Renal Physiology
Proff. Amjad Fawzi
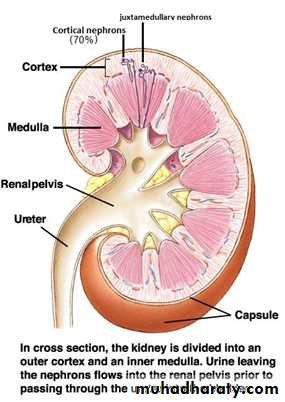
2016anatomy
Renal functions
[1] Regulate water and electrolytes balance:
Intake of water and many electrolytes usually are governed mainly by a persons's eating and drinking habits, necessating the kidneys to adjust their excretion rates to prevent excess OR loss state.
[2] Responsible for excretion of metabolic waste products
urea (from the metabolism of amino acids)
creatinine (from muscle creatine)
metabolites of drugs and toxins.
Wastes must be eliminated as rapidly as they are produced to prevent the toxic effects of their accumulation.
[3] Play essential role in regulation of arterial pressure
long-term regulation (through excretion of variable amounts of sodium and water)short-term regulation (through secretion of vasoactive substances such as renin).
[4] Contribute to acid-base regulation through
excreting acids
regulating the body buffer stores.
[5] Regulation of erythrocyte production from the bone marrow by secreting erythropoetin.
[6] Regulate vit D production .
The processes of urine formation
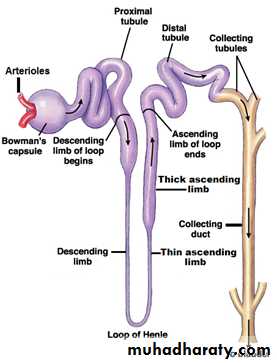
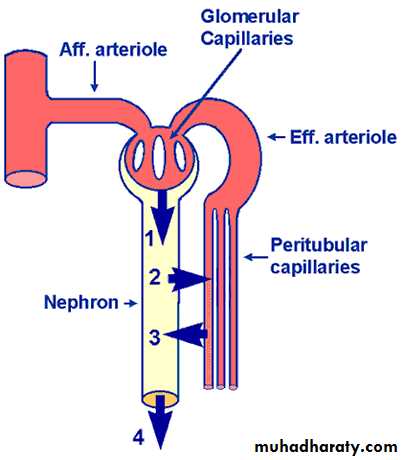
• Glomerular filtration (F)• Tubular reabsorption (R)
• Tubular secretion (S)
• Urinary exretion of substance = F-R+S
• Net reabsorption
• Net secretion
•
Filtration
non selective process…..In order to restore body fluids volume & composition …..we need
Reabsorption
highly selective according to body need
complete R: glucose & AA
partial R: water & electrolytes
no R : wastes (urea,creat,UA)
For fine tuning of body fluid volume & comp qualitatively we need…..
Secretion
H ion secretion to keep blood Ph
K ion secretion
Filtration must be constant to prevent gain or Loss (to keep homeostasis)…..the problem is
Filtration is pressure dependent and pressure is variable …??....how to solve this problem?
The answer is AUTOREGULATION
myogenic……afferent arteriole reflexive constr&dilation.
JG apparatus
Glomerular filtration rate (GFR)
The amount of fluid filtred through the glomerulus each minute in both kidneys. GFR =125 ml/min (180 L/day).
• glomerular capillaries has very high permeability
• 100-500 times as great as that of the usual capillary.
• glomerular capillaries has high degree of selectivity depends on:
• Size of the molecules
• less than 4 nm are freely filtrated
• more than 8 nm filtration is zero
2. The electrical charges of the molecules
The inner side of the pores of the glomerular membrane is negatively chargedFor these two reasons(size &charge)
the glomerular membrane is almost completely impermeable to all plasma proteins
The composition of the glomerular filtrate is the same as plasma except that it has no significant amount of proteins.
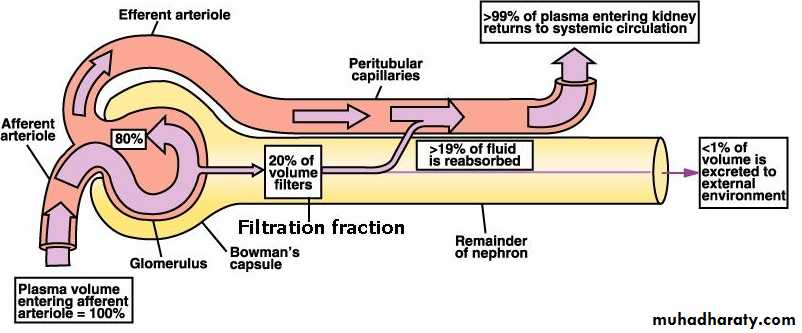
Filtration fraction
The fraction of the renal plasma flow that becomes glomerular filtrate.Since the normal plasma flow through both kidneys is 650 ml/min and the normal GFR is 125 ml/min, the average filtration fraction is about 20%.
