Glaucoma
GlaucomaThe term glaucoma refers to a group of diseases that have in common :
A characteristic optic neuropathy
Associated visual field loss
Intraocular pressure is usually a key modifying factor .
The intraocular pressure (IOP)
The accepted range of IOP in the general population is 10-21 mmHg.Normal physiological variations in IOP (1-2 mmHg), varies with :
Respiration .
BP, heartbeats .
Time of day (maximum in the morning).
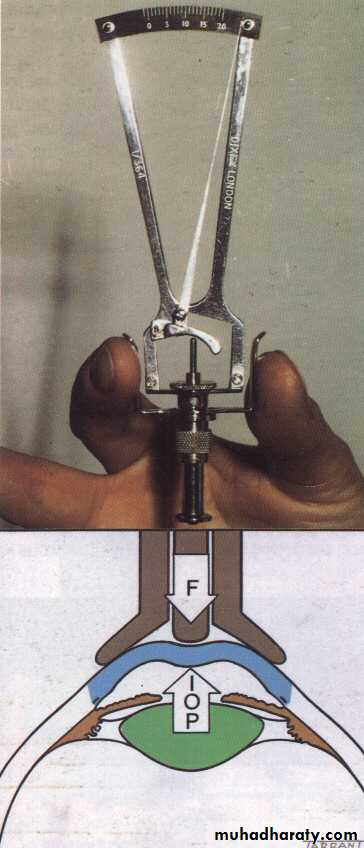
IOP measured by:
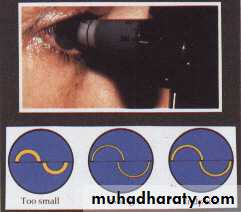
-Indentation tonometry: Schiotz tonometry .
-Applanation tonometry: Goldmann tonometry
Eye ball can be considered as a closed system with relatively constant contents, except the aqueous humor.
The continuous turnover of aqueous is the main determinant of IOP.
Three factors determine the IOP
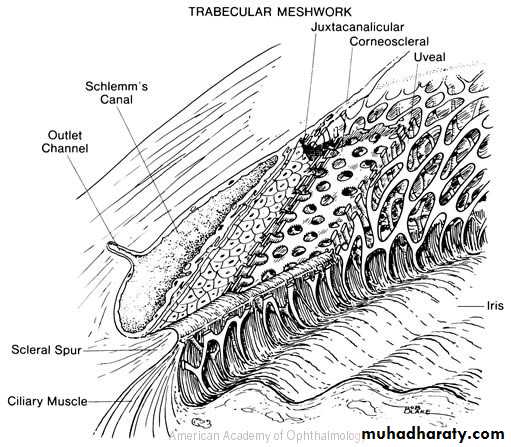
The rate of aqueous humor production by the ciliary body .Resistance to the aqueous outflow across the trabecular meshwork – Schlemm’s canal system .
The level of episcleral venous pressure .
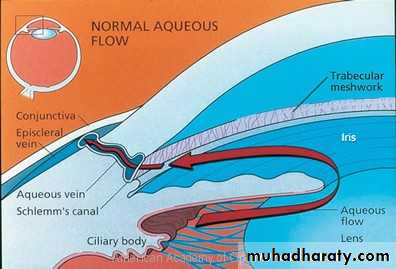
Aqueous Pathway:
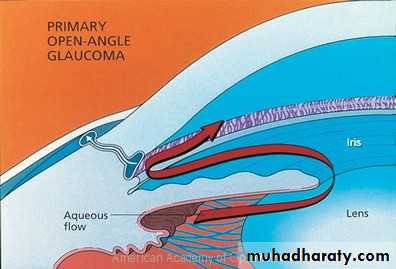
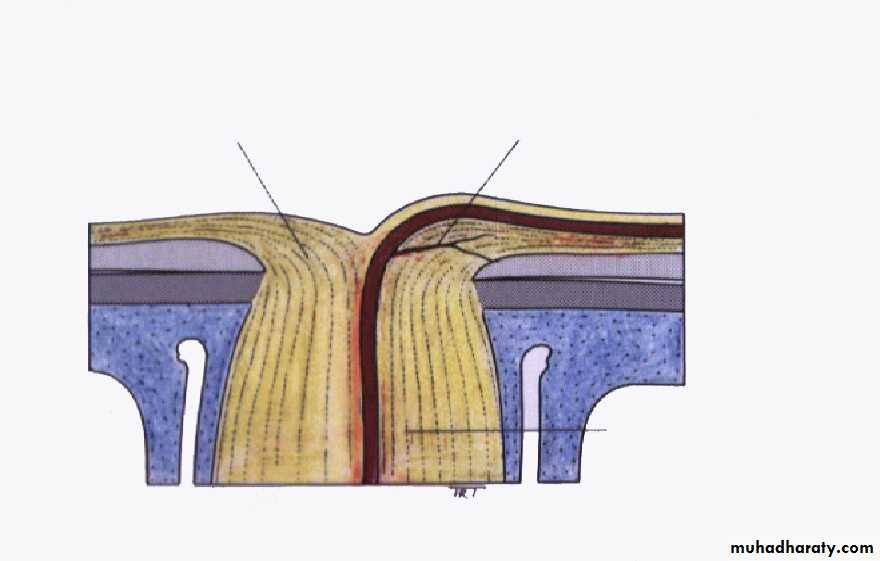
