1
Fifth stage
Dermatology
Lec-20
.د
عمر
18/4/2016
Actinic Keratosis & Squamous Cell Carcinoma
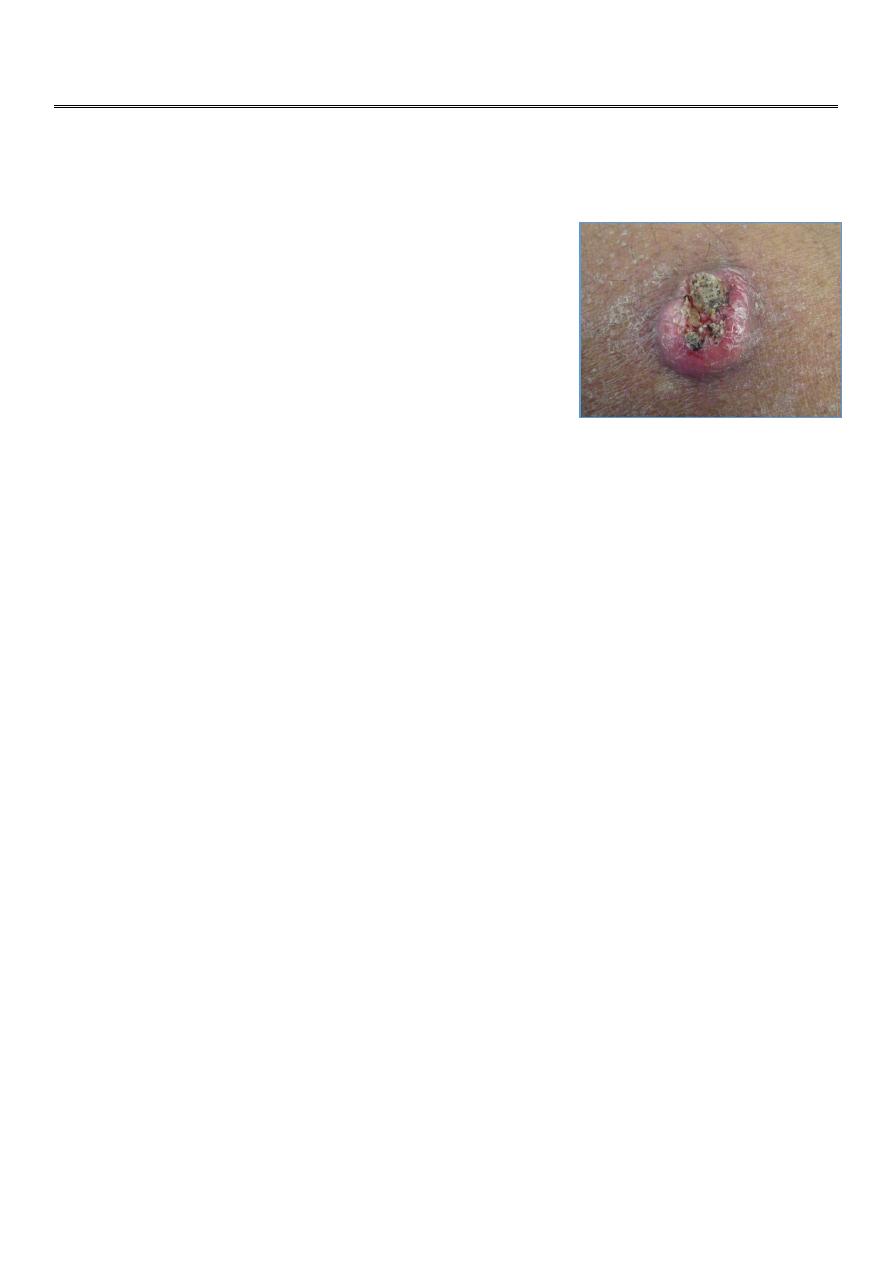
Case One: Skin Exam:
How would you describe this growth?
Well-circumscribed, 2cm, erythematous nodule with
central ulceration and crust. The lesion is firm with
palpation.
What is your differential diagnosis?
Actinic keratosis
Basal cell carcinoma
Melanoma
Seborrheic keratosis
Squamous cell carcinoma
Verruca vulgaris
Management:
What is your next step in management?