Measurement of GFR
Clearance: Is the volume of blood cleared of a substance per unit time.• GFR can be measured by calculating the clearance of a substance which fulfills the following criteria
• Freely filtered.
• Neither reabsorbed nor secreted by the tubules.
• Not metabolized or stored in the kidney.
• Not toxic and not affecting the GFR.
• A substance known as inulin fulfill the above criteria, therefore it can be used to measure GFR.
• Inulin clearance = UV/P
• U= urine conc of inulin• V= urine volume
• P= plasma conc of inulin
• = 1.1 x 29/ 0.25 = 128 mL/min=GFR.
however, measurement of endogenous creatinine clearance is more suitable because it does not need intravenous infusion as in inulin.
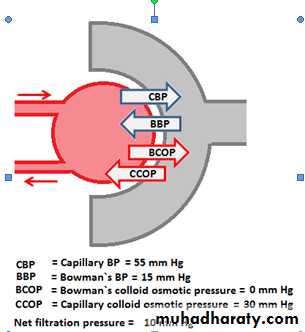
Filtration pressure The net pressure forcing fluid through glomerular membrane. it is determined by:
[A] Glomerular capillary hydrostatic pressure
[B] Bowman's capsule hydrostatic pressure
[C] Glomerular capillary colloid osmotic pressure
[D] Bowman's capsule colloid osmotic pressure
Factors that affect GFR
[A] Glomerular capillary hydrostatic pressure: affected by:1.Renal blood flow
2. Afferent arteriolar constriction
decrease the glomerular pressure and decrease the GFR, and vice versa.
3. Efferent arteriolar constriction
A slight efferent arteriolar constriction increases the glomerular pressure causing slight increase in GFR.
However, moderate and severe efferent arteriolar constriction causes a decrease in the GFR because large portion of plasma will filter out which increase the plasma colloid osmotic pressureز
[B] Bowman's capsule hydrostatic pressure
Urinary tract obstruction by stone for example, reduces GFR and vice versa.
[C] Glomerular capillary colloid osmotic pressure:
When decreased, GFR increases and vice versa.[D] Bowman's capsule colloid osmotic pressure:
damaged glomerular membrane by renal disease causes filtration of protiens and consequently increases GFR.
(II): The capillary filtration coefficient
The product of the permeability which (affected by renal diseases) and filtering surface area & thickness (affected by contraction or relaxation of mesangial cells).
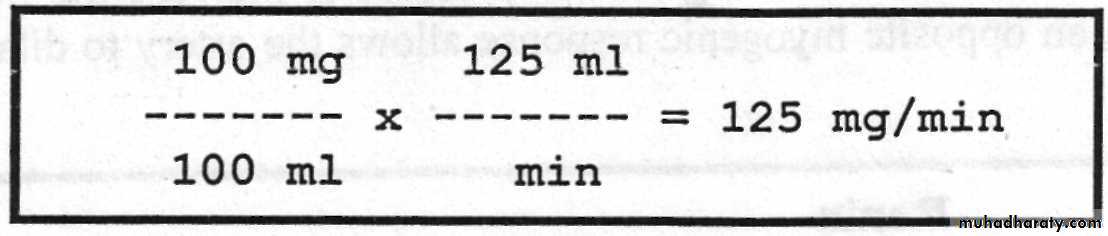
Is the total amount of the substance that filters through the glomerular membrane into tubules per minute.
Tubular load = conc. of the substance in the filtrate x GFR.
For example, if the plasma glucose is 100 mg/100 ml plasma and GFR =125 ml/min
so the tubular load of glucose is equal to :
Tubular load of a Substance
Tubular transport maximum (Tm) :It is the maximum rate for actively reabsorbing or secreting substance by the tubule.Tm for glucose = 320 mg/min
greater than 320 mg/min glucose begins to spill into the urine (Glycosuria).
Threshold concentration: It is the serum level of the substance below which none of it appears in the urine and above which progressively larger quantities appear.
