Peripheral Vascular Diseases
Assistant prof.Dr.Abdulameer M. Hussein
Objectives
1. Describe the anatomy of the vessels.2. To differentiate between pathophysiology of acute and chronic ischemia.
3. We should know the urgency of acute ischemia.5. To be familiar with methods of investigation in ischemia.
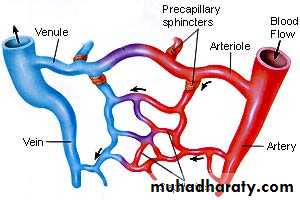
6. To understand the principles of management of acute ischemia.Arteries
• are thick-walled vessels that transport 02 and blood via• the aorta from the heart to the tissues
3 Layers of Arteries
inner layer of endothelium (intima)middle layer of connective tissue, smooth muscle and elastic fibers (media)
outer layer of connective tissue (adventitia)
have smooth muscles that contracts & relaxes to respond changes in blood volume.
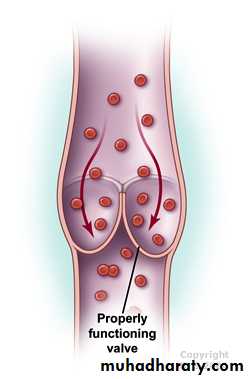
Veins
are thin-walled vessels that transport deoxygenated bloodfrom the capillaries back to the right side of the heart
3 Layers – intima, media, adventitia
there is little smooth muscle &connective tissue makes
the veins more distensible
they accumulate large volumes of blood
Major veins, particularly in the lower
extremities, have one-way valves
---allow blood flow against gravity
Valves allow blood to be pumped back
to the heart but prevent it from
draining back into the periphery
What is an end arteries
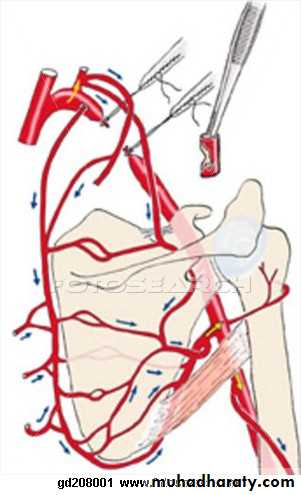
An end artery is an artery that is the only supply of oxygenated blood to a portion of tissue. End arteries are also known as terminal arteries.Collateral CirculationWhat is collateral circulation? This is a process in which small (normally closed) arteries open up and connect two larger arteries or different parts of the same artery. They can serve as alternate routes of blood supply.
Collateral circulation to arm after ligation of the axillary artery Arrows indicate direction of adjusted blood flow.
Investigation of peripheral vascular diseases:
General : peripheral vascular disease (atherosclerosis) is a systemic disease so full investigation is required and this include:blood picture.
Biochemical investigation.
Lipid profile.
ECG.
Echocardiography.
Radiological:
Chest X-ray.
Abdominal X-ray (aortic calcification).CTA scan.
MRI and MRA. (Magnetic resonance angiography).
Doppler study: ultrasound blood flow detection.
The principle of this examination is by applying a continuous wave ultrasound signal which is beamed at an artery and reflected beam picked up by a receiver, presented as a sound waves.
Colored Doppler (duplex scan) which display a real time image of the vessel structure.
Plethysmography : is an instrument for measuring changes in volume within an organ or whole body (usually resulting from fluctuations in the amount of blood or air it contains).Angiography (Arteriography).
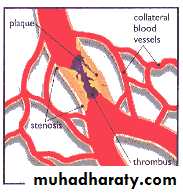
ISCHAEMIAMeans diminish blood supply. It may be acute or chronic according to the speed of arterial occlusion.
The effect of ischemia depends upon:-
1- The type of artery. 2. The rate of occlusion of the artery. 3. The state of the collateral vessels. 4. The general condition of the patient, the presence of MI and anemia will exacerbate the effect of ischemia.Etiology of acute ischaemia
Embolism
Left atrium in patients in atrial fibrillationMural thrombus after myocardial infarct
Prosthetic and diseases heart valves
Aneurysm or atheromatous stenosis
Tumour, foreign body, paradoxical
Thrombosis
Trauma.