Aqueous is produced from ciliary processes into the posterior chamber, passes through the pupil into the anterior chamber and leave the eye through:Angle of anterior chamber ( 90%) the aqueous passes across trabecular meshwork into canal of schlemm, and then drained by the episcleral veins.
Uveoscleral route (10%) the aqueous passes across the ciliary body into the suprachoroidal spaces and is drained by the venous circulation
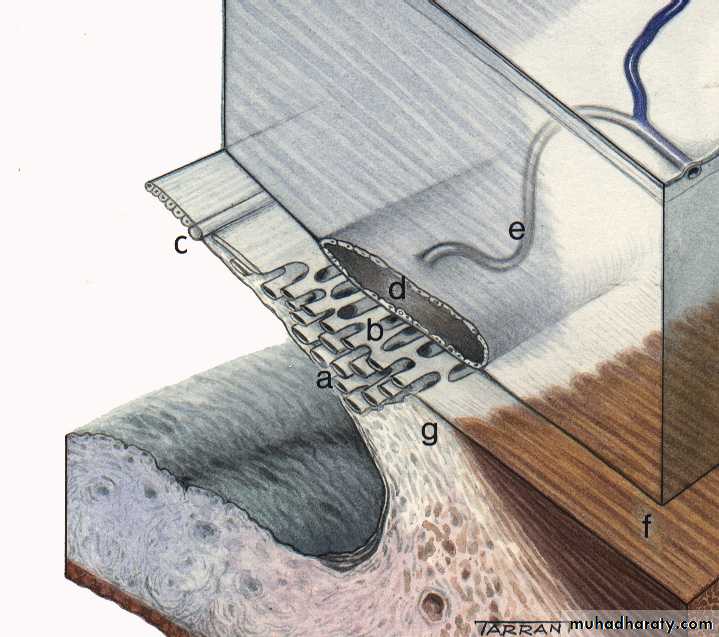
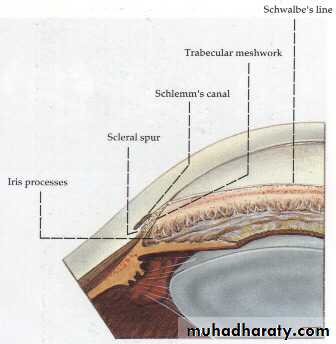
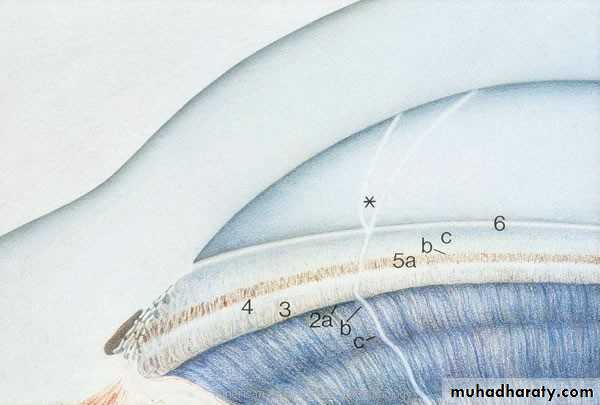
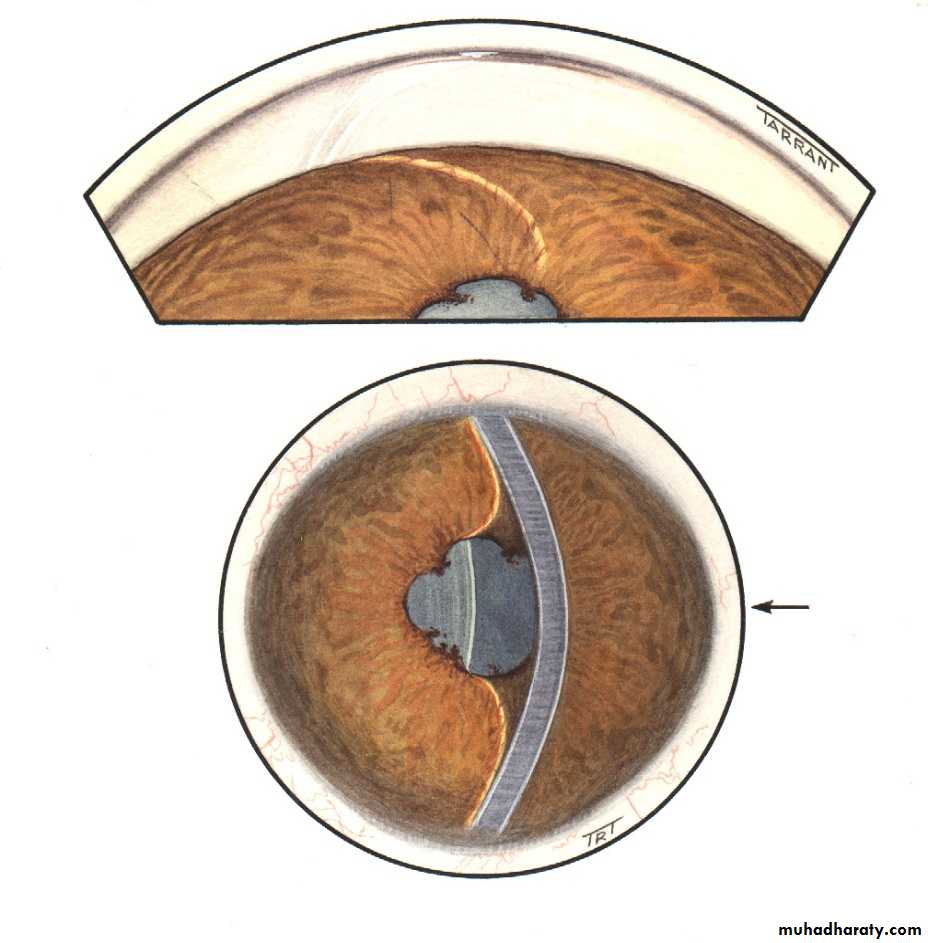
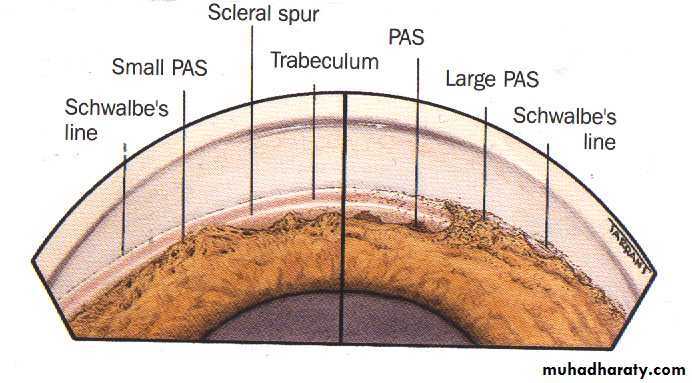
Angle of the anterior chamber :
The angle between the posterior surface of the cornea and the anterior surface of the iris.At the angle there is a circumferential porous meshwork about 1 mm in width called Trabecular meshwork , through which aqueous drained from the anterior chamber to canal of Schlemm
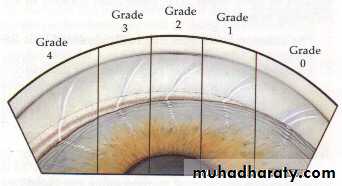
The configuration of the angle indicate the pathogenesis of glaucoma.
Contact between the peripheral iris and the cornea signifies a closed angle .
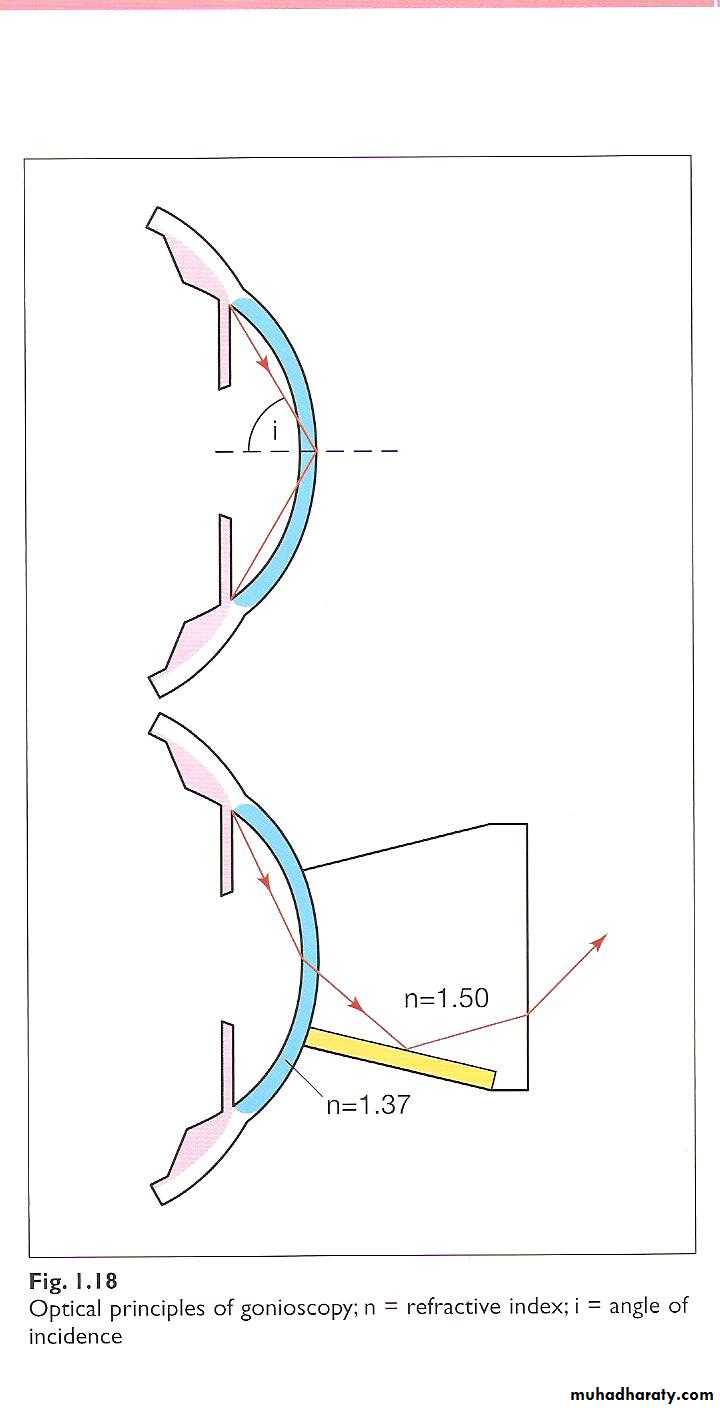
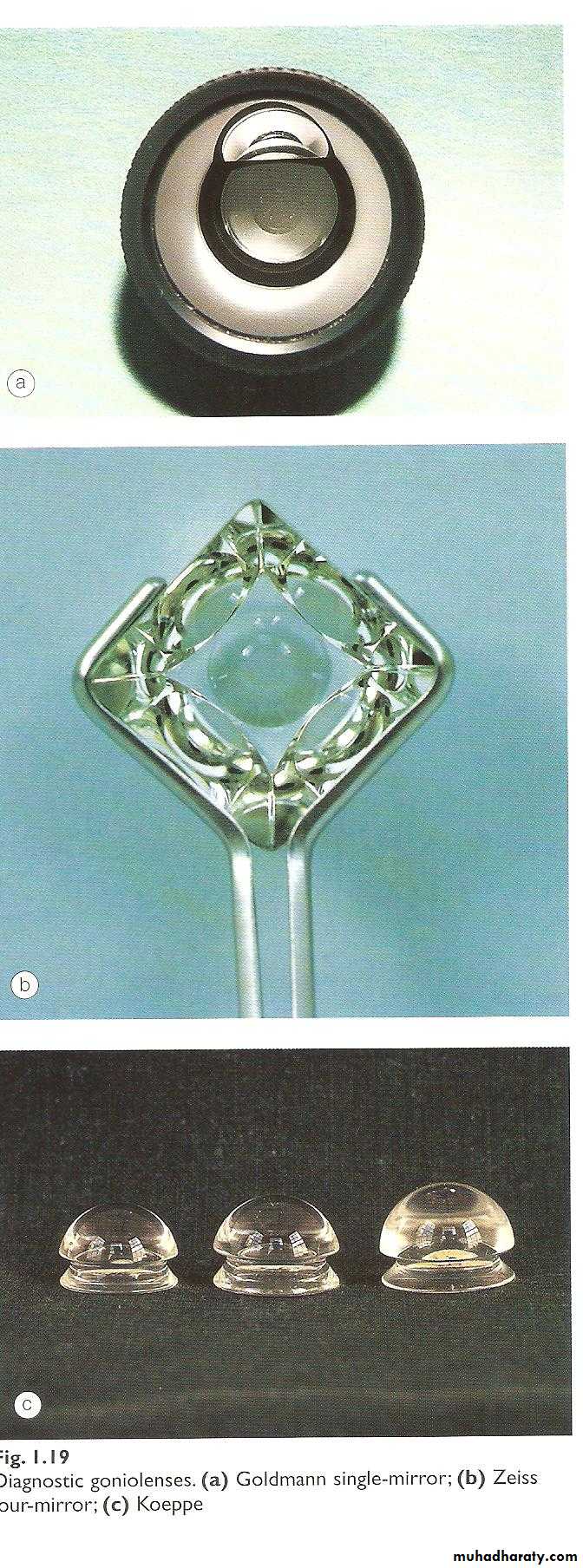
while wide separation between the two indicate open angle .Gonioscopy:
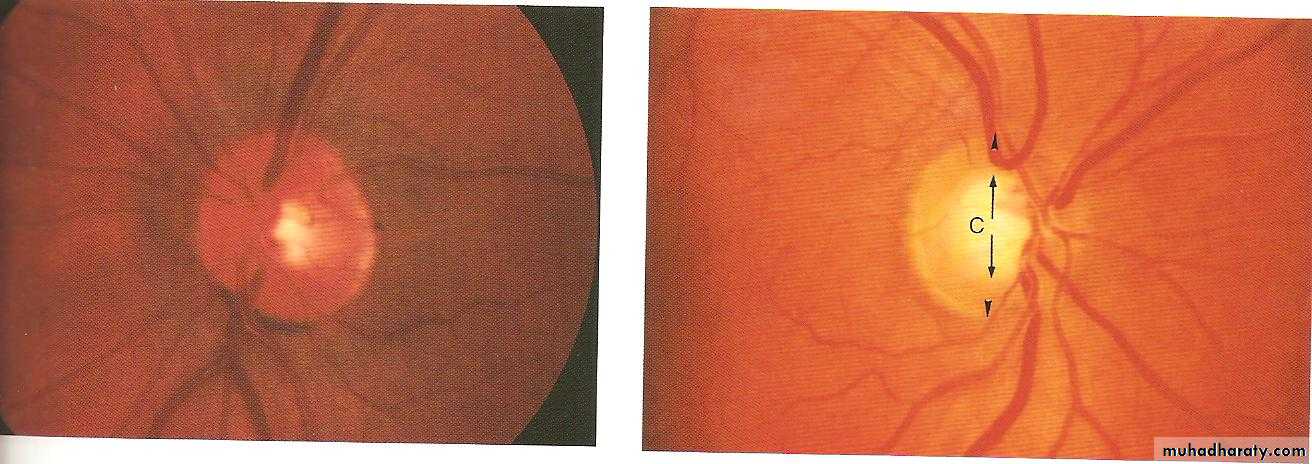
