Auto Immune Diseases
Ch 4((P 120 - 134
March. 7. 2016
Autoimmunity is hard to classify as strictly a B cell or T cell mediated disease as multiple arms of the immune system are involved
• Auto Immune Diseases
Auto Immune DiseasesSymptomsInitial diagnosis may be missed in patients as diseases present with general symptoms
Fever, muscle ache, fatigue, joint pain
Disease specific manifests
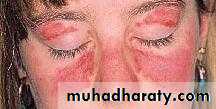
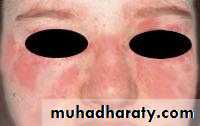
SLE – rashSjogren’s – dry mouth, dry eyes
Diagnosis
General testsC - Reactive Protein
Autoantibody titers (anti DNA, anti phospholipids, etc)
Presence of Rheumatoid Factor
Disease specific tests
Neurological exam – MSFasting glucose - Diabetes
SLE
A multisystem autoimmune disease.
Most organ involve in the body; skin, kidneys, serosal membranes, joints, & heart.
Remitting and relapsing.
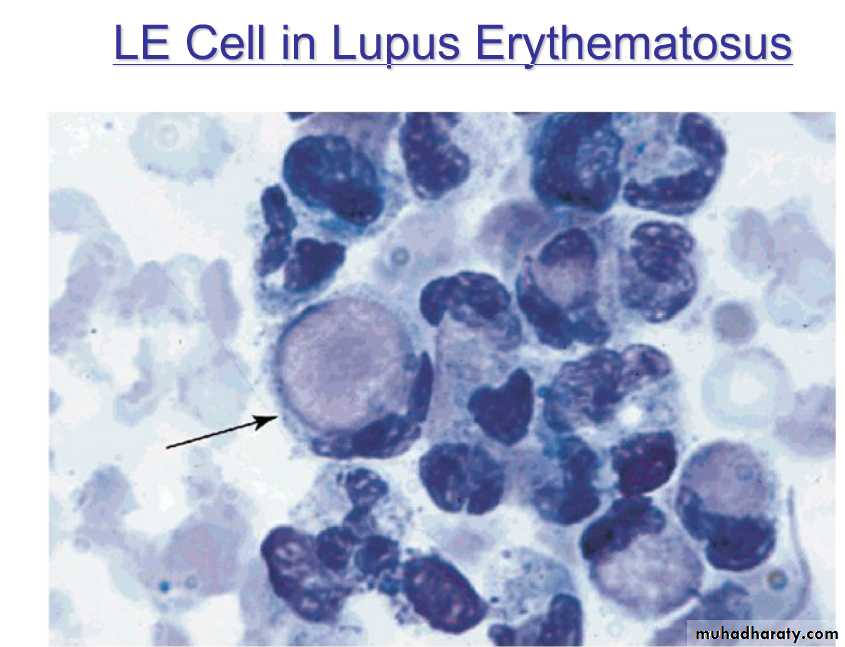
autoantibodies, including (ANAs).
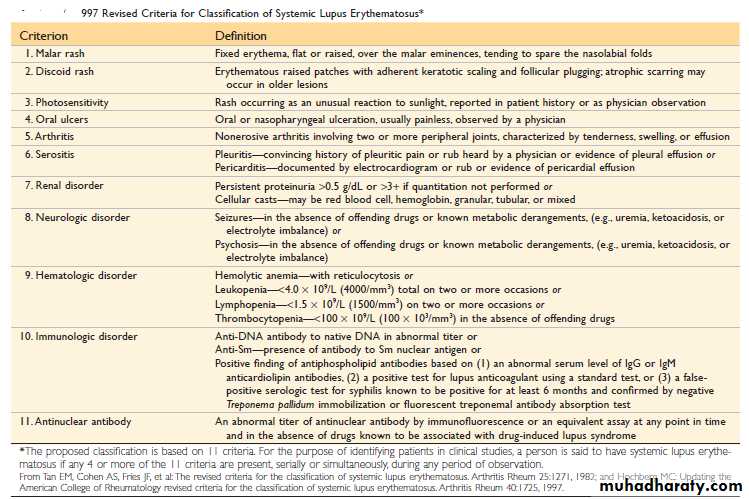
Dx; demonstration of four or more of the criteria
(F / M = 9 : 1)
2nd or 3rd decade of life.
