Anatomy
For
Thorax
http://goo.gl/rjRf4F
I
LOKA
©
http://www.muhadharaty.com/anatomy-thorax
I

Content
Topics:
Page:
Thoracic wall
3
Mediastinum
21
The lung
29
The heart
44
Part1
: Thoracic wall
-
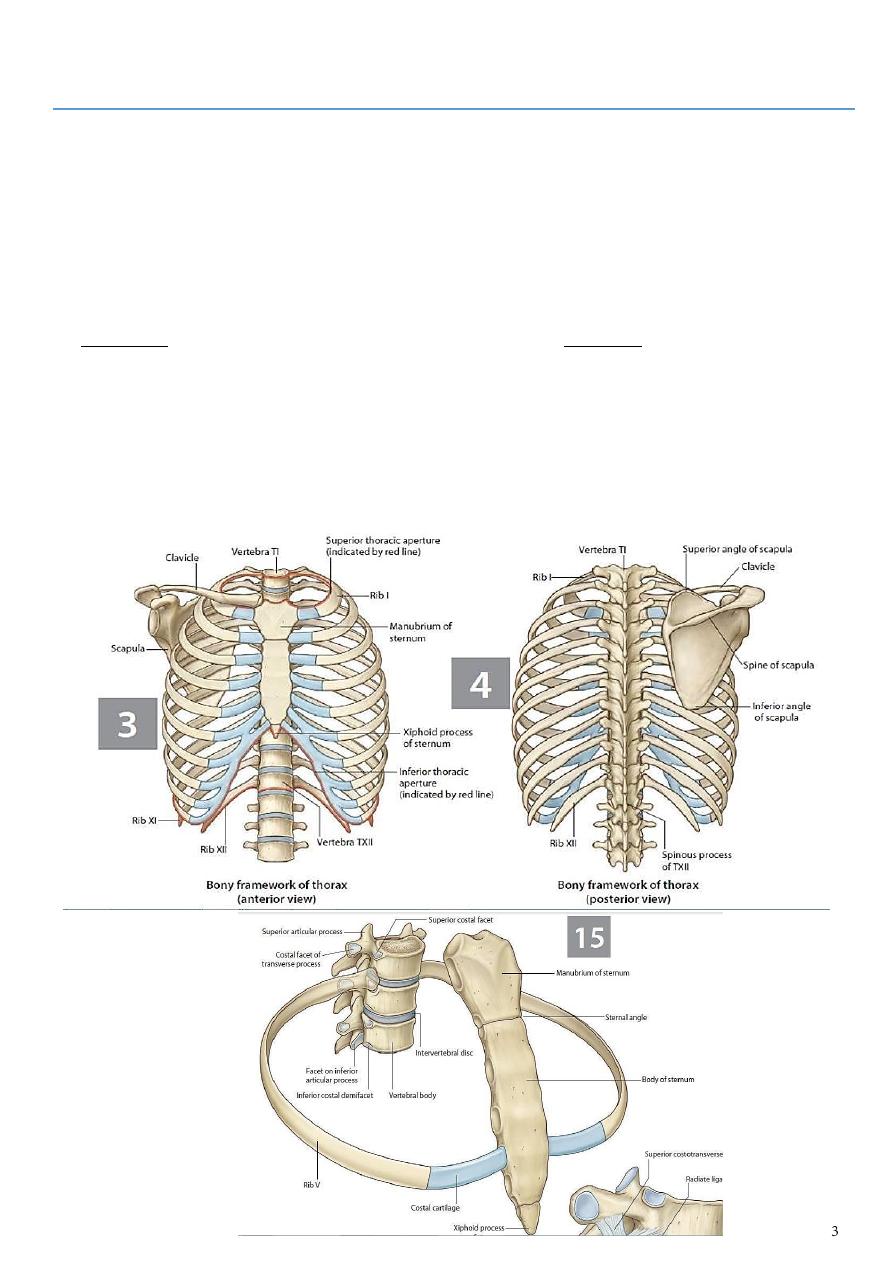
The thorax (or chest) : is the region of the body between the neck and the abdomen.
-
It is flattened in front and behind but rounded at the sides.
-
The framework of the walls of the thorax, which is referred to as the thoracic cage, is
formed by
1- the vertebral column behind
2- the ribs and intercostal spaces on either side
3- and the sternum and costal cartilages in front.
-
Superiorly, the thorax communicates with the neck, and inferiorly it is separated from
the abdomen by the diaphragm.
-
The thoracic cage protects the lungs and heart and affords attachment for the muscles
of the thorax, upper extremity, abdomen, and back.
-
The cavity of the thorax can be divided into : a median partition, called the mediastinum
and the laterally placed pleurae and lungs.