Examination of the angle of the anterior chamber performed by goniolensesOptic disc:
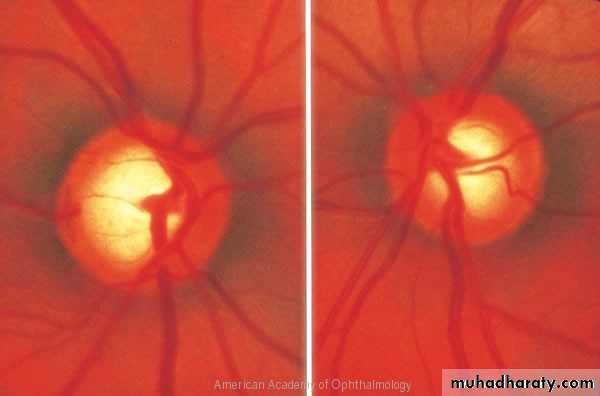
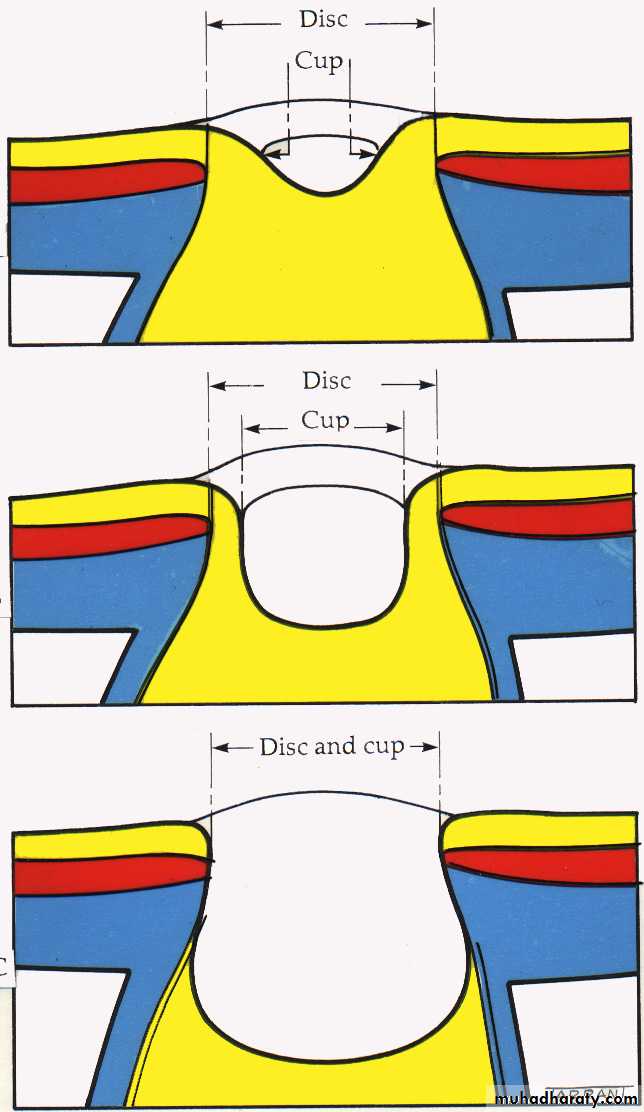
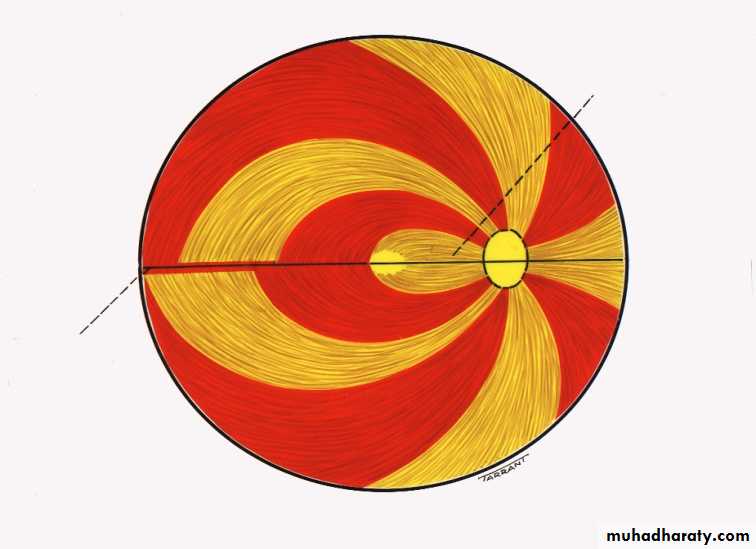
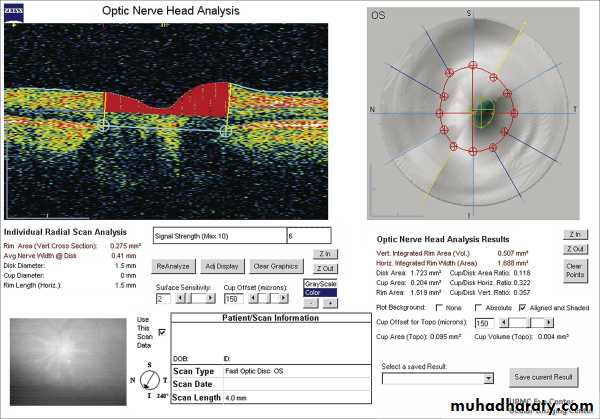
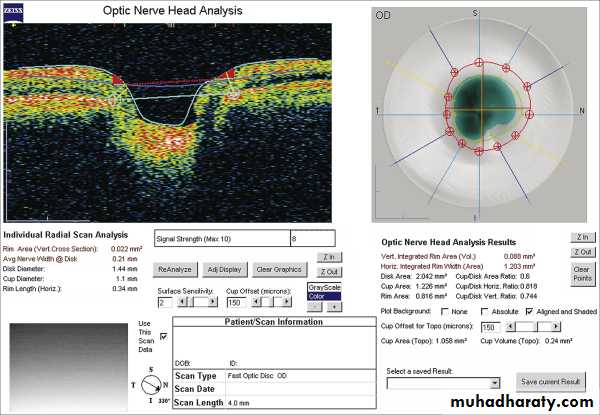
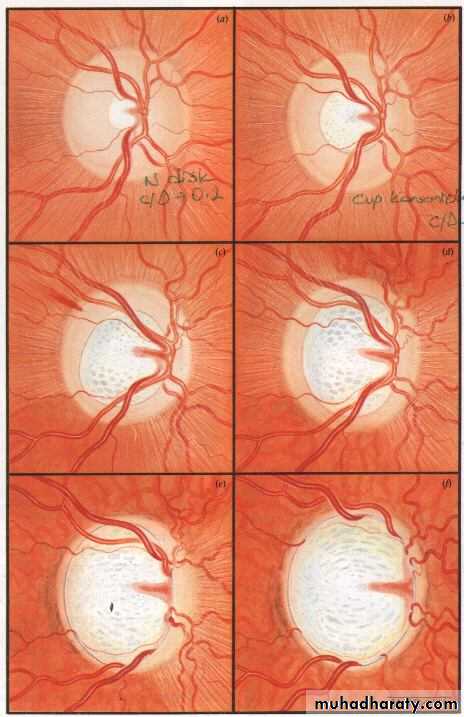
Anterior end of the optic nerve, about 1.5 mm in diameter. Lies about 3mm from the fovea. All retinal layers except the nerve fiber layer stop at the margin of the optic disc. The nerve fiber layer pass through the lamina cribrosa a sieve like structure, bridge the posterior scleral foramen.Optic cup; central depression in the optic disc not occupied by neural tissue.
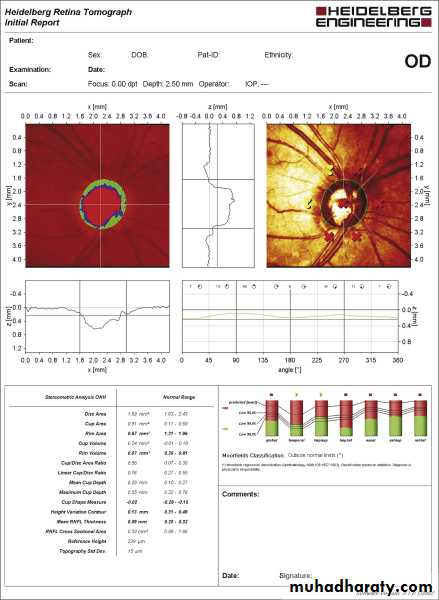
Cup/Disc ratio in most normal eyes is 0.3 or less, asymmetry of 0.2 or more is suspicion.
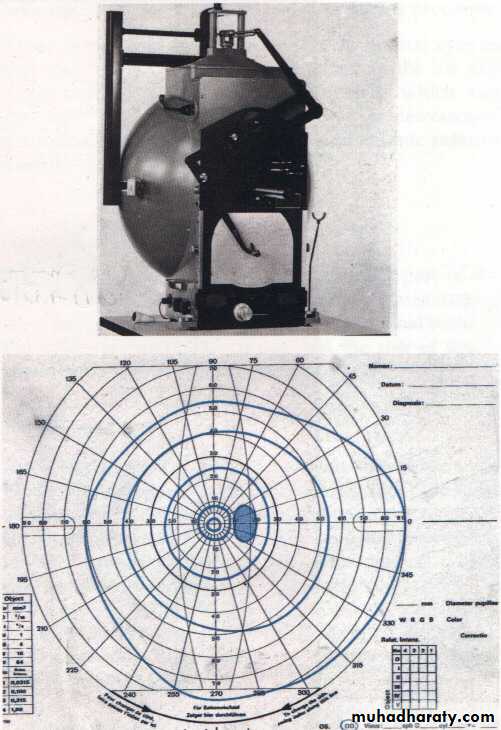
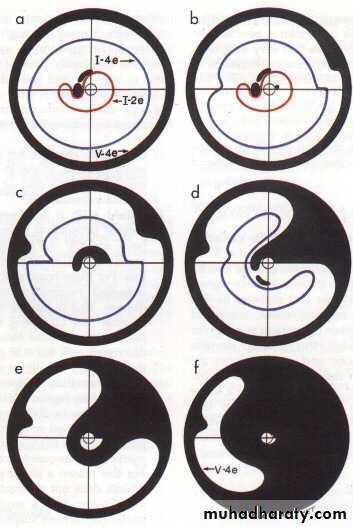
Visual Field
Classification of glaucoma:
Open angle glaucomaPrimary open angle glaucoma
Secondary open angle glaucoma
Closed angle glaucoma
Primary closed angle glaucomaSecondary closed angle glaucoma
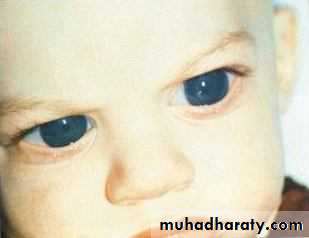
Congenital glaucoma
BuphthalmusPrimary glaucomas are not associated with ocular or systemic disorders that cause increase resistance to aqueous outflow.
Primary glaucomas usually affect both eyes and may be inherited.
Secondary glaucomas are associated with ocular or systemic disorders that are responsible for increase resistance to aqueous outflow.
Secondary glaucomas are usually unilateral and not inherited.
Primary Open Angle Glaucoma (POAG)
Definition : is generally bilateral disease (although not nessessarly a symmetrical disease ) of adult onset .
characterized by :
An IOP > 21 mmHg at some stage .
Glaucomatous optic nerve damage .
An open anterior chamber angle .
Characteristic visual field loss as the damage progress .
Increase IOP caused by increase resistant to aqueous outflow due to thickening of the trabecular meshwork lamellae, with reduce in the pores size.
Theories of glaucomatous damage
Direct damage by pressure
Capillary occlusionInterference with
axoplasmic flow
Risk factors
1- Age
2- Race: more common and a more severe in Blacks .
3- Family history and inheritance.
4- Myopia: increased incidence of POAG.
5- D.M and vascular disease .
Diagnosis
History• Visual symptom will usually be absent , unless damage is advanced .
• Previous ophthalmic history (Refractive status and causes of secondary glaucoma )
• F.H
• PMH
• Current medication and allergies .