1. Liquid nitrogen cryotherapy
2. Reassurance with close follow-up
3. Shave biopsy
4. Surgical excision
5. Topical antibiotics
Answer: c
What is your next step in management?
a. Liquid nitrogen cryotherapy (Would not treat the lesion with cryotherapy
without knowing the diagnosis. This is a suspicious lesion that warrants a
biopsy)
b. Reassurance with close follow-up (A history of a new growing lesion with
concerning characteristics warrants a biopsy)
2
c. Shave biopsy (Before treating this lesion, you must establish a diagnosis)
d. Surgical excision (You must know the diagnosis before you can plan treatment
with surgical excision and surgical margins)
e. Topical antibiotics (The lesion is not an infection)
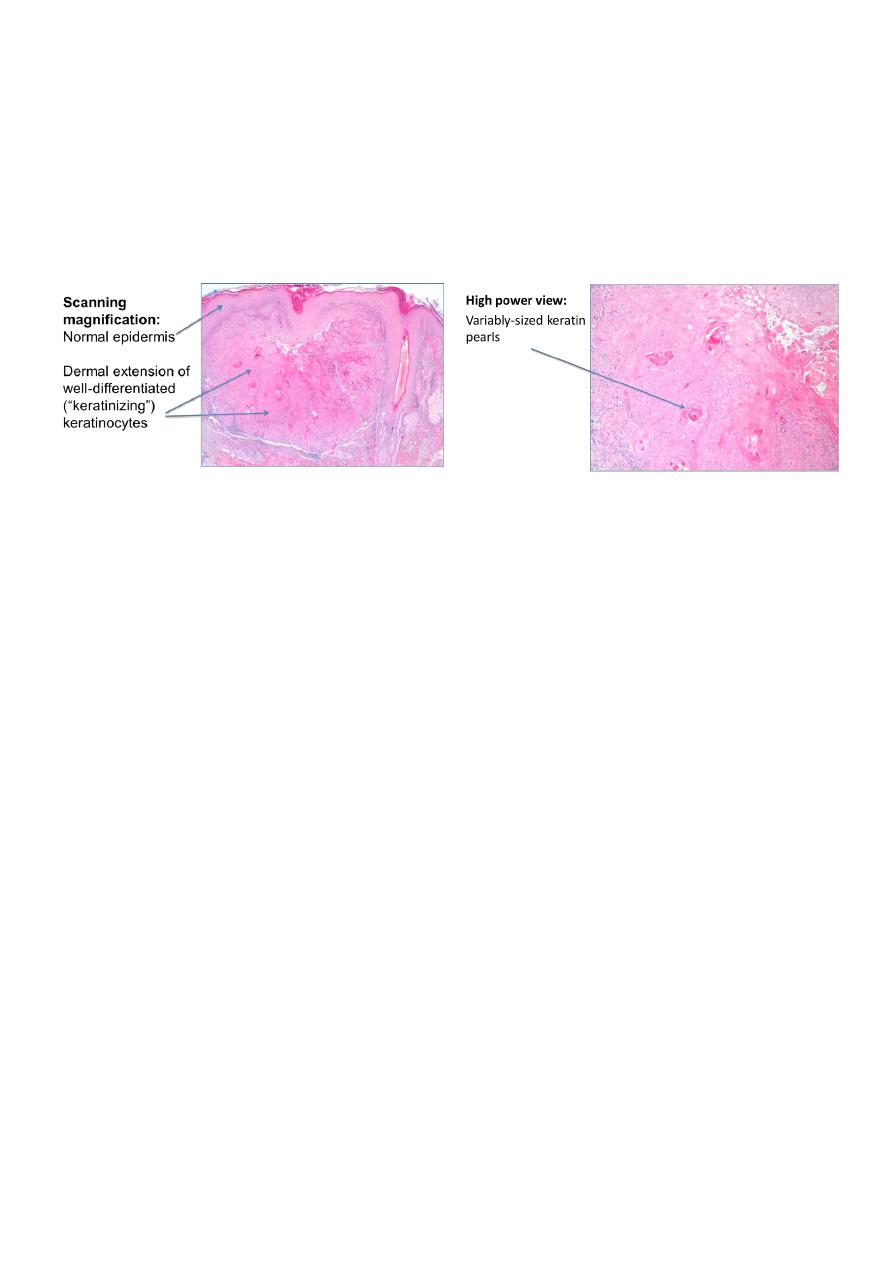
Shave biopsy reveals…
Diagnosis:
What is your diagnosis? Click on the correct answer.
