Forth stage
SurgeryLec-3
د. زيد
17/3/2016
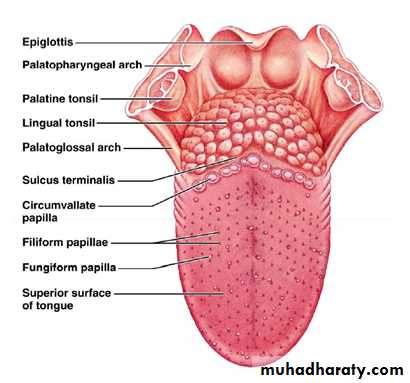
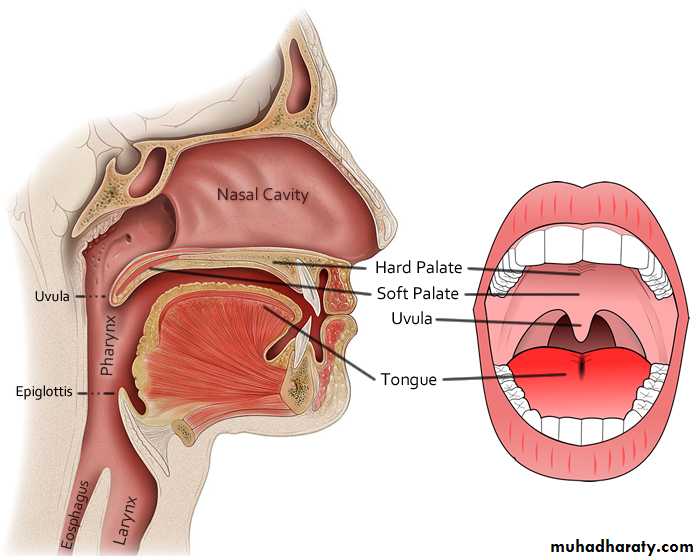
The oral cavityFrom the skin–vermilion border of the lips ant. to the junction of the soft palate sup. & the line of circumvallate papillae (the junction of the post. 1/3 and ant. 2/3of tongue posteriorly).
DEVELOPMENTAL ANOMALIES OF TONGUE
AGLOSSIA: absence tongue.Microglossia.
Macroglossia (cong./ acquired).
CLEFT or BIFID TONGUE : failure of fusion of 2 lingual processes.
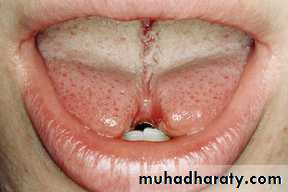
TONGUE TIE(ANKYLOGLOSSIA): short thick lingual frenum.
May cause:
Impairment of tongue movements.
deformity of dental occlusion.
difficulty of swallowing & speech defects
Treatment: partial self correction
complete division of frenum
(LA,GA)
Black hairy tongue (or lingua villosa nigra):
Painless.
benign disorder.
Hyperplasia of filiform papillae.
Overgrowth of pigment producing organism.
Treatment: cleaning and brushing the tongue.
GEOGRAPHIC TONGUE or benign migratory glossitis :
benign condition
alternating red & yellowish-white areas due to alternating hypertrophy / atrophy of tongue papillae
unknown etiology.
Treatment : proper tongue hygiene.
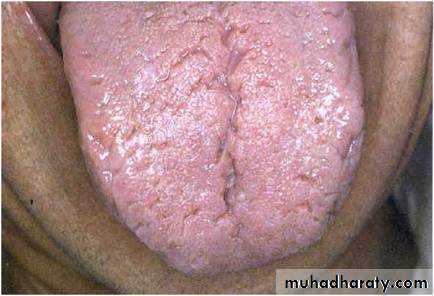
CONGENITAL FISSURED TONGUE (FURROWING):
furrowed surface of the tongue.deep median fissure.
many short fissures run transversely from a median groove.
This sometimes get infected by candida albicans resulting in median rhomboid glossitis.
Median rhomboid glossitis
Candida albicans infectionRed, smooth, oval- or diamond-shaped de-papillation
on the dorsum of the tongue
just ant.to the circumvallate papillae.
Treatment : antifungals .
LINGUAL THYROID
red lobulated mass.Post. 1/3 of tongue.
may be the only thyroid tissue present.
asympt.
Or cause obstructive symptoms such as choking, dysphagia, airway obstruction, or hemorrhage.
Treatment :
if symptomatic check if there is other thyroid tissue.
exogenous thyroid hormone may need radioactive iodine (RAI) ablation followed by hormone replacement and rarely Surgical excision.