• Examination
• V.A
• Pupil
• SLE
• Tonometry noting the time of the day
• Gonioscopy
• Optic disc examination
• Perimetry
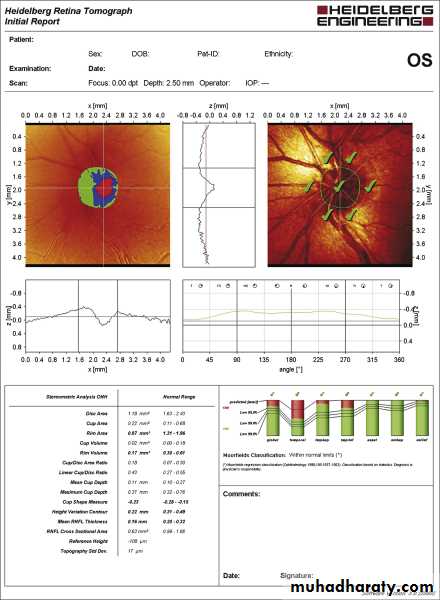
• Optic disc or peripapillary RNFL imaging .
IOP > 21mmHg is suspicious .
Optic nerve head damage : Increase in cup/disc ratio.
Most normal eyes have cup/disc of 0.3 or lessIncrease in cup/disc ratio or asymmetry between two eyes of 0.2 or more is suspicion.
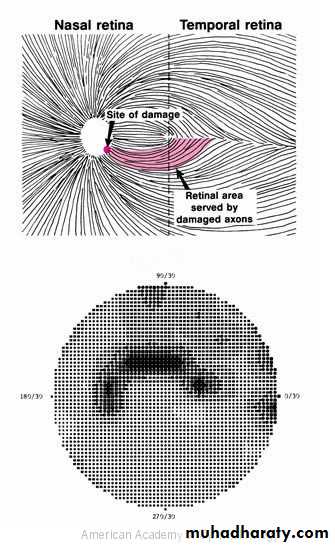
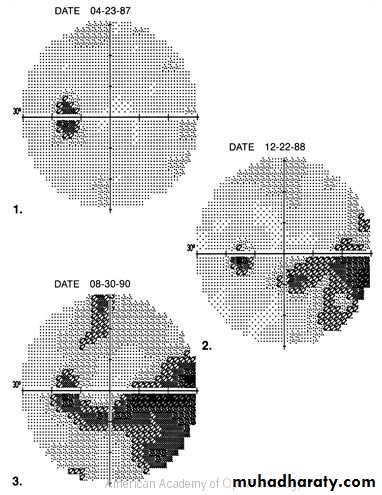
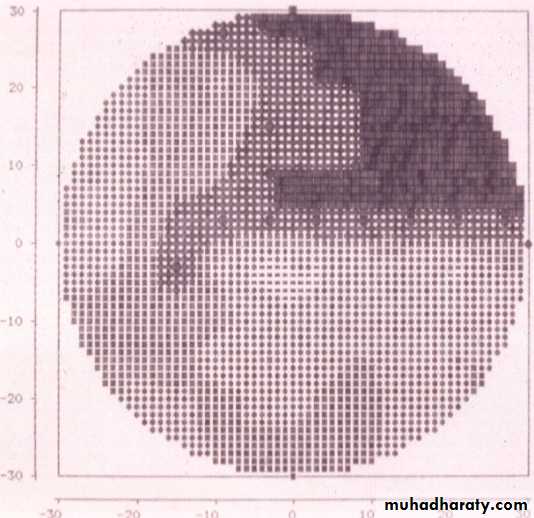
Visual field defects :Paracentral scotoma .
arcuate scotoma .
peripheral field loss with nasal step
generalized visual loss, leaving small central vision which is lost at the end
Open angle assessed by gonioscopy
IOP > 21 mmHg
Glaucomatous disc damageOpen angle of normal appearance
Visual field loss
Management:
The aim of management is to reduced IOP to the target pressure (safe pressure) at which no further damage occurs.Continuous follow up with checking IOP, examination of the optic disc and assessment of the visual field is essential.
Initially primary open angle glaucoma is treated medically with topical eye-drops, but if IOP is not reduced to the target pressure then laser therapy or surgery has to be considered
Treatment:
Medical:A-Beta adrenergic blocking drugs .
Mode of action: decrease the aqueous production e.g. Timolol 0.5% eye drops
B-Topical carbonic anhydrase inhibitors;
Mode of action: decrease the aqueous production e.g. Dorzolmide2% eye dropsC- Cholinergic drug
Mode of action: increase the aqueous outflow e.g. Pilocarpine 2% eye dropsD- Sympathomimetics drugs;
Mode of action: decrease the aqueous production and increase uveoscleral aqueous outflow e.g. Brimonidine 0.2% eye dropsE- Prostaglandin derivatives
Mode of action: increase uveoscleral aqueous outflow e.g. Latanoprost eye drops2- Laser Trabeculoplasty is a procedure by which the application of discrete burns to the trabeculum meshwork enhance aqueous outflow and lower IOP.
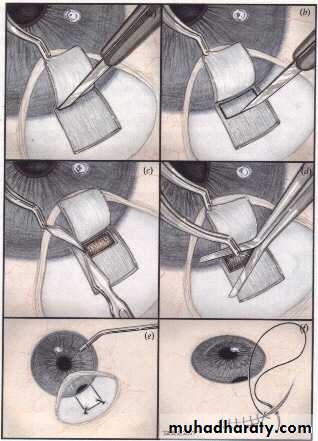
3- Surgical : Trabeculectomy (creating a fistula between the anterior chamber and sub-Tenon space to by pass the trabecular meshwork.
Secondary Open Angle Glaucoma
Angle is open, but the trabecular meshwork blocked by:Blood (hyphaema) following trauma
Inflammatory cells(iritis)
Pigment from the post pigment epithelium of the iris(pigment dispersion syndrome)
Deposition of amyloid- like substance (pseudoexfoliative syndrome)
Drug induced (steroid induced glaucoma)
Ocular hypertension;
IOP>21 without optic disc cupping and visual field defect.7% of the general population above 40 have IOP>21 only 1% of them have glaucoma.
Normal tension glaucoma;
patients with IOP= or <21mmHg with optic disc cupping and visual field defect.