Actinic keratosis
Basal cell carcinoma
Melanoma
Verruca vulgaris
Seborrheic keratosis
Squamous cell carcinoma
What is your diagnosis?
That was incorrect. Try again.
Actinic keratosis
Basal cell carcinoma
Melanoma
Verruca vulgaris
Seborrheic keratosis
Squamous cell carcinoma
Your diagnosis is correct!
Actinic keratosis

3
Basal cell carcinoma
Melanoma
Verruca vulgaris
Seborrheic keratosis
Squamous cell carcinoma
Squamous cell carcinoma (SCC)
Most commonly occurs among people with white/fair skin
Commonly located on the head, neck, forearms, and dorsal hands (sun-exposed
areas)
SCC has increased associated mortality compared to basal cell carcinoma, mostly due
to a higher rate of metastasis
SCC: Etiology
Cell of origin: keratinocyte
Cumulative UV exposure
• Cause genetic alterations, which accumulate and provide selective growth
advantage
SCC arising in non sun-exposed areas may be related to chemical carcinogen
exposure (e.g. arsenic)
SCC: Clinical manifestations
Various morphologies
• Papule, plaque, or nodule
• Pink, red, or skin-colored
• Scale
• Exophytic (grows outward)
• Indurated (dermal thickening, lesion feels thick, firm)
• May present as a cutaneous horn
Friable – may bleed with minimal trauma and then crust
Usually asymptomatic; may be pruritic

4
SCC in situ
Also known as Bowen’s disease
Circumscribed pink-to-red patch or thin plaque with scaly or rough surface
Keratinocyte atypia is confined to the epidermis and does not invade past the
dermal-epidermal junction
Back to our case
Our patient was diagnosed with invasive SCC. What is your next step in management?
a. Liquid nitrogen cryotherapy
b. Reassurance with close follow-up
c. Shave biopsy
d. Surgical removal
e. Topical antibiotics
What is your next step in management?
Answer: d
a. Liquid nitrogen cryotherapy (Liquid nitrogen is used to treat pre- cancerous actinic
keratoses. It is NOT the treatment for invasive squamous cell carcinoma.)
b. Reassurance with close follow-up (Squamous cell carcinoma is a malignant lesion with
potential for metastases. You must treat it!)
c. Shave biopsy (You already know the diagnosis and there is no need for another
biopsy.)
d. Surgical removal (The treatment of choice for squamous cell carcinoma is surgical