Tongue injury
CAUSES:
Tongue biting (commonest) e.g. fall, seizure, or other blunt force
Piercings, intoxication, and iatrogenic causes.
bleeding
Why serious especially in unconscious?
Tongue hematoma can cause airway obstruction
If laceration serious bleeding.
Treatment:
Usual heal well without repair
Repair indicated if: (suturing by Absorbable sutures 4-0)
Bisecting wounds.
Large flaps.
Persistent bleeding.
Wounds larger than 1 cm.
Gaping wounds.
U-shaped lacerations.
Avulsion or amputation injuries.
Tongue ulcer
TRAUMATIC ULCERS: DENTAL ULCER
repeated trauma by carious ,broken or ill-fitted denture.
At tongue side of the tongue.
Acute :Painful oval-round ulcers with granulating floor , soft base & sloping margin +/- enlargement of draining LN
Chronic : ulcer edge is raised & indurated base + LN enlargement so biopsy is indicated to rule out ca.
Treatment: Removal of cause & antiseptic mouth wash.
INFLAMMATORY ULCERS:
A. IDIOPATHIC APHTHOUS ULCERS (dyspeptic)
Most common lesion .
Recurrent, very painful ulceration / healing
Etiology: ??,
TYPES:
Minor
Major
Herpetiform
B. Oral LICHEN PLANUS
Dermatologic disorder ?? due to autoimmune /HIVUlcers + hyperkeratotic whitish tongue lesions
C. HERPETIC ULCERS( herpes simplex type 1).
Recurrent self limiting multiple small ulcers in children preceded by blisters at tip of tongue
D.TUBERCULOUS.
E. SYPHILITIC (snail track / gummatous ulcers).
F. CHRONIC SUPERFICIAL GLOSSITIS.
NEOPLASTIC ULCERS: A- S.C.C (most common).B-Lymphoma.
Other Tongue lesions:
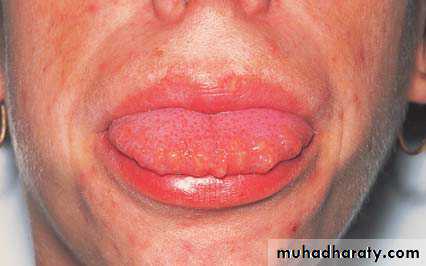
Multiple mucosal neuromata on the tongue of a patient with MEN 2b.
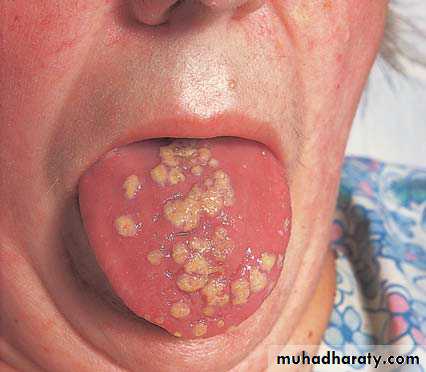
Monilial stomatitis. The colonies of Monilia on the tongue and mucous membranes look like patches of cream-coloured paint.
Oropharyngeal cancer
MenElderly(>60)
frequently involved sites :
the floor of the mouth
the lateral border of the anterior tongue
the retromolar trigone.
Histology:
Squamous cell carcinoma is the predominant
minor salivary glands tumours
Lymphomas
Tobacco and alcohol are the main causes.
chronic irritation 7 S (Smoking or tobacco chewing, Sharp tooth, chronic dental Sepsis, Syphilis, Spirits, Spices & Snuffing) .
Conditions associated with malignant transformation
High-risk lesions
Erythroplakia
Speckled erythroplakia
Chronic hyperplastic candidiasis
Medium-risk lesions
Oral submucous fibrosis
Syphilitic glossitis
Sideropenic dysphagia (Paterson–Kelly syndrome)
Low-risk/equivocal-risk lesions
Oral lichen planus
Discoid lupus erythematosus
Discoid keratosis congenital
Leucoplakia
White hyperkeratotic patches or plaque .
No pathological or clinical characteristics.
variable Size: (small, well-circumscribed, homogenous white plaque to an extensive large surface areas) .
May be smooth or wrinkled, fissured
vary in colour (white paint coated tongue that can not be rubbed off)
Speckled leucoplakia
Variation of leucoplakia on erythematous base
Has a highest rate of malignant transformation
Erythroplakia
Bright red plaque which cannot be characterized clinically or pathologically
Are irregular in outline and separated from nearby normal mucosa
The surfaces may be nodular.