SLE
Genetic
family
HLA-DR2, HLA-DR3
Low complement.
Environmental factors;
UV, Smoking, hormones, Drugs
The diagnosis is established by demonstration of four or more of the criteria during any interval of observation.
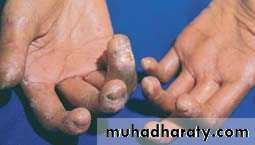
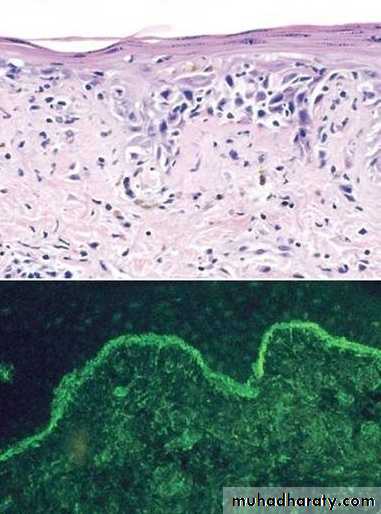
SLE, SKIN
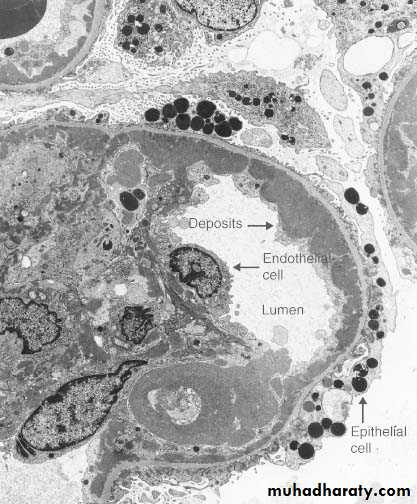
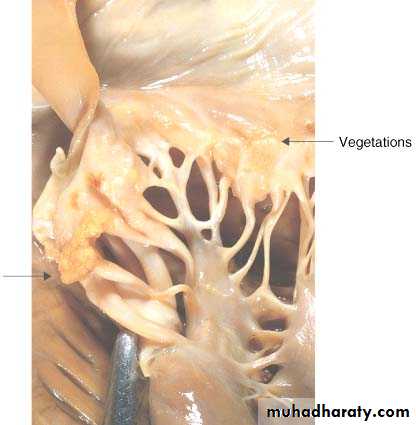
SLE, GlomerulousLibman-Sacks vegetations
Libman-Sacks vegetations, (Libman-Sacks endocarditis), are on BOTH sides of the leafletLUPUS (SLE)
Etiology: Abs directed against the patient’s own DNA (ds DNA), HISTONES, NON-histone RNA, & NUCLEOLUS (Sm), & phospholipids.Abs against Bl. Cells
Abs against phospholipids.
Pathogenesis: Immune complex disease, in skin, joints, kidneys, vessels, heart, CNS
& Type II HR in Blood cells.
Morphology: “Butterfly” rash, skin deposits, GN.
Clinical expression: Progressive renal and vascular disease, POSITIVE A.N.A.