Dissecting aneurysm
Raynaud's Syndrome
Clinical features of limb ischaemia
Clinical diagnosis depends on the 5'p' sPain
Paraesthesia
Pallor
Pulselessness
Paralysis
Fixed staining is a late sign
Objective sensory loss requires urgent treatment
Need to differentiate embolism from thrombosis
Important clinical features include
Rapidity of onset of symptoms
Features of pre-existing chronic arterial disease
Potential source of embolus
State of pedal pulses in contralateral leg
Management of acute ischaemia
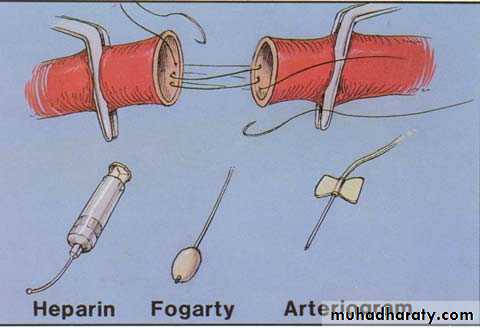
InitialHeparin & analgesia
Correction of fluid and electrolyte disturbance.
Vasodilators.
Treat associated cardiac disease
Treatment options are:
Embolic disease - embolectomy
Thrombotic disease - intra-arterial thrombolysis / angioplasty or bypass surgery
Emergency embolectomy