Primary angle closure glaucoma (PACG)
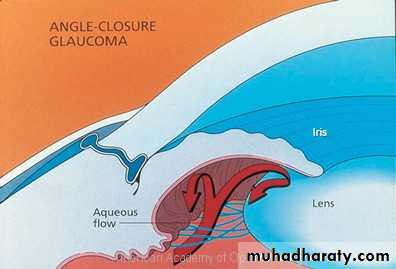
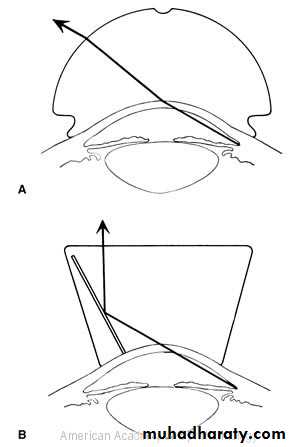
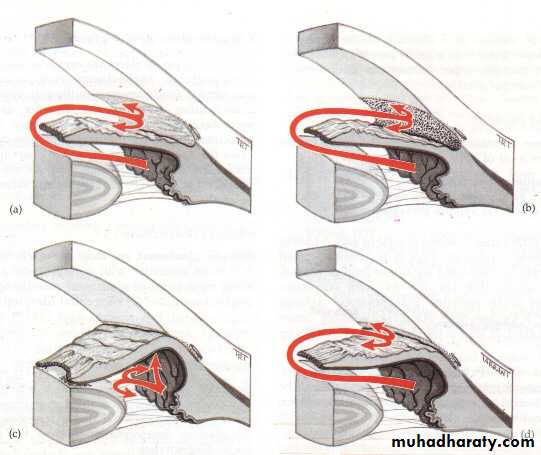
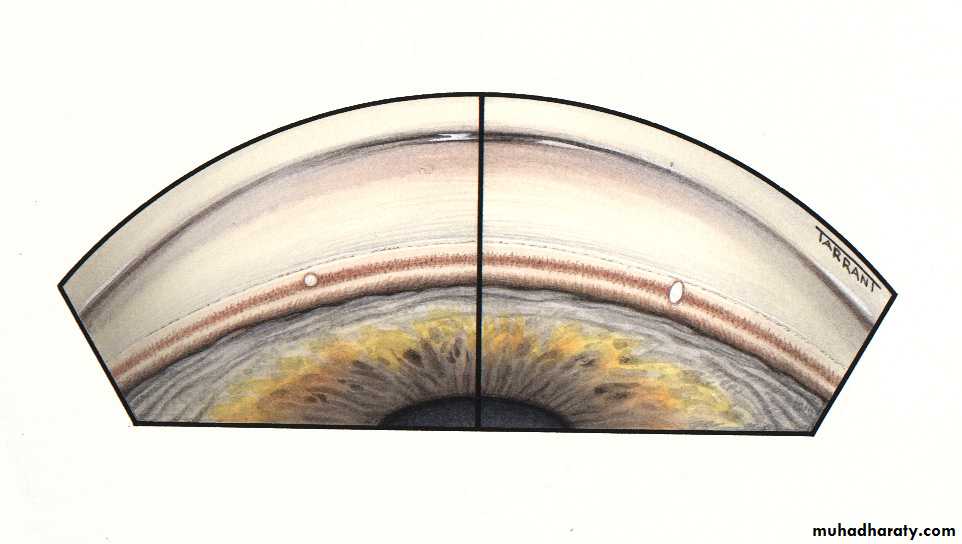
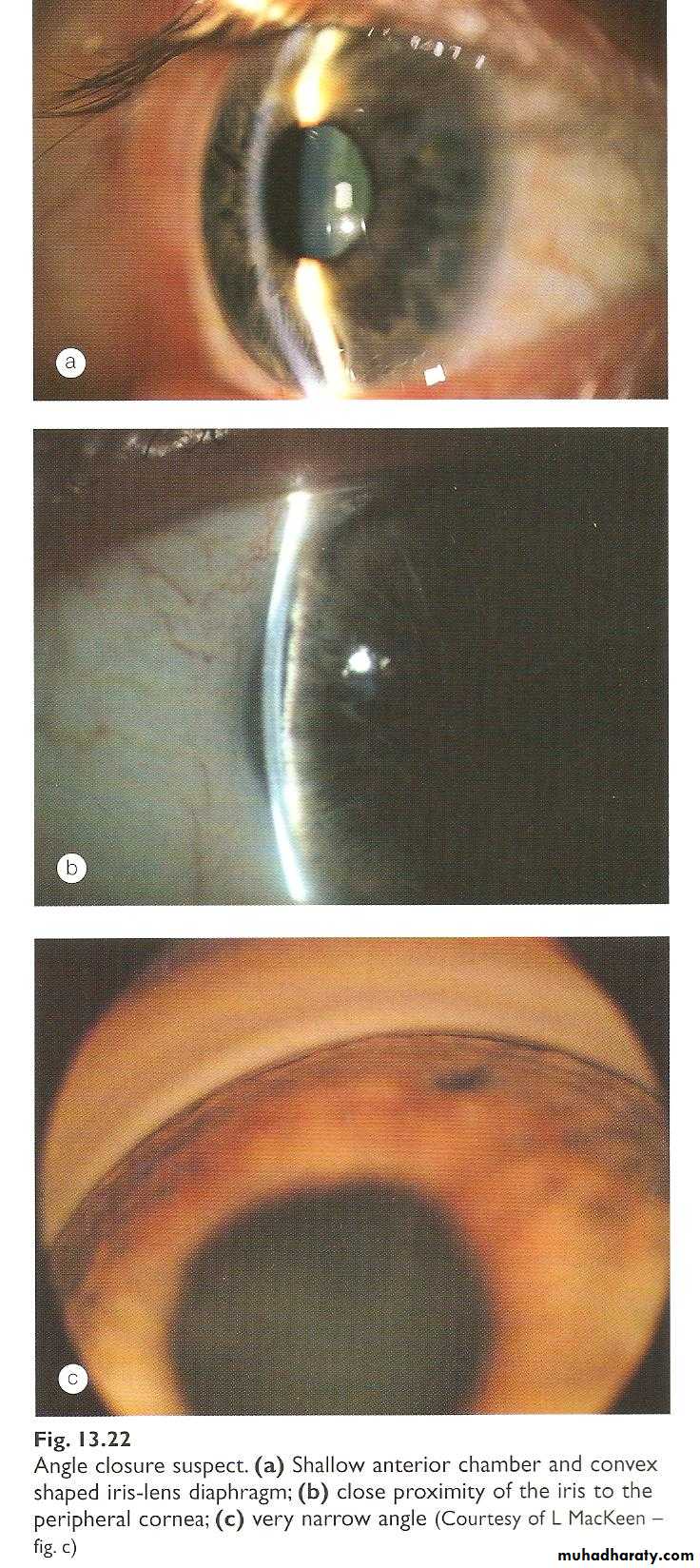
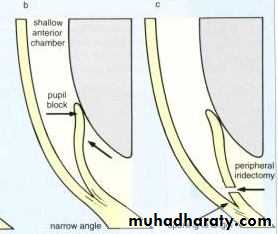
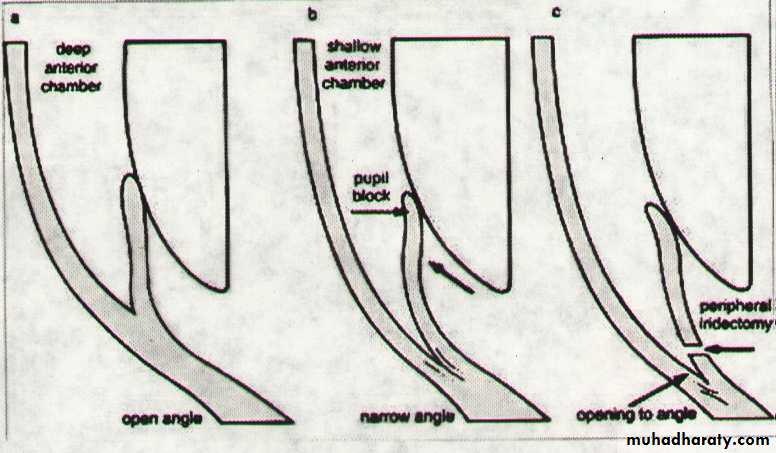
Is a condition in which elevation of IOP occurs as a result of obstruction of the aqueous drainage by closure of the angle with the peripheral iris.Anatomical predisposing factors
1- Relative anterior location of iris-lens diaphragm.2- Shallow anterior chamber (AC) due to short axial length of the eye ( e.g. hypermetropia).
3- Narrow entrance to anterior chamber angle.
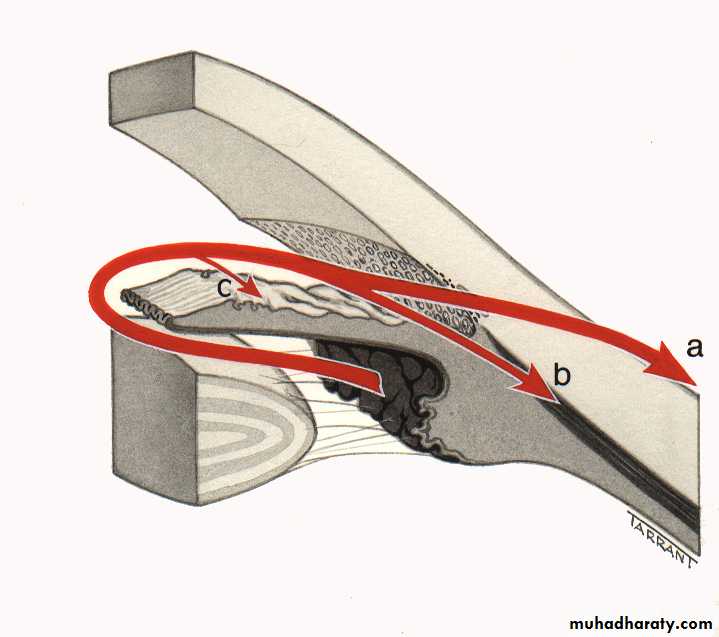
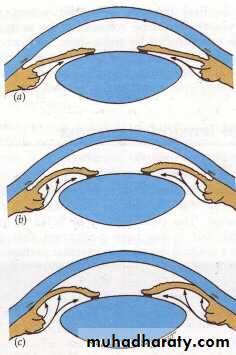
Mechanism of angle closure
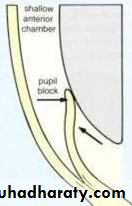
In most cases PCAG is initiated by;a- Pupillary Block : which is increase resistance to aqueous passage between posterior and anterior chamber by the iris lens contact .
b- Iris bombe : increase pressure in the posterior chamber, the peripheral iris will bow forward
c- Irido-corneal contact : obstructing the angle .