The threshold concentration of glucose is 180 mg/100 ml
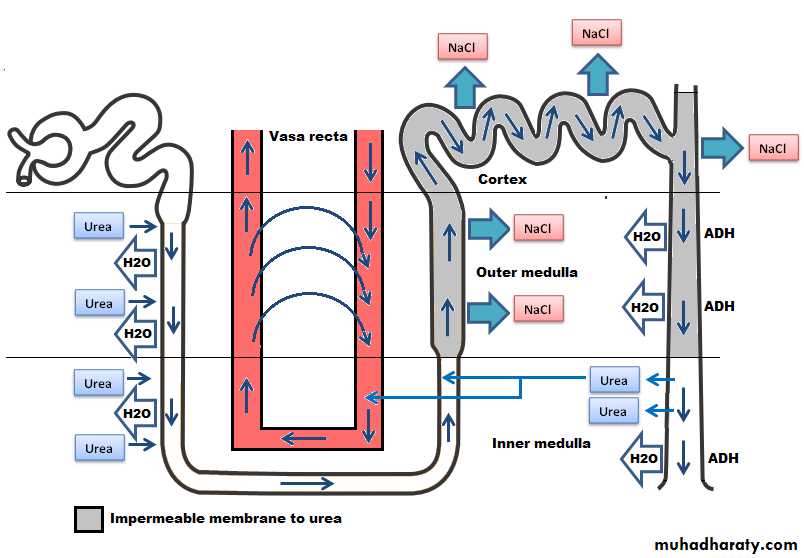
Role of urea
urea plays an important role in producing and maintaining the high medullary osmotic gradient necessary for the urine concentration process.people who fed a high protein diet concentrate their urine much better than those on low protein diet.
Urea excretion: The rate of urea excretion is determined by:
The concentration of urea in the plasma.The GFR.
Between 40-60% of the filtered urea is excreted with urine.
In many renal diseases there is reduction in the GFR and the following renal function tests results:
elevated blood urea
elevated creatinine
elevated uric acid.
Urea cycle: The kidneys can excrete urea with minimum quantities of water and this can be achieved by two mechanisms:
By the presence of ADH.
Recirculation of urea from the collecting duct into the thin limb of the loop of Henle so that it passes upward through distal tubule, collecting tubule and then collecting duct again.
In this way, urea can recirculate deep in the medulla for several times in a way to concentrate urea in the medullary interstitium before it is excreted.
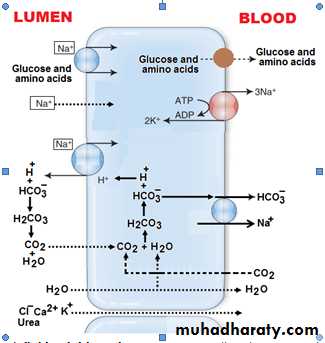
Hydrogen ion secretion in the proximal tubule
Regulation of Extracellular Fluid (ECF) Volume
The basic mechanism for fluid volume control is the same as the basic mechanism for arterial pressure control.• (1) Volume receptor reflexes
• A. Neural reflexes:
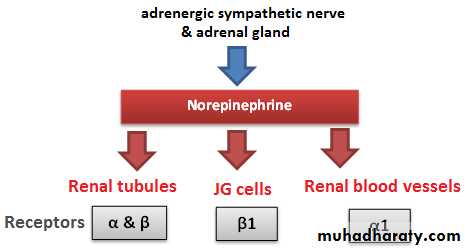
1. inhibits the renal sympathetic nerve increasing the urinary output(by increasing the …….?
2. Inhibiton of ADH secretion by the posterior pituitary gland allows the kidneys to excrete increased quantities of water.
B. Atrial Natriuretic Factor (ANF) release: Excess blood volume stretches the atrial walls and this promotes the release of ANF that in turn causes renal Na excretion and concomitant water loss .
• (2). Cardiac output mechanism: The final determination of the precise level to which the blood volume will be adjusted is still the function of the cardiac output level. This is because the volume receptors adapt completely within one to three days and become no longer active.
A slight increase in blood volume increases cardiac output markedly…increases arterial pressure markedly. …stim. baroreceptors…….activate essentially the same central nervous system reflexes as the atrial volume receptors.
Diuretics
A substance that increases the rate of urine output by decreasing Na reabsorption from the tubules, and this in turn causes loss of water (diuresis or polyuria).Because the renal tubular reabsorption of many solutes, such as K, Cl, Mg, and Ca, is also influenced secondarily by Na reabsorption, many diuretics raises renal loss of these solutes as well(side effects).