Can be performed under either general or local anaesthesia
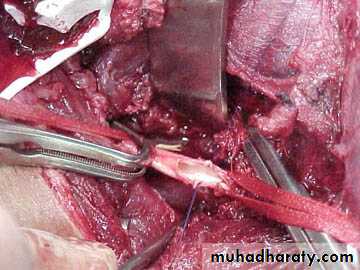
Display and control arteries with slingsTransverse artereotomy performed over common femoral artery
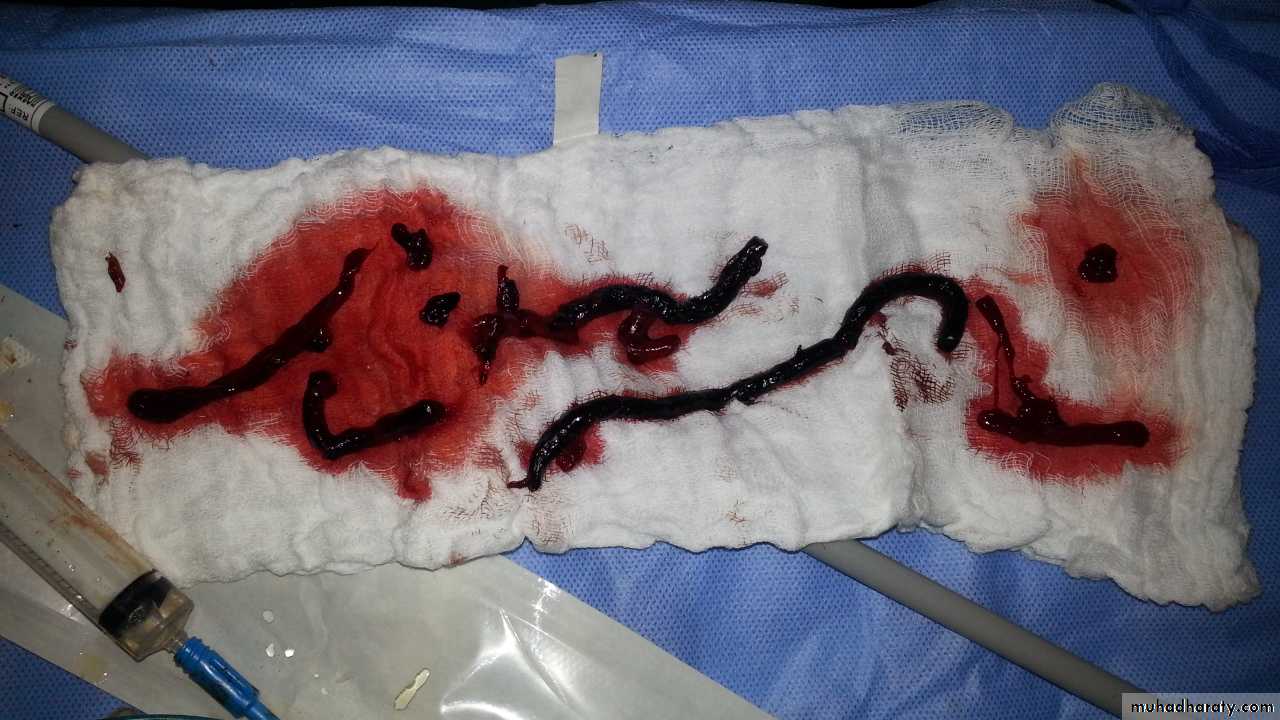
Fogarty balloon embolectomy catheters used to retrieve thrombus
If embolectomy fails - on-table angiogram and consider
Bypass graft or intraoperative thrombolysis
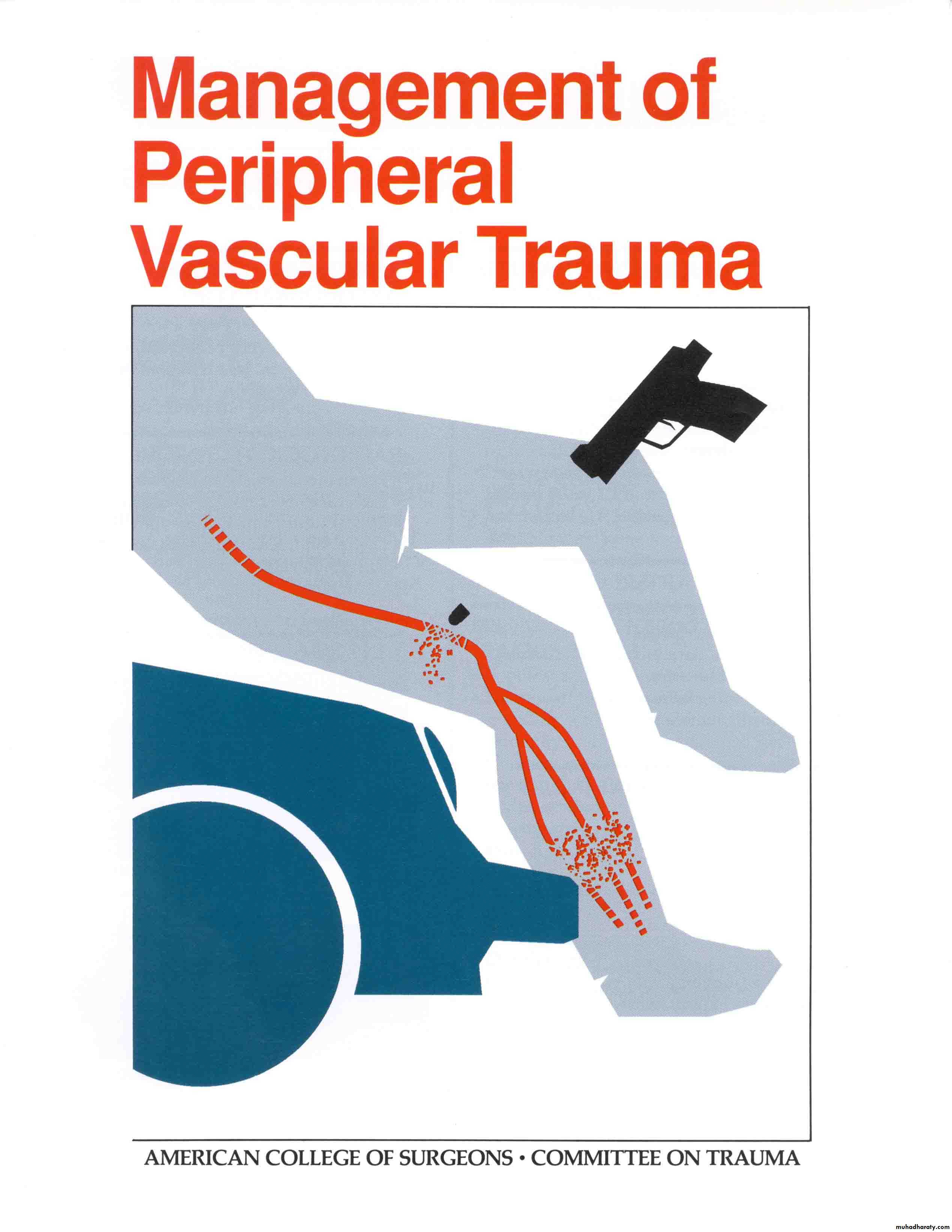
Management of Peripheral Vascular Trauma
CAUSES OF Vascular Trauma•Penetrating wounds
Gunshot, stab, or shotgun
IV drug abuse
•Blunt trauma
Joint displacement
Bone fracture }Adjacent to major artery
Contusion
•Invasive procedures
Arteriography
Cardiac catheterization
Balloon angioplasty
HARD SIGNS OF ARTERIAL INJURY
(Immediate surgery)• External arterial bleeding.