Antigen
Ab SystemAntinuclear Abs in Autoimmune Diseases
SLE
Drug-Induced LE
SS—Diffuse
S—CREST
Sjögren Syndrome
Many nuclear antigens (DNA, RNA, proteins)
Generic ANA (indirect IF)
>95
>95
70–90
70–90
50–80
Native DNA
Anti–double-stranded DNA
40–60
<5
<5
<5
<5
Histones
Antihistone
50–70
>95
<5
<5
<5
Core proteins of small nuclear RNP particles (Smith antigen)
• Anti-Sm
20–30
<5
<5
<5
<5
RNP (U1RNP)
Nuclear RNP
30–40
<5
15
10
<5
RNP
SS-A(Ro)
30–50
<5
<5
<5
• 70–95
RNP
SS-B(La)
10–15
<5
<5
<5
• 60–90
DNA topoisomerase I
Scl-70
<5
<5
• 28–70
10–18
<5
RNP, ribonucleoprotein;
Chronic Discoid Lupus Erythematosus.
disease with skin manifestations mimic SLE,
face and scalp are usually affected,
Only 5% to 10% of patients develop systemic dis.
35% of patients show a positive ANA test,
Abs to ds DNA are rarely.
skin biopsy show deposition of Ig and C3 at the dermoepidermal junction similar to that in SLE.
Drug-Induced Lupus Erythematosus
SLE –like syndrome may develop in patients receiving hydralazine, procainamide, isoniazid, and d-penicillamine,
Positive ANAs,
Negative ds DNA Abs are rare,
HLA-DR4 allele are at a greater risk
The disease remits after withdrawal of the offending drug.
MORE SYSTEMIC AUTOIMMUNEDISEASES
RHEUMATOID ARTHRITISSJÖGREN SYNDROME
SCLERODERMA (SYSTEMIC SCLEROSIS)
NORMAL Bi-Layered Synovium
↑Destructive Rheumatoid Synovitis
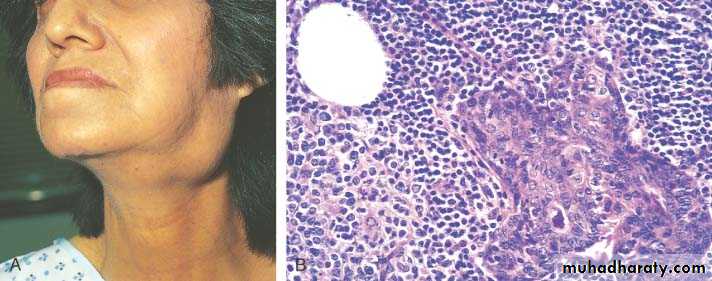
Sjögren syndrome
chronic auto imm. disease,dry eyes (keratoconjunctivitis sicca) and dry mouth (xerostomia)
CD4+T & Ab mediated reaction against epith. Cells of lacrimal and salivary glands.
primary form
secondary form, associated with rheumatoid arthritis SLE, polymyositis, scleroderma, vasculitis, mixed connective tissue disease, or thyroiditis.
Genetic & Environmental factors.
SJÖGREN SYNDROME
SJÖGREN SYNDROME
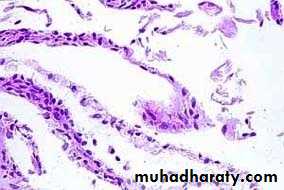
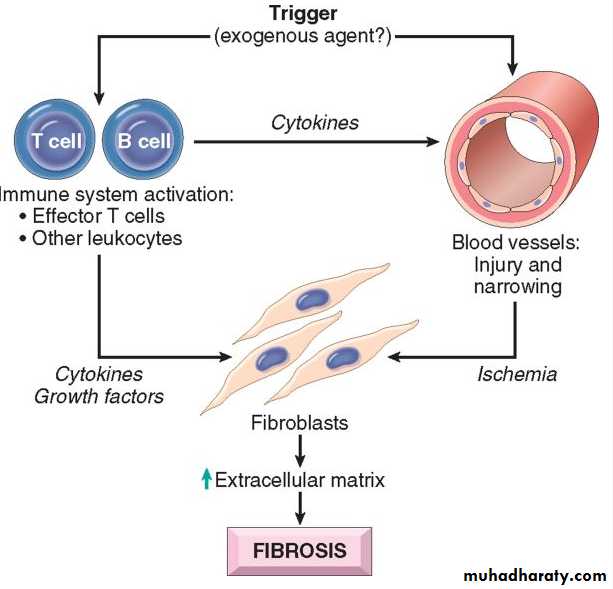
SYSTEMIC SCLEROSIS (SCLERODERMA)1. chronic inflammation
2. widespread damage to small bl ves.