If this peripheral irido-corneal contact persist for few days then permanent peripheral anterior synachae (PAS) occurs
Presentation
Average age of is about 60 years and aboveMore common in females
Frequently bilateral, although presentation is asymmetrical
Classification
1. Latent2. Subacute
3. Acute
4. Chronic
5. Absolute
Subacute ( Intermittent) Angle Closure Glaucoma
A transient attack of sudden subtotal closure of the angle results in rapid increase in IOP, followed by spontaneous reopening of the angle with the IOP returns to normal.
Symptoms
The attack may be precipitated by physiological mydriasis (dilation of the pupil) e.g. watching T.V. in dark roomSudden onset of
1-Blurring of vision
2-Halloes around light due to corneal edema
3- Sometimes eye-ache or headache
The attack may last for 1-2 hours and usually broken by miosis (constriction of the pupil) e.g. exposure to bright light.
Signs
During the attackCorneal edema
Shallow anterior chamber
Elevated IOP
Between the attacks
The eye looks normal apart from narrow angle
Treatment
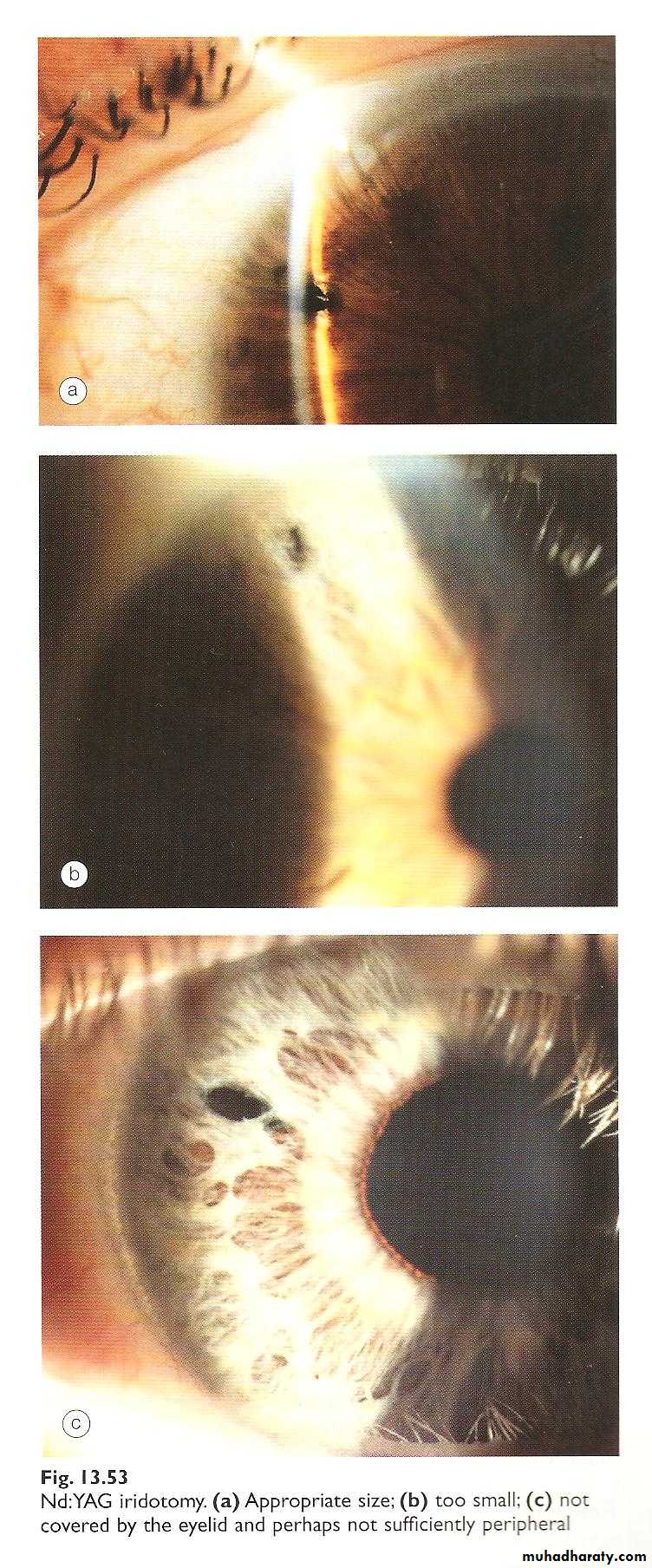
Laser iridotomy to create an opening between the posterior chamber and anterior chamber and bypass the pupillary blockBoth eyes must be treated with Laser iridotomies
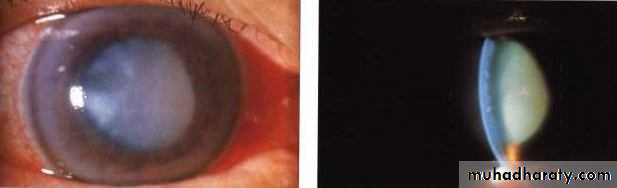
Acute Angle Closure Glaucoma
Sudden total closure of the angle with rapid high increase in IOP.Symptoms
Onset : SuddenPeriocular pain and headache
Bluring of vision
Halloes around light due to corneal edema
Redness of the eye
Sometimes nausea and vomiting
Signs
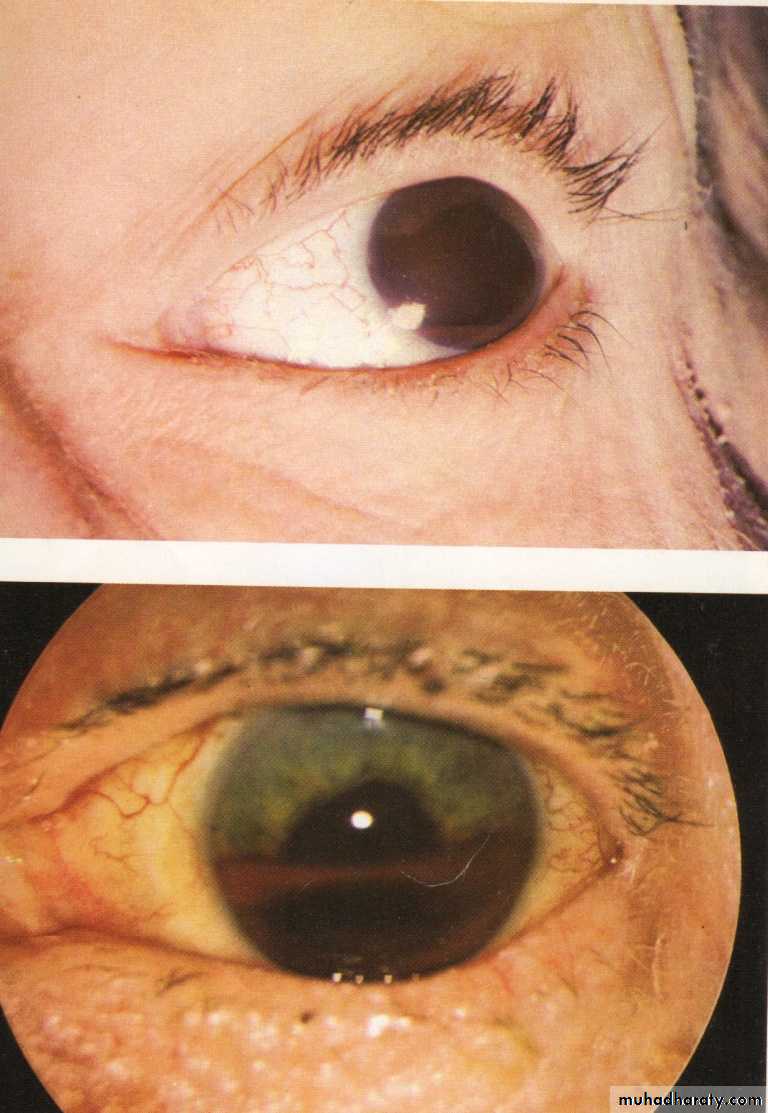
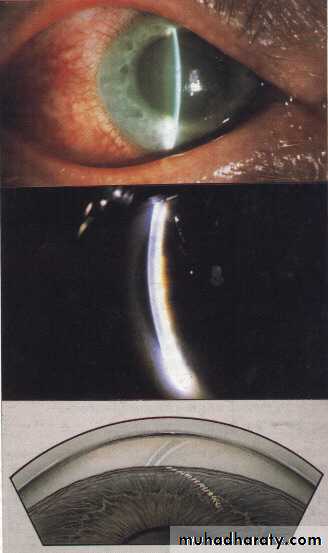
Cicum-corneal congestion
Corneal edema
Shallow anterior chamber
Mid-dilated ,fixed pupil
IOP elevated
Clinical features
Treatment
Admission to the hospitalMedical treatment :
Systemic Carbonic anhydrase inhibitors, initially Acetazolamide 500mg i.v. followed by 250 mg orally qds.