They occasionally coexist with leucoplakia.
Chronic hyperplastic candidiasis
dense plaques of leukoplakia around commissures of mouth.
Rx6 weeks antifungal
If no response surgical excision or laser vaporisation
Oral submucous fibrosis
Asian population
Progressive epithelial fibrosis + atrophy and hyperplasia/dysplasia of the overlying epithelium
use of pan masala areca nut, with or without concurrent alcohol use.
fibrous bands form beneath the oral mucosaScarring contracturelimited mouth opening and restricted tongue movementRX. intralesional steroids or surgical excision and skin grafts.
Sideropenic dysphagia (Plummer–Vincentand Paterson–Kelly syndromes)
Sideropenia (iron deficiency without anaemia) predisposes to CA due to epithial atrophy.
iron to reduce epithelial atrophy and risk of ca.
Potential for malignant change
increases with increasing age of the patient;
increases with increasing age of the lesion;
is higher in smokers;
increases with alcohol consumption;
depends on the anatomical site of the premalignant lesion; particularly high for leukoplakia on the floor of the mouth and ventral surface of the tongue, particularly in younger women, even in the absence of associated risk factors.
Pathology of oral cancer:
Main sites : the floor of the mouth, the lateral border of the anterior tongue and the retromolar trigone:
GROSS TYPES:
Malignant ulcer: deep irregular necrotic floor, raised everted or rolled edge& hard red indurated base.
Raised oval white plaque that fungates as cauliflower-like mass +central necrosis .(commonest)
Hard sub mucous nodule (less common)
Deep indurated chronic fissure that does not heal.
Diffuse infiltrative wooden base i.e frozen tongue (rare)
MICROSCOPIC TYPES:
Ant. 2/3 well differentiated squamous cell ca. > 95%.
Post 1/3 ca are less differentiated
Basal cell ca & adenoca of minor salivary glands (rare)
SPREAD: CA in situ=no invasion to BM + no spread.
Direct (local) spread :
Ca ant 2/3 invades lat. then to floor of mouth then to mandible.
Post 1/3 ca invades tonsils, pharynx & larynx..
Fascial planes& periosteum act as barriers to direct spread
Lymphatic spread: occurs early with 30% clinical / subclinical
Ca. tip of tongue drains bilaterally to submental LN.
Ca. ant.2/3 to ipsilateral SMD& then to DCLN..
Ca. post 1/3 drains bilaterally to upper DCLN.
Blood spread: very rare& occurs in post 1/3 ca & correlates with distant metastases (bad prognosis).
Perineural invasion (bad prognosis)
Main clinical features of oral cancer
■ Elderly, males +/- risk factors .
■ Persistent oral swelling or mouth ulceration for > 4 weeks.
■ Painless unless deeply invasive (sore tongue).
■ Difficulty swallowing.
■ Jaw or facial swelling.
■ Painless palpable submandibular or jugular L. nodes .
■ Unexplained tooth mobility.
■ Trismus.
■ Fixation of tongue (Ankyloglossia).
Complications
Inhalation of necrotic tissues bronchpneumonia.Combined cancer cachexia & starvation due to pain & dysphagia.
Bleeding due to erosion of lingual vessels& erosion of ICA in post 1/3 tumors.
Asphyxia due to enlarged fixed LN or due to glottic edema.
Investigations of ca tongue:
Biopsy (for the suspicious lesion)Additional investigations:
Plain radiography of the jaw
MRI of head and neck
Ultrasound &CT
radioisotope bone scan of the facial skeleton
Treatment of Tongue cancer
Carcinoma in situ Rx =
localized small lesions, on the lateral border of tongue Rx by
surgical excision + primary closure.
Larger lesions = laser vaporization
T1 (< 2 cm diameter) tumour = either surgery or radioth.
Surgery :Surgical excision of tumour by partial (hemiglossectomy 2 cm margin + Ipsilateral selective neck dissection.Radiotherapy.
Advanced tumours (T3 and T4 cross midline)
Rx= total glossectomy, floor of the mouth and mandible+ bilateral neck dissection.Palliative treatmentIndicated for recurrence, metastasis ,fixed LN or unresectable tumours:
Radiotherapy
Palliative debulking of big primary
Combination Chemotherapy
Radiofrequency thermal ablation:
Supportive care.
Prognosis: Depends on:
Site : posterior 1/3 poor prognosisTNM Stage:
Size (T)= large tumours more LN metastasis.
Cervical node metastasis (N)= is the most significant factor in determining prognosis .
Concomitant medical problems as CVS or resp. disease.