Genus Neisseria
Department of MicrobiologyCollege of Medicine
Baghdad University
Lec. 4, 2013-2014
Dr. Sarmad Zeiny
Objectives:
Describe the morphology & physiology for genus Neisseria.Determine the virulence factors for genus Neisseria.
Analyze the diseases & pathogenicity for genus Neisseria.
Demonstrate the epidemiology/transmission for genus Neisseria.
Outline the laboratory diagnosis for genus Neisseria.
State the drug of choice and prophylaxis where regularly used.
Genus neisseria
PATHOGENIC:NON-PATHOGENIC:
• N. gonorrhoeae (gonococci, G.C).
• N. meningitidis (meningococci).
• N. catarrhalis.
N. sicca, others
General characteristics
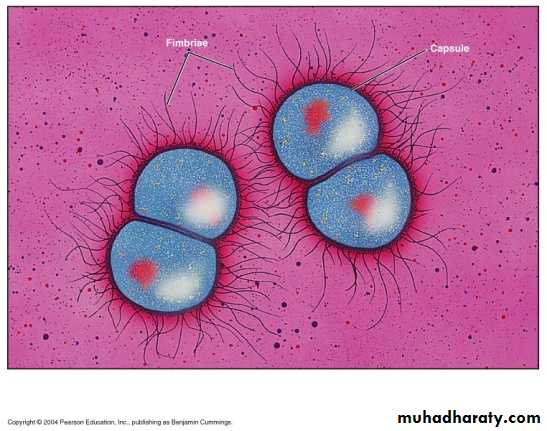
• G –ve diplococci, kidney (coffee bean) shape, with flat• opposing edge.
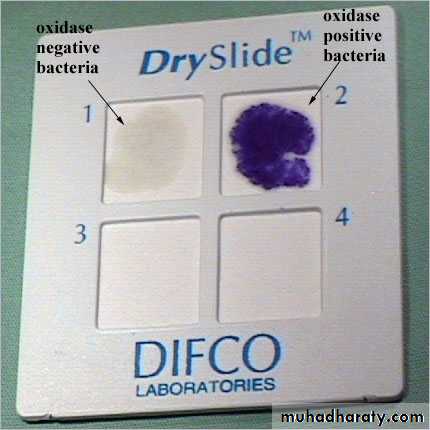
• All members are Oxidase positive.
• Pathogenic to human only.
• Ferment carbohydrates.
• Pyogenic: produce pus.
• Non – haemolytics.
Continuation of general characteristics
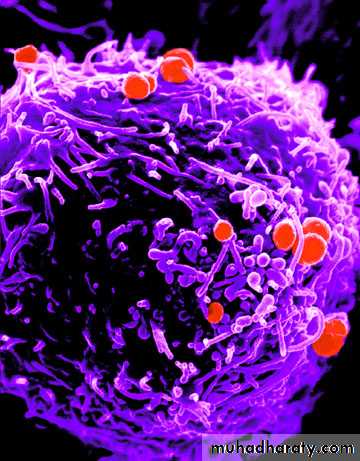
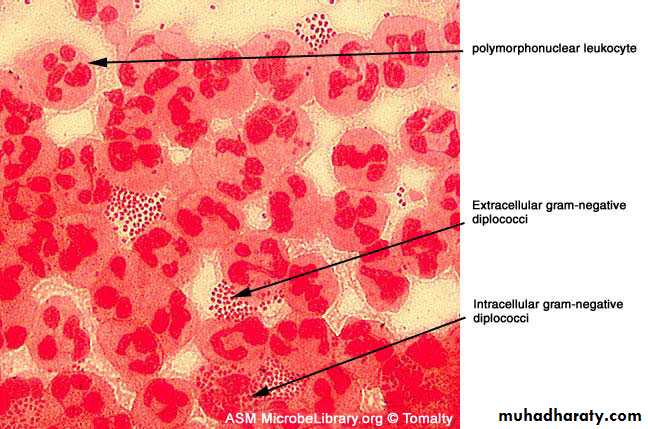
Intracellular &/or extracellular.Needs 48h of culturing time.
They are rapidly killed by drying, sunlight and many disinfectants.
70% DNA homology and are differentiated by few LAB tests.
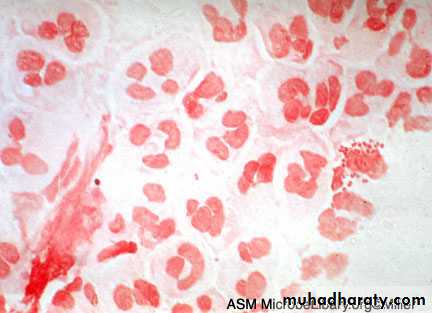
Gram’s negativeDiplococci
Kidney (coffee bean) shape with flat opposing edge
Neisseria
Neisseria attached to lymphocyte
By Electronic MicroscopyDirect Gram’s staining slide from urethral swab
Neisseria gonorrhoeae (gonococcus)
Reservoir: human genital tract
Transmission
Sexual contact, birth
Sensitive to drying and cold
Disease: gonorrhea (STD)
Localized infection.
Systemic infection.
Gonorrhea
GonorrheaOphthalmia neonatorum
Antigenic & Virulence structures:
• Pilli:Attachment to mucosal surfaces.
Inhibit phagocytic uptake.
Antigenic (immunogenic) variation:> 1 million variants
• Porin (por) protein (protein I):
• Opacity (Opa) proteins (protein II): Attachment
• RMP (protein III):
It is associated with (Opa) protein in the formation of pores.
• Lipooligosaccharide (LOS): endotoxic effect.
IgA protease:
Treatment
More than 20 percent of current isolates of N. gonorrhoeae are resistant to penicillin.A single intramuscular dose of ceftriaxone is the recommended therapy for uncomplicated gonococcal infections.