excision. The specimen must be sent to pathology to document clear margins
(complete excision).)
e. Topical antibiotics (The lesion is not an infection.)
Pathology reports for SCC:
“Invasive squamous cell carcinoma”
• Means there are SCC cells in the dermis
• If there is no dermal involvement, it is squamous cell carcinoma in situ

5
• Unrelated to metastatic potential
“Atypical squamous proliferation”
• Often used when biopsy is too superficial
• If dermis cannot be seen in the biopsy, invasive SCC cannot be excluded
SCC: Treatment
There are several medical and surgical treatment options
Suspicion of SCC should prompt referral to a dermatologist for evaluation and
discussion of specific treatment approaches
Surgical Treatment Options
• Surgical excision (standard of care for invasive SCCs)
Wide local excision
Mohs micrographic surgery
• Curette and Desiccation (reserved for in situ SCC)
Non-surgical Treatment Options
• Radiation therapy for poor surgical candidates
• 5-Fluorouracil cream, imiquimod cream, photodynamic therapy – typically
reserved for in situ SCCs when excision is a suboptimal choice
SCC: Course & Prognosis
For SCC arising in sun-exposed skin, the rate of metastasis to regional lymph nodes ~
5%
Higher rates of metastasis if:
• Large (diameter > 2cm), deep (> 4mm), and recurrent tumors
• Tumor involvement of bone, muscle, and nerve
• Location on scalp, ears, nose, and lips
• Tumor arising in scars, chronic ulcers, burns, sinus tracts, or on the genitalia
• Immunosuppressed patients
• Tumors caused by arsenic ingestion
6
Patient Follow-up:
All patients treated for cutaneous SCC need surveillance for the early recognition and
management of:
• Treatment-related complications
• Local or regional recurrences
• Development of new skin cancers
Patients with a history of SCC should have close follow-up
Patients are often seen every 6 to 12 months
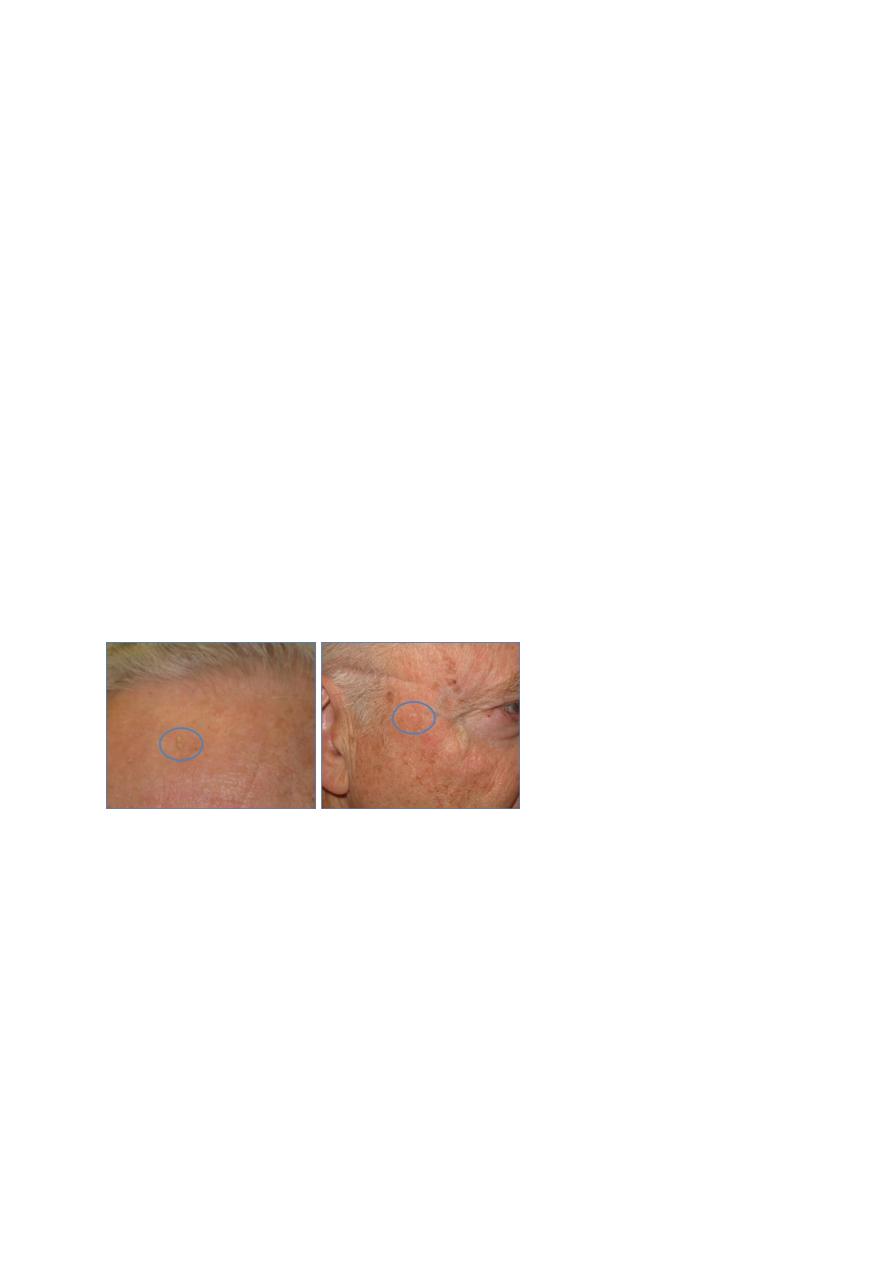
Case Two
Case Two: History
A 66-year-old man with a history of SCC who presents to the dermatology clinic for
his regularly scheduled follow-up visit. He reports that during a self skin exam, he
noticed a few rough, red spots on the face. He asks if this could represent another
cancer.