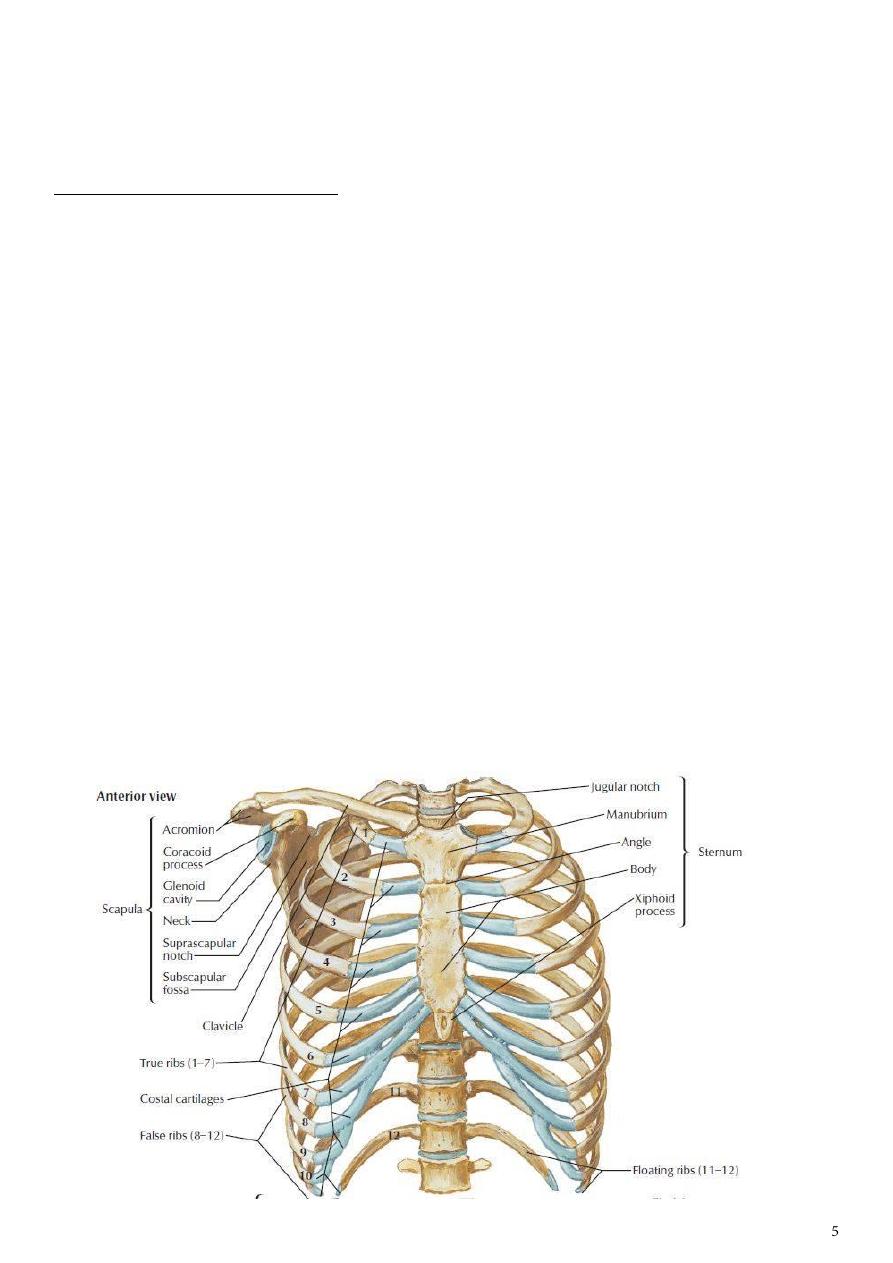
Structure of the Thoracic Wall
-
The thoracic wall is covered on the outside
by skin and by muscles attaching the
shoulder girdle to the trunk.
-
It is lined with parietal pleura.
-
The thoracic wall is formed
1- posteriorly by the vertebral column
2- anteriorly by the sternum and costal
cartilages
3- laterally by the ribs and intercostal spaces
4- superiorly by the suprapleural membrane
5- and inferiorly by the diaphragm, which
separates the thoracic cavity from the abdominal cavity.