3. progressive fibrosis in skin & organs
Two types;
a. Diffuse type, SS
b. Limited “CREST”
Two ANAs ;
a. Anti DNA topoisomerase I (anti-Scl 70), highly specific. systemic sclerosis.
anticentromere Ab, in CREST or limited sclerosis.
Possible mechanisms leading to systemic sclerosis.
SclerodermaScleroderma
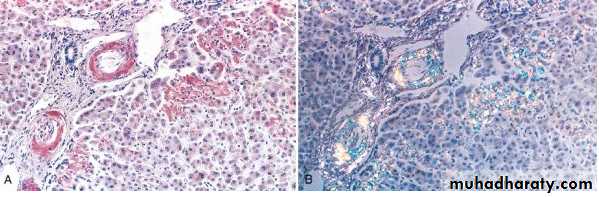
(Collagen Vascular Disease)SYSTEMIC SCLEROSIS
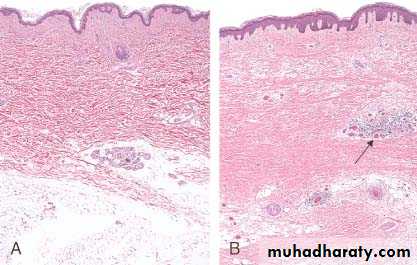
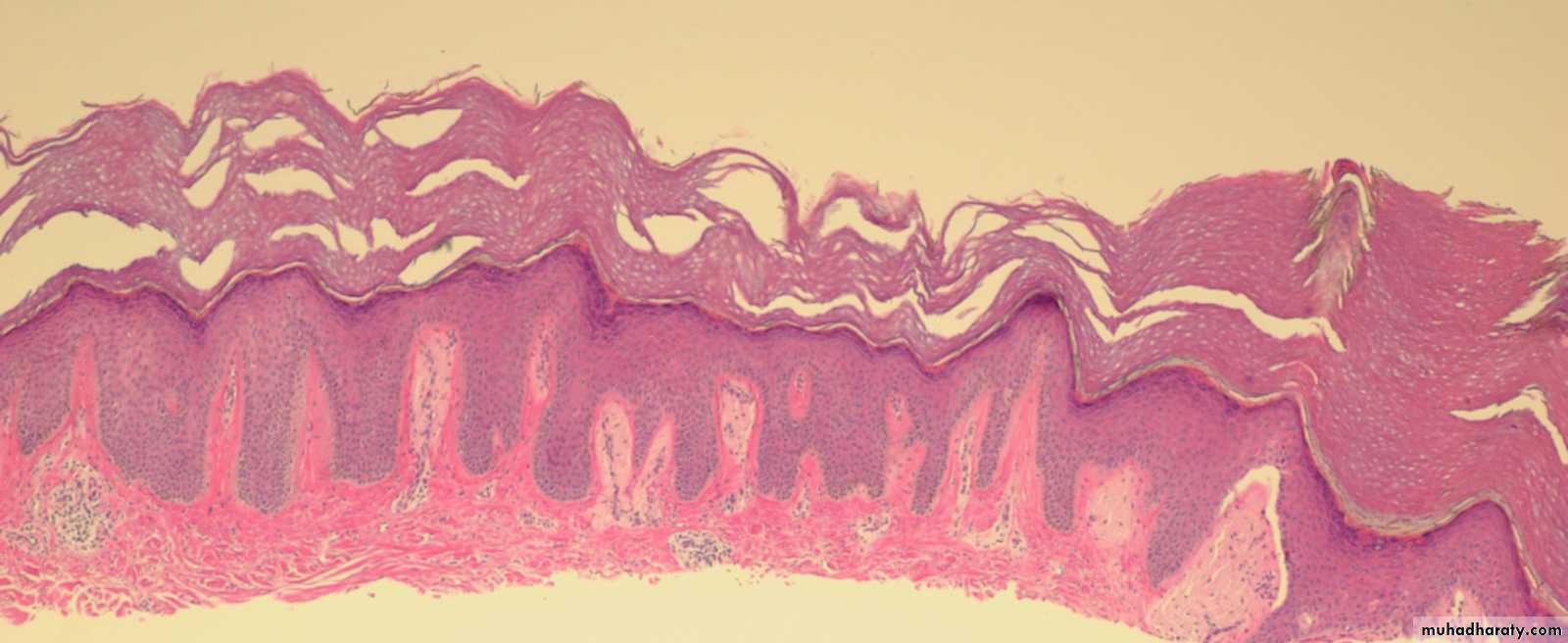
(SCLERODERMA)Systemic sclerosis. A, Normal skin. B, systemic sclerosis. Note the extensive deposition of dense collagen in the dermis with virtual absence of appendages &foci of inflammation (arrow).
PAN
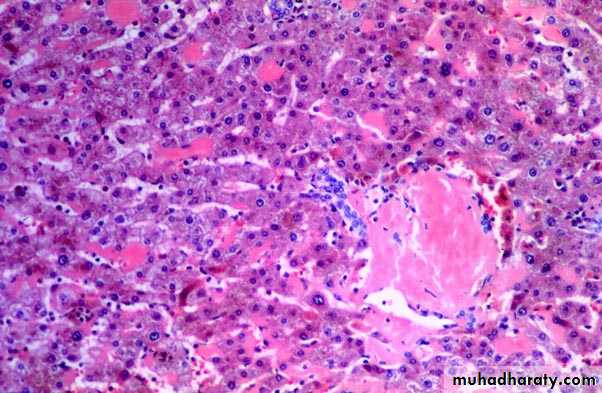