How would you describe the skin findings?
Rough, scaly, thin, red-pink plaques scattered on the forehead and right temple area
Diagnosis:
What is your diagnosis? Click on the correct answer.
Actinic keratosis
Basal cell carcinoma
Melanoma
Seborrheic keratosis
Squamous cell carcinoma
Verruca vulgaris
7
Your diagnosis is correct!
Actinic keratosis
Basal cell carcinoma
Melanoma
Seborrheic keratosis
Squamous cell carcinoma
Verruca vulgaris
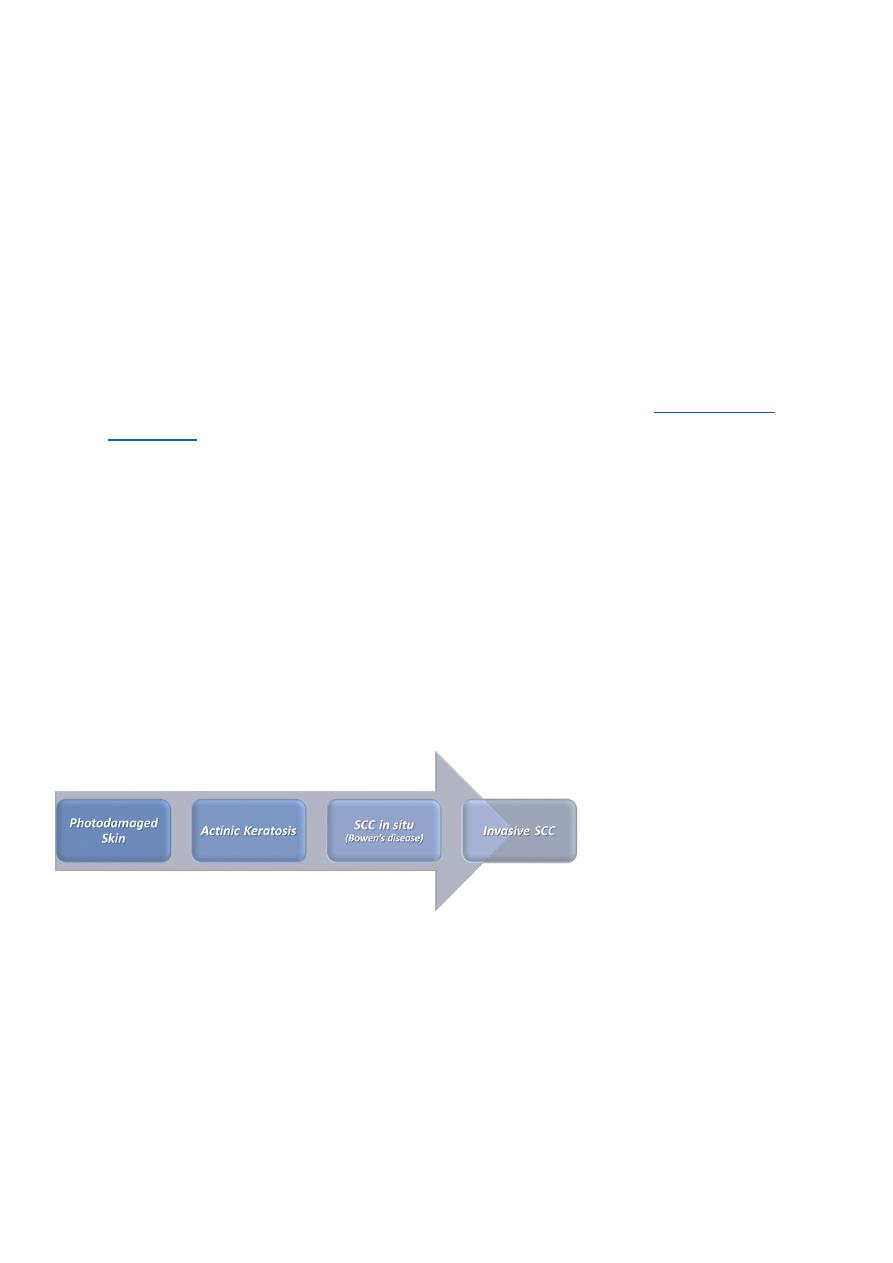
Actinic Keratosis (AK)
AKs are premalignant lesions; they have the potential of transforming into a skin
cancer. Virtually all AKs that transform into cancer will become
Most AKs do not progress to invasive SCC
• Risk of malignant transformation of an AK to SCC within one year is about 1 in
1000
• Risk factors for malignant progression of AK to SCC include: persistence of the
AK, history of skin cancer, and immunosuppression
The keratinocyte is the cell of origin
AKs may be considered as part of a disease spectrum:
AK: Etiology
Cumulative and prolonged UV exposure, resulting in:
• UV-induced p53 tumor suppressor gene mutations
Individual risk factors can increase susceptibility:
• Increasing age
• Fair skin, light eyes/hair (skin types I,II)

8
• Immunosuppression
• Genetic syndromes, such as xeroderma pigmentosum and albinism
AK: Clinical manifestations
May be symptomatic (tender)
Located in sun-exposed areas
• Head, neck, extensor forearms, and dorsal hands
Typically on background of sun damaged skin
Erythematous papule or thin plaque with a characteristic rough, gritty scale
Often diagnosed by feel (like sandpaper)
* The diagnosis of AKs should be made cautiously in lesions > 6mm since these may
represent SCC in situ or a superficial BCC.
AK: Actinic cheilitis
Actinic cheilitis represents AKs on the lips, most often the lower lip
Erythematous patch with rough gritty scale involving the lower lip
Persistent ulcerations or indurated areas should prompt a biopsy to rule out malignant
transformation
AK: Treatment
There are several topical and procedural treatment options for AKs. The best option
is chosen after consideration of number, location, and thickness, among other
patient factors.
Therapies are considered local – treating the individual lesion, or field therapies –
treating multiple AKs in one area