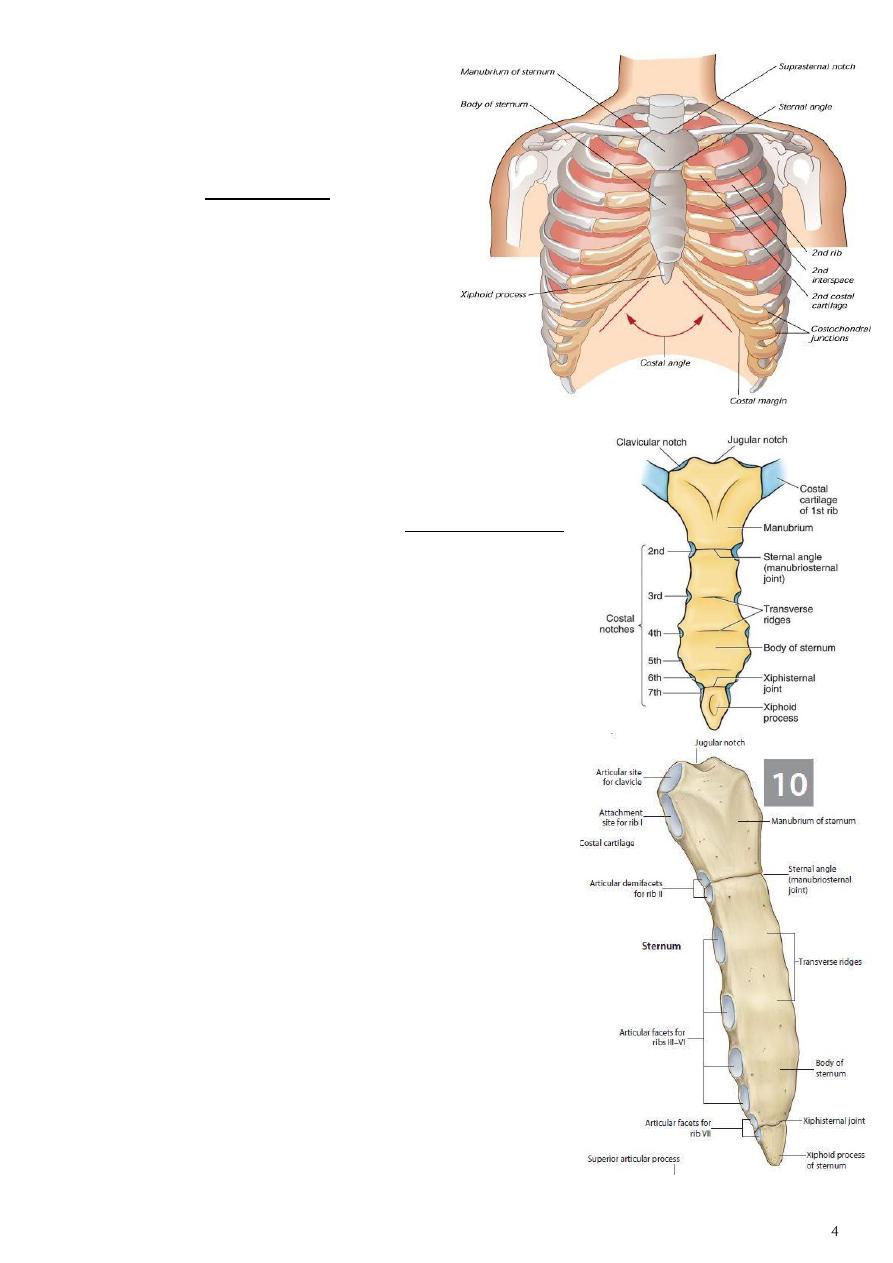
Sternum
-
The sternum lies in the midline of the anterior chest wall.
-
It is a flat bone that can be divided into three parts:
1.
Manubrium sterni.
2.
Body of the sternum.
3.
Xiphoid process.
1- The manubrium
▪ is the upper part of the sternum.
▪ It articulates with
a-
the body of the sternum at the manubriosternal
joint
b-
it also articulates with the clavicles
c-
and with the1st costal cartilage
d-
and the upper part of the 2nd costal cartilages on
each side.
▪ It lies opposite the 3
rd
and 4th thoracic vertebrae.
2- The body of the sternum
▪ Articulates :
1-
above with the manubrium at the manubriosternal
joint
2-
below with the xiphoid process at the xiphisternal
joint.
3-
On each side, it articulates with the 2nd to the 7th
costal cartilages
3- The xiphoid process
▪ is a thin plate of cartilage that becomes ossified at its proximal end during adult life.
▪ No ribs or costal cartilages are attached to it.
The sternal angle (angle of Louis)
-
formed by the articulation of the manubrium with the body of the sternum
-
can be recognized by the presence of a transverse ridge on the anterior aspect of the
sternum.
-
The transverse ridge lies at the level of the 2nd costal cartilage, the point from which
all costal cartilages and ribs are counted.
-
The sternal angle lies opposite the intervertebral disc between the 4th and 5th
thoracic vertebrae.
-
The xiphisternal joint lies opposite the body of the ninth thoracic vertebra.
Ribs
There are 12 pairs of ribs, all of which are attached posteriorly to the thoracic vertebrae.
The ribs are divided into three categories:
1.
True ribs: The upper seven pairs are attached anteriorly to the sternum by their
costal cartilages.
2.
