;- Fragments of renal papillary tissue are passed per urethra and can be identified histologically.
They may cause ureteric obstruction, and if this occurs bilaterally or in a single kidney, may cause acute renal failure.
Predisposing factors include DM
Chronic urinary obstruction,
Analgesic nephropathy and
Sickle-cell disease..
Acute pyelonephritis
Emphysematous pyelonephritis;-
A necrotizing form of pyelonephritis with gas formation,
is occasionally seen in patients with diabetes mellitus
Xanthogranulomatous pyelonephritis
is a chronic infection that can resemble a tumour. It is usually associated with obstruction, is characterised by accumulation of foamy macrophages and generally requires nephrectomy.. Infection of cysts in polycystic kidney disease requires prolonged antibiotic treatment.
Acute pyelonephritis
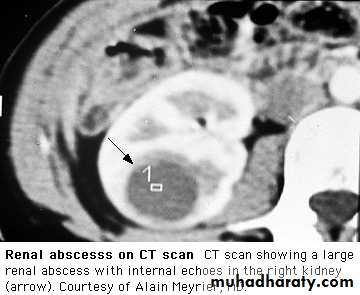
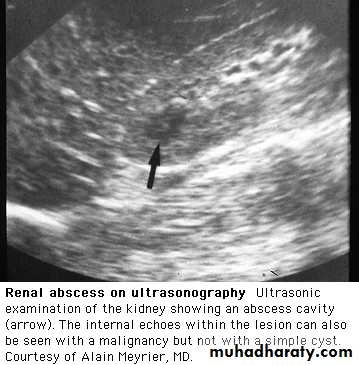
In perinephric abscess,there is marked pain and tenderness and often bulging of the loin on the affected side. Patients are extremely ill, with fever, leucocytosis and positive blood cultures. Urinary symptoms are absent, and urine contains neither pus cells nor organisms.
The D.DX of acute pyelonephritis includes;-
acute appendicitis,
diverticulitis,
cholecystitis and
salpingitis
ruptured ovarian cyst
ectopic pregnancy
Acute pyelonephritis
Investigations as in cyctitis Bacteria and neutrophils in the urine with typical clinical features confirm the diagnosis.Renal tract U/S, to exclude a perinephric collection and obstruction
should be considered
.
Acute pyelonephritis
Management- Adequate fluid intake, oral / intravenous.
- Antibiotics are continued for 7-14 days.
- Severe cases require I.V ABC , with a cephalosporin, quinolone or gentamicin), later switching to an oral agent.
In less severe cases, oral ABC can be used throughout.
Penicillins and cephalosporins are safe in pregnancy; other antibiotics should usually be avoided.
Urine should be cultured during and after treatment.
If obstruction is present, drainage by a percutaneous nephrostomy should be considered
.
Recurrent UTI
Relapse :-- Recurrence of bacteriuria with the same organism within 7 days of completion of antibacterial treatment
-Implies failure to eradicate infection,
- Usually in conditions such as stones, scarred kidneys, PKD or bacterial prostatitis.
Reinfection;-
- When bacteriuria is absent after treatment for at least 14 days,
- Followed by recurrence of infection with the same or different organisms.
- the result of reinvasion of a susceptible tract with new organisms.