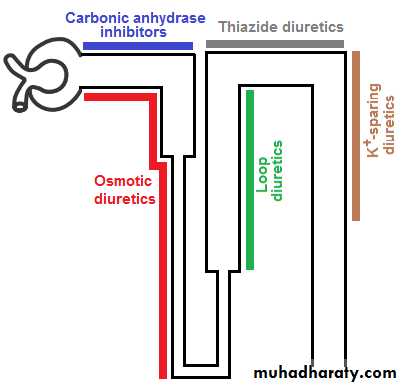
Types of diuretics
Osmotic diureticsglucose,sucrose,manitol
Inhibit water reabsorption mainly in the proximal tubules .
Loop diuretics
Frusemide(Lasix)
inhibit Na-K-Cl co-transport at thick ascending loop of Henle.
Thiazides
inhibit Na-Cl co-transport in luminal membrane at early distal tubule.
Sodium channel blockers
triamterene,amelorideluminal membrane of collecting tubules.
Aldosterone antagonist
Spironolactone
decrease Na reabsorption and decrease K secretion at collecting duct
they are called K sparing diuretics.
Carbonic anhydrase inhibitor
Acetazolamide
inhibit H secretion which reduce Na reabsorption at proximal tubule.
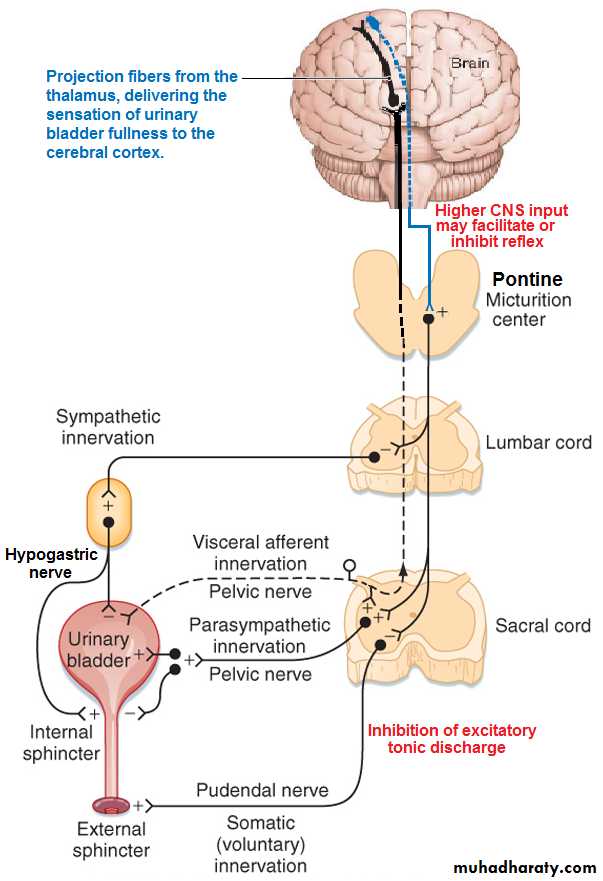
MICTURITION
Emptying the urinary bladder when it becomes filled.. The principal nerves supply to the bladder are:
(1). The pelvic nerves (S-2 and S-3)sensory ……detect s bladder wall stretch
parasympathetic motor supply of detrusor muscle to evacuate the bladder and inhibits the internal sphincter …….(micturition reflex).This is predominant in infants and children.
(2). Pudendal nerve
Motor somatic fibers innervate the skeletal muscle fibers of external bladder sphincter………(voluntary control).
(3).Hypogastric nerve (L2)
carry the sympathetic fiber mainly to the blood vessel and have very little to do with micturition.
mediate the contraction of the internal sphincter muscle that prevents semen from entering the bladder during ejaculation.
The Micturition Reflex
at 150 ml ……first urge to void is felt ….at 300-400 ml….. marked sense of fullness.
When convenient, micturition reflex started, otherwise, higher control centers in the pons send inhibitory signals to prevent micturition)in adults).
See animation below for more information on the micturition reflex.
animation of micturution reflex
Abnormalities of Micturition[1] Atonic bladder
Destruction of the sensory fibers
prevents micturition reflex contraction
the bladder fills to capacity and overflows a few drops at a time through urethra (overflow dribbling or incontinence).
[2] The autotmtic bladder
spinal cord is damaged above the sacral region
micturition reflexes can still occur however, they are no longer controlled by the brain.
[3] The neurogenic bladder
partial damage in the spinal cord or the brain stem that interrupts most of the inhibitory signals
facilitatory impulses passing continually down the cord keep the sacral centers so excitable causing fequent uncontrolled micturation.