IgG4-RD (Fibroiflammatory disease).
Inflamm.
Fibrosis
Obliterative phlebitis.
Amyloidosis
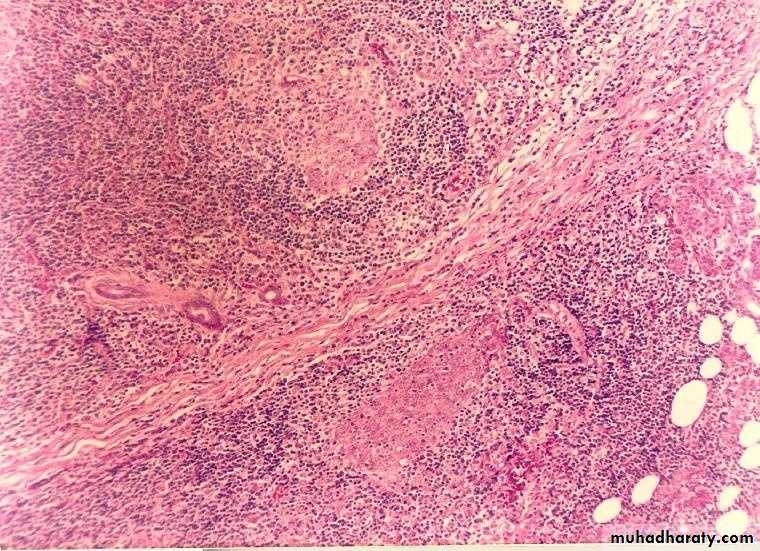
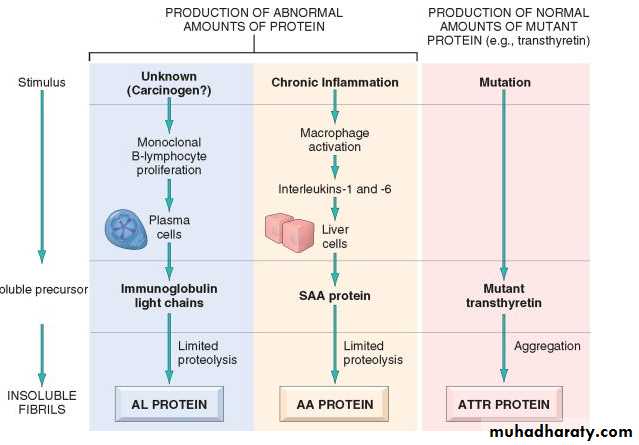
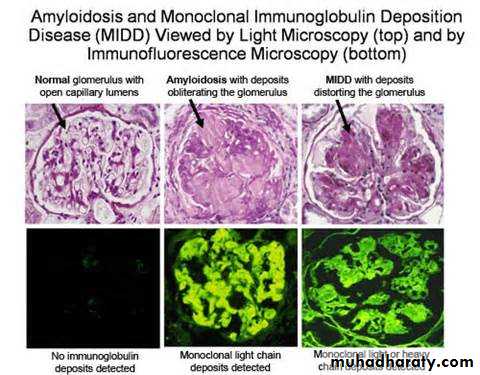
Pathogenesis of AmyloidosisAmyloidosis - abnormal folding of pr., which are deposited as fibrils in EC tissues and disrupt normal function.
The Pr. that form amyloid fall into two general categories:
(1) Normal proteins that have an inherent tendency to fold improperly, and do so when they are produced in increased amounts; and
(2) mutant proteins that are prone to misfolding and subsequent aggregation
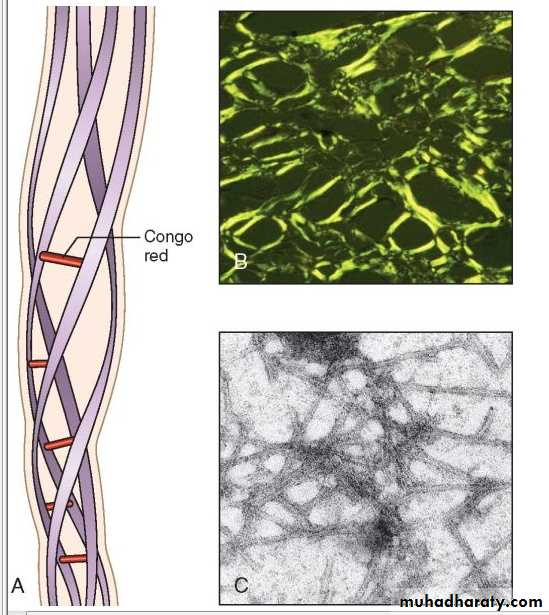
Physical Nature of Amyloid
nonbranching fibrils, 7.5 - 10 nm.cross-β-pleated sheet conformation
Chemical Nature of Amyloid
95% of amyloid material consists of fibril pr,(1) AL (amyloid light chain) is derived from Ig light chains produced in plasma cells;
(2) AA (amyloid-associated) is derived from a unique non-Ig protein synthesized by the liver; and
(3) Aβ amyloid is produced from β amyloid precursor protein and is found in the cerebral lesions of Alzheimer disease.
Classification of Amyloidosis
PrimarySecondary
systemic
LocalizedCongenital
AcquiredPrimary Amyloidosis
Secondary (Reactive) AmyloidosisAA protein.
Systemic amyloidosis,
TB, bronchiectasis, ch. Osteomyelitis.
Rh arthritis, other CT disorders such as ankylosing spondylitis, and IBD.
Heroin abusers
renal cell carcinoma
Hodgkin lymphoma.