Consultation with a dermatologist to guide therapy may be useful
Localized Therapies
Liquid nitrogen cryotherapy
Curettage +/- electrocautery
Shave excision

9
Field Therapies
Topical 5-fluorouracil or imiquimod creams
Photodynamic therapy
AK: Patient Education
Patients with AKs are at increased risk of developing other non-melanoma and
melanoma skin cancers.
• Therefore, these patients should have regular skin exams every 6-12 months
• Patients should be seen prior to their regularly scheduled follow-up if they
notice a concerning lesion on a self-skin exam
Patient Education: Be Sun Smart
®
Generously apply a broad-spectrum, water-resistant sunscreen with a Sun
Protection Factor (SPF) of 30 or more to all exposed skin.
• “Broad-spectrum” provides protection from both UVA and UVB rays.
• Reapply approximately every two hours, even on cloudy days, and after
swimming or sweating.
Wear protective clothing, such as a long-sleeved shirt, pants, a wide-brimmed hat,
and sunglasses.
Seek shade.
• Remember that the sun's rays are strongest between 10 AM – 4PM.
• If your shadow appears to be shorter than you are, seek shade.
Use extra caution near water, snow, and sand because they reflect and intensify the
damaging rays of the sun, which can increase your chances of a sunburn.
Get vitamin D safely through a healthy diet that may include vitamin supplements.
Don't seek the sun.
Avoid tanning beds. Ultraviolet light from the sun and tanning beds can cause skin
cancer and wrinkling. If you want to look tan, consider using a self-tanning product,
but continue to use sunscreen with it.
Check your birthday suit on your birthday. If you notice anything changing, growing,
or bleeding on your skin, see a dermatologist.

10
How to perform a skin self-examination
Take Home Points:
Indurated erythematous lesions with keratin are SCC until proven otherwise.
The diagnosis of SCC is established via shave biopsy.
The treatment of SCC is surgical excision. Radiation therapy is a good choice in poor
surgical candidates.
Actinic keratoses are erythematous papules or thin plaques with scale. They feel
rough on palpation but are not indurated.
Actinic keratosis is a precancerous lesion that can evolve into squamous cell
carcinoma.
The treatment for actinic keratoses depends on the number of lesions and the
patient’s preference.