PERSISTENT OR RECURRENT UTI
Prophylactic measures to be adopted by women with recurrent urinary infections
Fluid intake of at least 2 L/day
Regular complete emptying of bladder
If vesico-ureteric reflux is present, practice double micturition (empty the bladder then attempt micturition 10-15 minutes later
Good personal hygiene
Emptying of the bladder before / after sexual intercourse
Small dose abc at bed time
Cranberry juice may be effective
Drug
UTI3days
women 7days
A.Pyelonephritis
7-14 days
B.prostatitis
• 4-6weeksProphyl-actic
Trimethoprim200 mg daily
200 mg daily
200 mg 12 hr
100 mg night
Nitrofurantoin
50 mg 6 hr
50 mg 6-hr
Co-amoxiclav
250/125 mg 8hourly
250/125 mg 8hourly
250/125 mg night
Ciprofloxacin
100 mg 12 hr
250-500 mg 12hr 100 mg 12hr IV
250mg /12hr
Norfloxacin
400 mg 12 hr
400 mg 12 hourly
400 mg / 12 hr
Cefuroxime
250 mg/ 12 hr 750mg 6-8hrly IVCefalexin
500mg 12 hr
500mg 12 hr
250mg night
Gentamicin
3-5mg/kg IV daily
UTI in the presence of an indwelling catheter
After urinary catheterization > few days colonization of the bladder by a urinary pathogen,
an increases the risk of Gram-negative bacteraemia fivefold .,.
Treatment
is usually avoided in asymptomatic patients.
and ABC indicated only if ;-
- symptoms or evidence of infection,
- immunocompromised pt
- removal or replacement of the catheter.
Prevention
- Catheters should not be used unnecessarily
- Sterile insertion, to be removed as soon as it is not required
- Closed drainage systems .
.
UTI in the presence of an indwelling catheter
- Bladder stonesmay form with long-term indwelling catheters,
- Infection by Candida
is a frequent complication of prolonged bladder catheterization. Specially in DM .
Treatment for patients with evidence of invasive infection or those who are immunosuppressed,
- removal or replacement of the catheter,
- urinary alkalinazation and
in severe infections intra vesical amphotericin
Asymptomatic bacteriuria
This is defined as > 100 000/ml organisms in the urine of apparently healthy asymptomatic patients.
Approximately 1% of children < 1yr,
1% of schoolgirls,
0.03% of schoolboys and men,
3% of non-pregnant adult women and
5% of pregnant
more > 65 yr
30% ---- symptomatic infection within 1 year. n.
Asymptomatic bacteriuria
. There is no evidence that this condition causes renal scarring in adults who are not pregnant and have a normal urinary tract,
- In general, treatment is not indicated only In :-
Infants
Pregnant women
Abnormal urinary tract.
Bacteriuria in pregnancy
.- Urine C/S is a must in pregnancy
- 2- 6% asymptomatic bacteriuria.
- Risk of - severe symptomatic pyelonephritis
- premature labour.
-previous renal dis., - pre-eclamptic toxaemia,
- anaemia of pregnancy,
- small or premature babies.
Therefore bacteriuria must always be treated and be should to be eradicated.
Reinfection may require prophylactic therapy..
Bacteriuria in pregnancy
Amoxicillin and ampicillin, Nitrofurantoin &Cephalosporins may be safely be used in pregnancy
WHILE
Tetracycline, trimethoprim, sulphonamides and 4-quinolones must be avoided in pregnancy
Urethral Syndrome
- Abacteriuric frequency or dysuria
- Usually female,
- Symptoms of urethritis and cystitis
- No bacteria are cultured from the urine. 'sterile pyuria',
Causes include:-
- postcoital bladder trauma,
- post menopausal atrophic vaginitis or urethritis in the elderly,
- interstitial cystitis
- infection with organisms not cultured by ordinary methods
(e.g. Chlamydia, certain anaerobes ,TB),
- intermittent or very low-count bacteriuria,
- reaction to toilet preparations or disinfectants.
Urethral Syndrome
0ther causes;-- Incomplete trt by ABC.
- Malignancy
- Stones
- Vasculitis
Antibiotics are not indicated
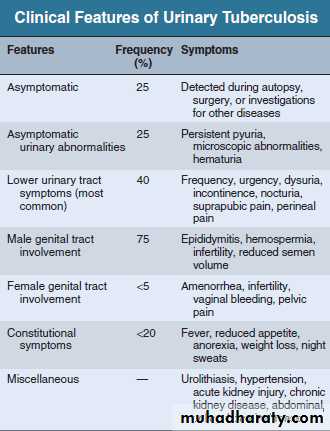
Tuberculosis of the urinary tract
- TB Increase world-wide, in low socioeconomic group ,reservoir of infection in HIV-infected individuals and by
the emergence of drug-resistant strains. .