Prevention of gonorrhea :
Antibiotic prophylactically in an exposed individual even in the absence of symptoms.The use of barrier methods is also a preventive measure against gonorrhea as is the case for all sexually transmitted infections.
No vaccine is available for gonorrhea.
Neisseria meningitidis (meningococcus)
Distinguishing Features
Gram-negative, kidney coffee bean-shaped diplococci.
Large capsule, Antigenic.
Grows on chocolate (not blood) agar in 5% C02 atmosphere.
Ferments maltose in contrast to gonococci.
Reservoir: human nasopharynx (5-10% carriers).
Transmission:
Respiratory droplets; oropharyngeal colonization, spreads to the meninges via the bloodstream
Antigenic & Virulence structures:
• Capsule: At least 13 serogroups most important serogroups are A,B,C,Y, W135 .• Outer membrane protein (OMP):about 20 antigenic types, used for serotyping.
• Pilli: attachment
• IgA protease: cleaves IgA
• Opa protein: attachment
• Lipooligopolysaccharide (Endotoxin) : fever, septic shock in meningococcemia.
Q) Answer with true or false:
The important Criteria for genus Neisseria are:• Gram –ve diplococci.
• Kidney shaped diplococci.
• Oxidase positive.
The answer: all above are true.
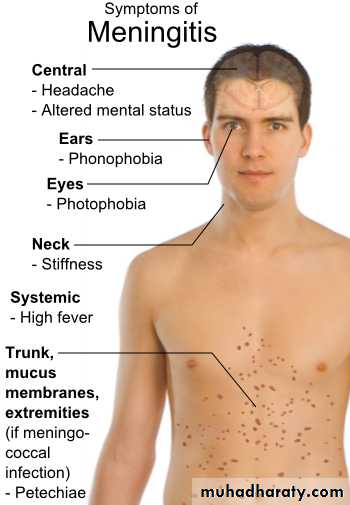
Diseases & Pathogenicity
The source of the infection is either the patient or the carriers.The route of entry is through the nasopharynx by droplet.
Attach to the epithelia then spread through the blood stream:
• Meningitis: mainly in adult ages 11 to 55 years.
• Fulminating meningococcemia.
Fulminating meningococcemia
Risk factors :• Recent viral or mycoplasma upper respiratory tract infection,
• Active or passive smoking, and
• Complement deficiency (C5-C8).
Treatment:
Medical emergency.
Penicillin G is the drug of choice.
Chloramphenicol and cefotaxime (or ceftriaxone) can be used.
Prevention
Irradiation of the carrier states (major source).Isolation of the patient.
Chemoprophylaxis for contact people.
Vaccination: used in adolescents and adults ages 11 to 55 years. Against A, C, W-135, and Y conjugated to diphtheria toxoid.
Moraxella catarrhalis
Neisseria catarrhalis, Branhamella and now they are a separated genus “Moraxella”.Normally found in upper respiratory tract especially among school children. (50% of school children carry this microorganism)
May cause pneumonia, otitis media, sinusitis and other infections.
Oxidase positive.
Non fastidious organisms can grow on nutrient agar.
Laboratory Diagnosis steps
Laboratory Diagnosis:1) Specimens:
CSF, Blood , throat swab meningococcal inf.
High vaginal swab, urethral discharge and urine deposit G.C. inf.
2) Gram's stain:
G – ve, diplococci
Intracellular &/or extracellular.
Note : Urethral swab for male is diagnostic, but High vaginal swab for female need confirmation, why?
Direct Gram’s staining slide from urethral swab
Gram’s staining slide for urethral discharge
3) CULTURE :
Pathogenic fastidious need chocolate agar, selective media.Non – pathogenic non fastidious can grow on nutrient media.
Selective media for Neisseria
• Thayer Martin (TM).• Modified Thayer Martin.
• Martin – Lewis (ML).
• New York City (NYC).
Biochemical tests
1) Oxidase test+ ve for all Neisseria spp.
2) Sugar fermentation test
SucroseMaltose
Glucose
N. spp.
ـــ
+
+
N. meningitidis
ـــ
ـــ
+
N. gonorrhoea
ـــ
ـــ
ـــ
N. catarrhalis
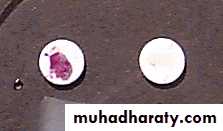
3) Nitrate reduction Nitrite.
+ ve Moraxella catarrhalis.
- ve Other Neisseria spp
HOW DIFFERENTIATE BETWEEN PATHOGENIC AND NON PATHOGENIC Neisseria?• Sugar fermentation test.
• Nitrate reduction test.
• PCR.
Serology
• Serology for G.C:It is not of great value in the diagnosis to detect ANTIBODIES ?
So it is more important to detect gonococcal ANTIGENS using a technique called (ELISA) or using radioimmunoassay (RIA).
Rapid detection methods (detect Ag)
N. meningitidis C.S.F Latex agglutination test.N. gonorrhoea urethral discharge ELISA, DNA probe (molecular assay) e.g. PCR.
Serogrouping for N. meningitidis.Latex agglutination test specific antisera for each 13 serogroups. (The most prevalent serogroups are A, B, C, W135, and Y)
Summary/ conclusions:
Neisseria are G-ve diplococci.
Neisseria are oxidase positive bacteria.
Pathogenic and non-pathogenic species can be differentiated by sugar fermentation, nitrate reduction and PCR.
Gonococci is highly antigenic variable due to pilli antigenic variation.
Meningococci is capsulated with 13 serogroups of that capsule.
Neisseria species are sensitive to pencillins and cephalosporins.
Vaccine against most virulent strain of meningococci are given to high risk groups.