Pathogenesis of amyloidosis
Clinicopathologic CategoryAssociated Diseases
Major Fibril Protein
Chemically Related Precursor Protein
SYSTEMIC (GENERALIZED) AMYLOIDOSIS
(primary amyloidosis)
Multiple myeloma andAL
Immunoglobulin light chains,
(secondary amyloidosis)
Chronic inflammatory conditions
AA
SAA
Hemodialysis-associated amyloidosis
Chronic renal failure
Aβ2m
β2-microglobulin
HEREDITARY AMYLOIDOSIS
Familial Mediterranean fever
AA
SAA
Familial amyloidotic neuropathies (several types)
ATTR
TransthyretinSYSTEMIC SENILE AMYLOIDOSIS
ATTR
TransthyretinLOCALIZED AMYLOIDOSIS
Senile cerebral
Alzheimer diseaseAb
APP
Endocrine
A Cal
CalcitoninMedullary carcinoma of thyroid
Type 2 diabetes
AIAPP
Islet amyloid peptide
Islets of Langerhans
AANF
Atrial natriuretic factor
Clinical Features.
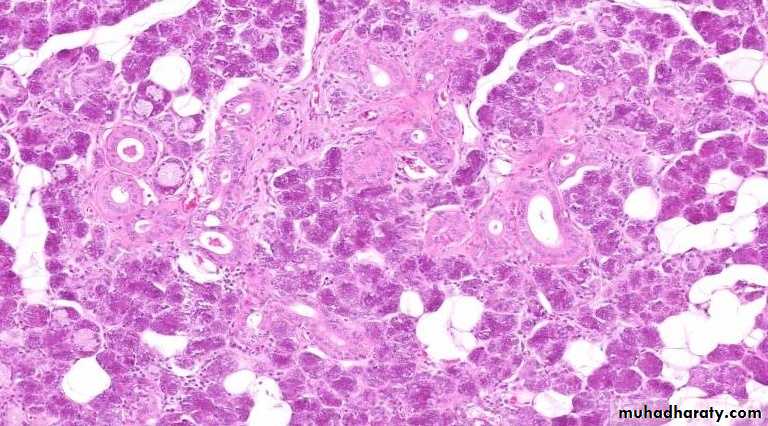
Renal involvement proteinuria, nephrotic syndrome. renal failure and uremia.Cardiac amyloidosis ____congestive heart failure.
Gastrointestinal amyloidosis, Amyloidosis of the tongue.
Depositions in the stomach and intestine may lead to malabsorption, diarrhea, and disturbances in digestion.
Diagnosis of amyloidosis
Biopsy: rectal or gingival tissues in patients suspected of having systemic amyloidosis.Examination of abdominal fat
kidney, when renal manifestations are present
Congo red.
serum and urine protein electrophoresis.
Bone marrow aspirates show monoclonal plasmacytosis,
Radiolabeled serum amyloid P (SAP) binds to the amyloid deposits and reveals their presence.
The prognosis for individuals with generalized amyloidosis is poor.
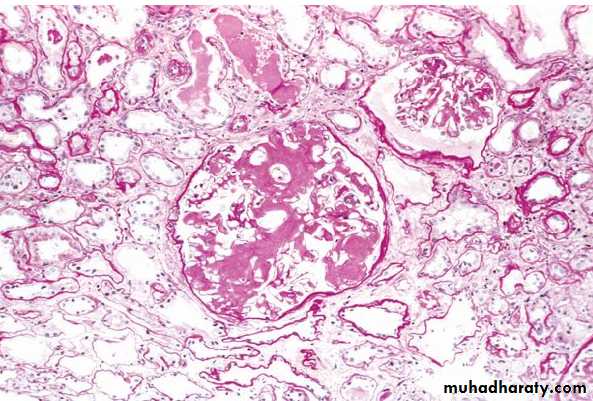
New therapeutic strategies aimed at correcting protein misfolding and inhibiting fibrillogenesis are being developed.Amyloidosis of the kidney. The glomerular architecture is almost totally obliterated by the massive accumulation of amyloid.