Topical 2% pilocarpine qds.
Topical 0.5% timolol bds.
If IOP still high after one hour then hyper osmotic agent is given
20% mannitol 1-2 gm/kg i.v. over 45 minutes
After reducing IOP medically treatment is essentially by laser iridotomy in early cases without established PAS (to create an opening between the posterior chamber and anterior chamber and by pass the pupillary block).
While in late cases with PAS, treatment is with surgical trabeculotomy to create an opening between the anterior chamber and sub-conjunctival space and by pass the PAS.
The other eye must be prophylactically treated with laser iridotomy.
If urgent management is not given, there will irreversible damage to the optic nerve with permanent blindness
Secondary Closed Angle Glaucoma
1- Lens-related glaucoma2- Neovascular glaucoma
3- Inflammatory glaucoma
4- Intra ocular tumor may push iris lens diaphragm forward and closing the angle
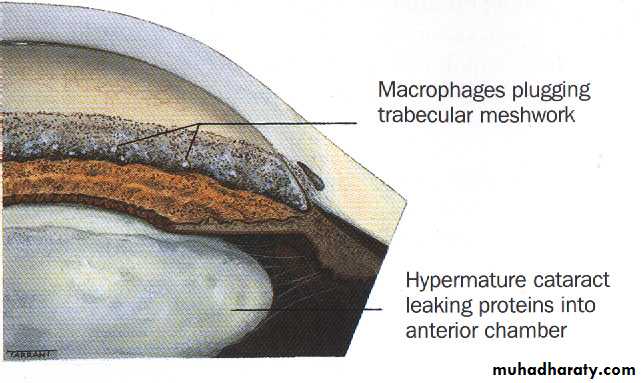
1-Lens-related glaucoma:
a- Phacolytic glaucoma.b- Phacomorphic (Intumescent) glaucoma:
b- Phaco anaphylactic glaucoma:a- Phacolytic glaucoma
b- Phacomorphic (Intumescent) glaucoma
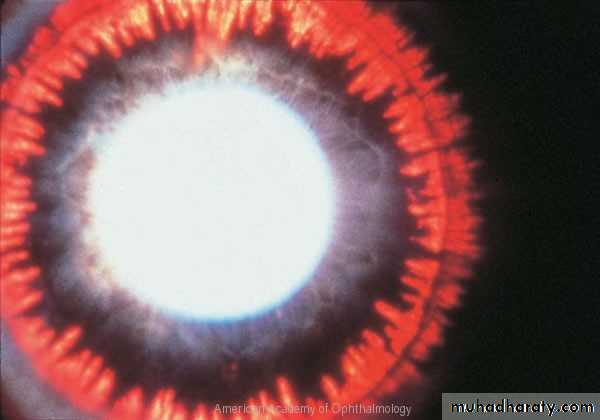
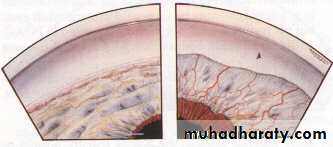
2- Neovascular glaucoma
Caused by rubeosis iridis associated with chronic, diffuse retinal ischaemia .Causes
• Central retinal vein occlusion. (commonest cause)• Diabetes mellitus (proliferative diabetic retinopathy).
• Miscellaneous
• Carotid obstructive disease.
• Central retinal artery occlusion.
• Intraocular tumours.
• Long standing retinal detachment.
• Chronic intraocular inflammation.
Inflammatory glaucoma
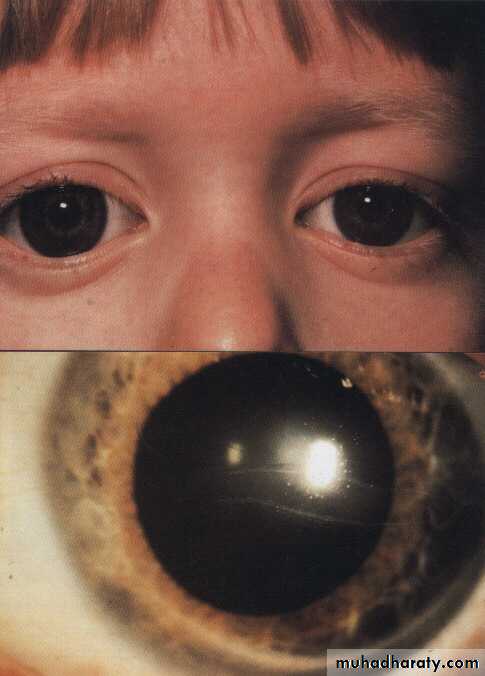
Congenital Glaucoma
Affect 1:10,000 birthsTrue congenital glaucoma: represents (40%) of all congenital glaucoma
2- Infantile glaucoma: represents (55%) of congenital glaucomas,
Juvenile glaucoma: represents (5%) of congenital glaucomas,
75% bilateral
65% male
Clinical features
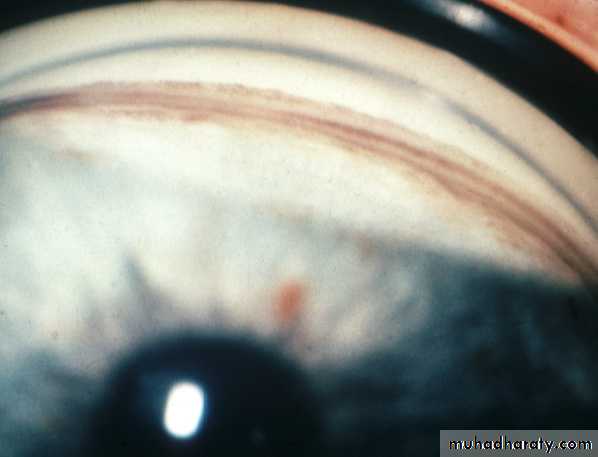
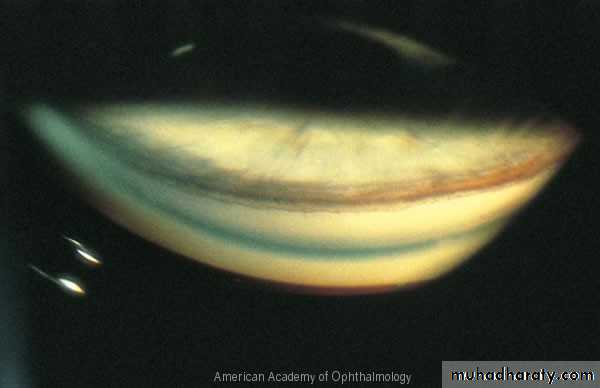
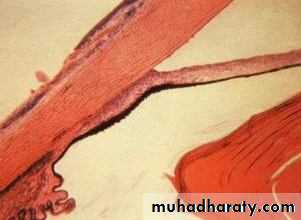
Corneal haze.Buphthalmos.
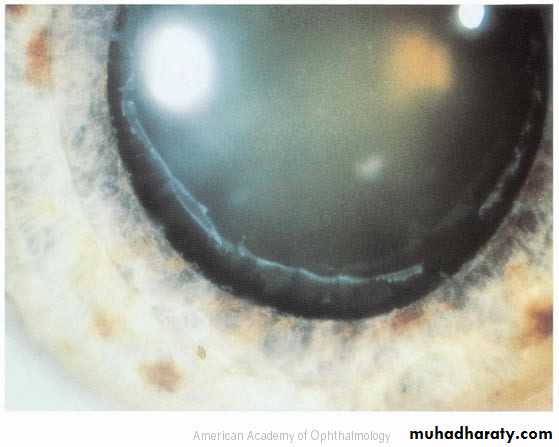
Breaks in descement membrane. (Haab striae)
Optic cupping
Diagnosis
Corneal diameterIOP
C/D ratio