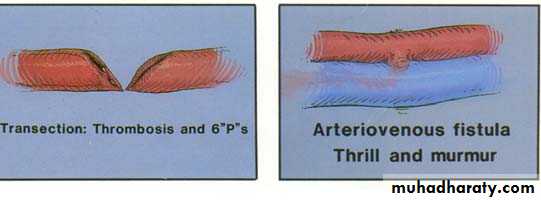
• Rapidly expanding haematoma.• Palpable thrill, audible bruit.
• Obvious arterial occlusion.
SOFT SIGNS OF ARTERIAL INJURY
(Consider arteriogram, serial examination, duplex)• History of arterial bleeding at the scene
• Proximity of penetrating or blunt trauma to major artery
• Diminished unilateral distal pulse
• Small non pulsatile hematoma
• Neurologic deficit
• Abnormal ankle-brachial pressure index (<0.9)
• Abnormal flow-velocity waveform on Doppler ultrasound
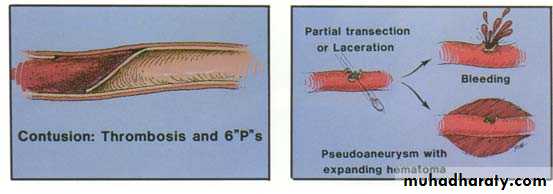
TYPES OF INJURIES
MANAGEMENT
REASONS FOR DIAGNOSTIC STUDIES• Prevent unnecessary operation
• Document presence of surgical lesion
• Localize surgical lesion to plan operative approach
DUPLEX SCANCT ANGIOGRAPH
ARTERIOGRAPHY
Clinical examination and reexamination remain the mainstays for identifying and treating these trauma
TREATMENT
• The priorities of vascular injury are arrest of hemorrhage and restoration of normal circulation.• Airway control and respiratory assessment take priority over management of the circulation.
• Volume resuscitation before & after } hemorrhage control.
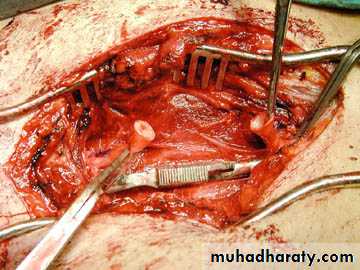
Operative Strategy
OPTIONS FOR PERIPHERAL VASCULAR REPAIR• Lateral arteriorrhaphy or venorrhaphy
• Patch angioplasty
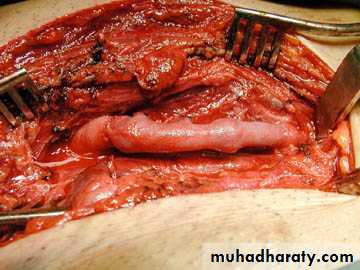
• Resection with end-to-end anastomosis
• Resection with interposition graft
• Bypass graft
• Extraanatomic bypass
• Ligation
(Intraluminal shunts may be employed to temporarily restore flow).
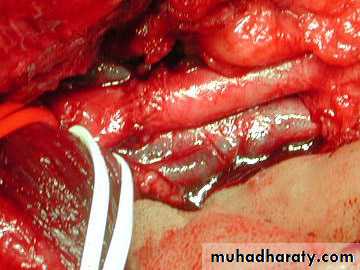
ShuntingReversed vein graft to transected common femoral artery
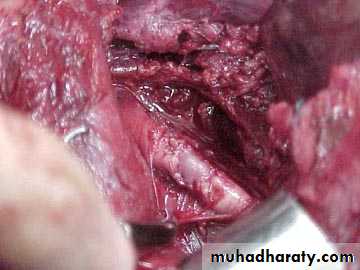
Vein patch to carotid artery
Vein patch to carotid artery
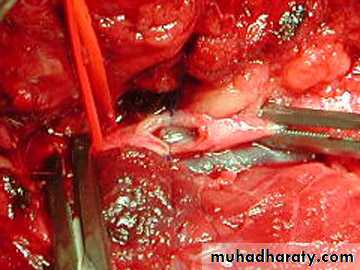
End-to-end anastomosis of transected popliteal artery.
End-to-end anastomosis of transected popliteal artery.
SPECIAL CONSIDERATIONS FOR VENOUS REPAIR• Popliteal vein is repaired rather than ligated
• Ligation of femoral or iliac vein, if necessary, is usually tolerated if elastic wraps are applied to extremity, which is elevated for 7–10 days
• Complex venous repairs functions temporary conduits in many patients but often show narrowing or occlusion on later venograms
Complications
These are considerable and may occur in up to 30% of cases.The major complications are
Thrombosis
Infection
Bleeding.
Stenosis.
Completion angiography, the use of only autologous material for repair and adequate soft tissue coverage are the means to decrease these risks.