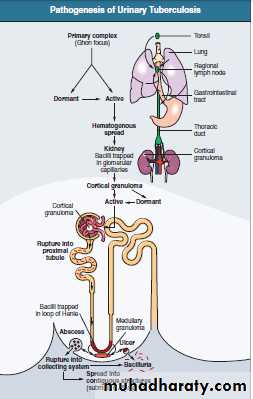
- Pathology
Cortical lesions from haematogenous spread in the primary phase. – Either - heals (most ) or
- persists - spreads to the papillae, cavitating lesions
- discharge of mycobacteria into the urine.
- Infection of the ureters and bladder,
( ureteral stricture , a contracted bladder)
- Rarely, cold abscesses may form in the loin.
- In males the disease may present with testicular or epididymal discomfort and thickening.
TB ofthe urinary tract
Tuberculosis of the urinary tract
A high index of suspicion
age 20 and 40 years ,
male to female ratio of 2:1..
High risk ;-
close contact with sputum smear–positive pts,social deprivation, neglect,
immunosuppression, HIV infection or (AIDS),
DM, CRF..
Transplanted kidneys may also transmit TB to their
recipients. Pathogenesis of
Tuberculosis of the urinary tract
Diagnosis ;-- Constant awareness, ??? sterile pyuria. - - - -
- Active infection - AFB with culture of mycobacteria from early-morning urine samples
- Excretion urography may show;-
- Cavitating lesions in the renal papillary areas, commonly with calcification.
- Evidence of ureteral obstruction with hydronephrosis.
- may be normal in diffuse interstitial renal TB
Tuberculosis of the urinary tract
- Renal biopsy.
Some patients present with small unobstructed kidneys, when the diagnosis is easy to miss.
- Renal ultrasonography or excretion urography
should be carried out 2-3 months after initiation of treatment as ureteric strictures may first develop in the healing phase.
Plain x-raycalcified kidney
Multiple ureteral strictures. Strictures associatedwith dilated ureter, infundibular stenosis and caliectasis
Renal tuberculosisCT scan shows an enlarged leftkidney with multiple cavities present bilaterally (
Contrast-enhanced CT image showing contractedcalcified right kidney and normal opposite side
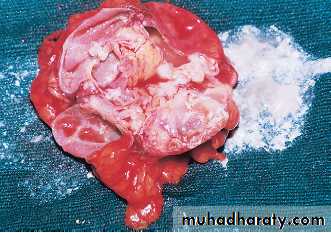
Renal tuberculosis. A cut section of kidney showingareas of cavitation and caseation necrosis (white chalky material).
Tuberculous granuloma. The granuloma comprisesLanghans giant cells (two large cells in the center), surrounding epithelioidcells, and a rim of lymphocyt es
Treatment
usually amenable to medical treatment.Many anti-TB drugs reach kidneys, urinary tract, urine, and cavitary lesions in high concentration, and there are
fewer organisms compared with cavitary lung lesions.
A short-course regimen is recommended.
The treatment is as for pulmonary TB
Daily rifampin (600 mg), isoniazid (300 mg), pyrazinamide (1500mg) in the morning. pyrazinamide is discontinued after 2 months, and isoniazid and rifampin are continued for another 4months.
Treatment
If the patient is very sick with irritative bladder symptoms,streptomycin in daily doses of 1 g may be added during the first 2 months
Longer courses of anti TB treatment 9 months to 2 years are useful in patients
who do not tolerate pyrazinamide,
those responding slowly to a standard regimen,
those with miliary or CNS disease,
and children with multiple-site involvement
Treatment
Surgical treatment. For
ureteral strictures,
- Stents across the narrow segment.
- Reconstructive surgery involves the correction of obstruction to the ureter pyeloplasty,….
- ??? Removal of a unilateral nonfunctioning kidney is controversial.