False ribs: The 8th, 9th, and 10th pairs of ribs are attached anteriorly to each other
and to the 7th rib by means of their costal cartilages and small synovial joints.
3.
Floating ribs: The 11th and 12th pairs have no anterior attachment.
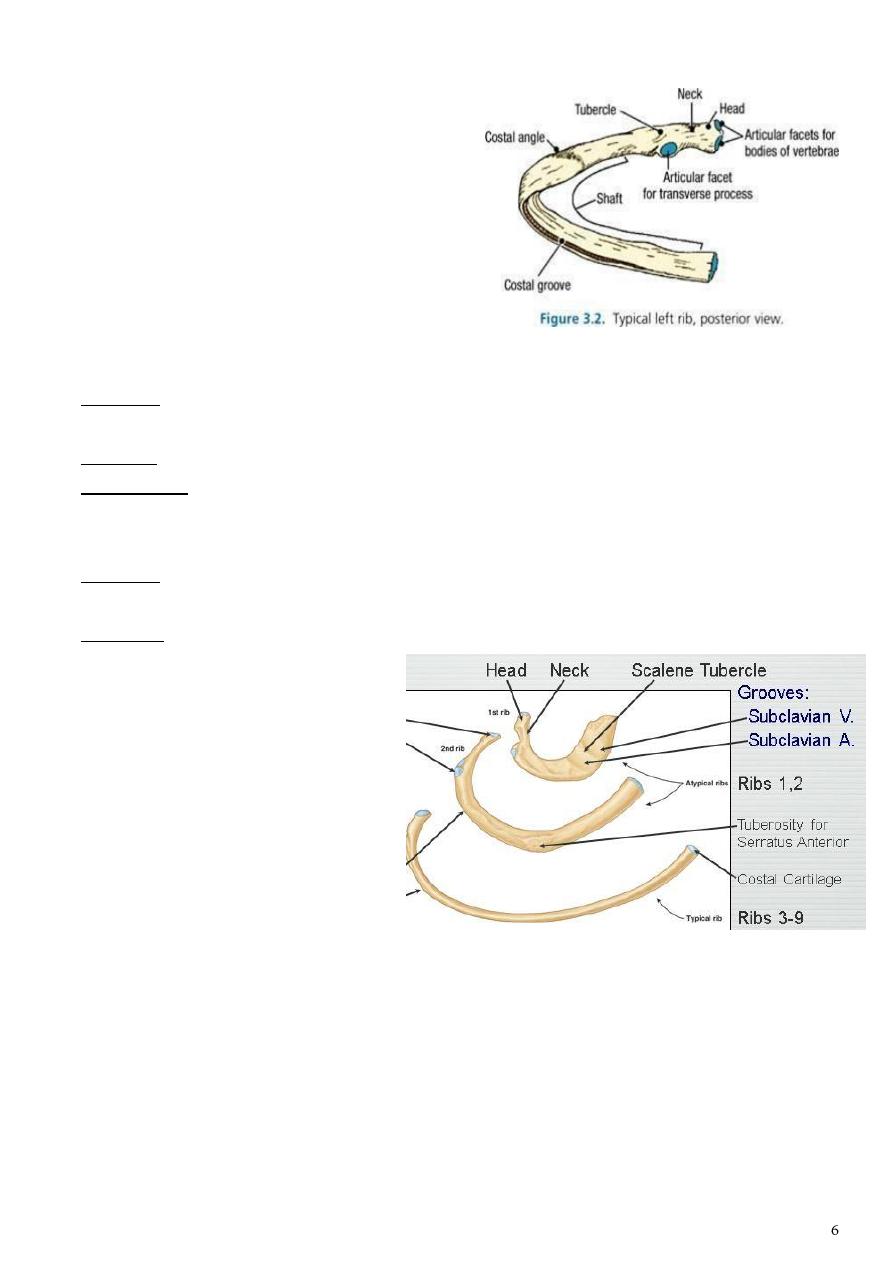
Typical Rib
A typical rib is :
1- a long, twisted, flat bone having a rounded,
smooth superior border and a sharp, thin
inferior border.
2- The inferior border overhangs and forms the
costal groove, which accommodates the
intercostal vessels and nerve.
3- The anterior end of each rib is attached to
the corresponding costal cartilage.
A rib has a head, neck, tubercle, shaft, and angle.
The head has two facets for articulation with the numerically corresponding vertebral
body and that of the vertebra immediately above.
The neck is a constricted portion situated between the head and the tubercle.
The tubercle is a prominence on the outer surface of the rib at the junction of the neck
with the shaft. It has a facet for articulation with the transverse process of the
numerically corresponding vertebra.
The shaft is thin and flattened and twisted on its long axis. Its inferior border has the
costal groove.
The angle is where the shaft of the rib bends sharply forward.
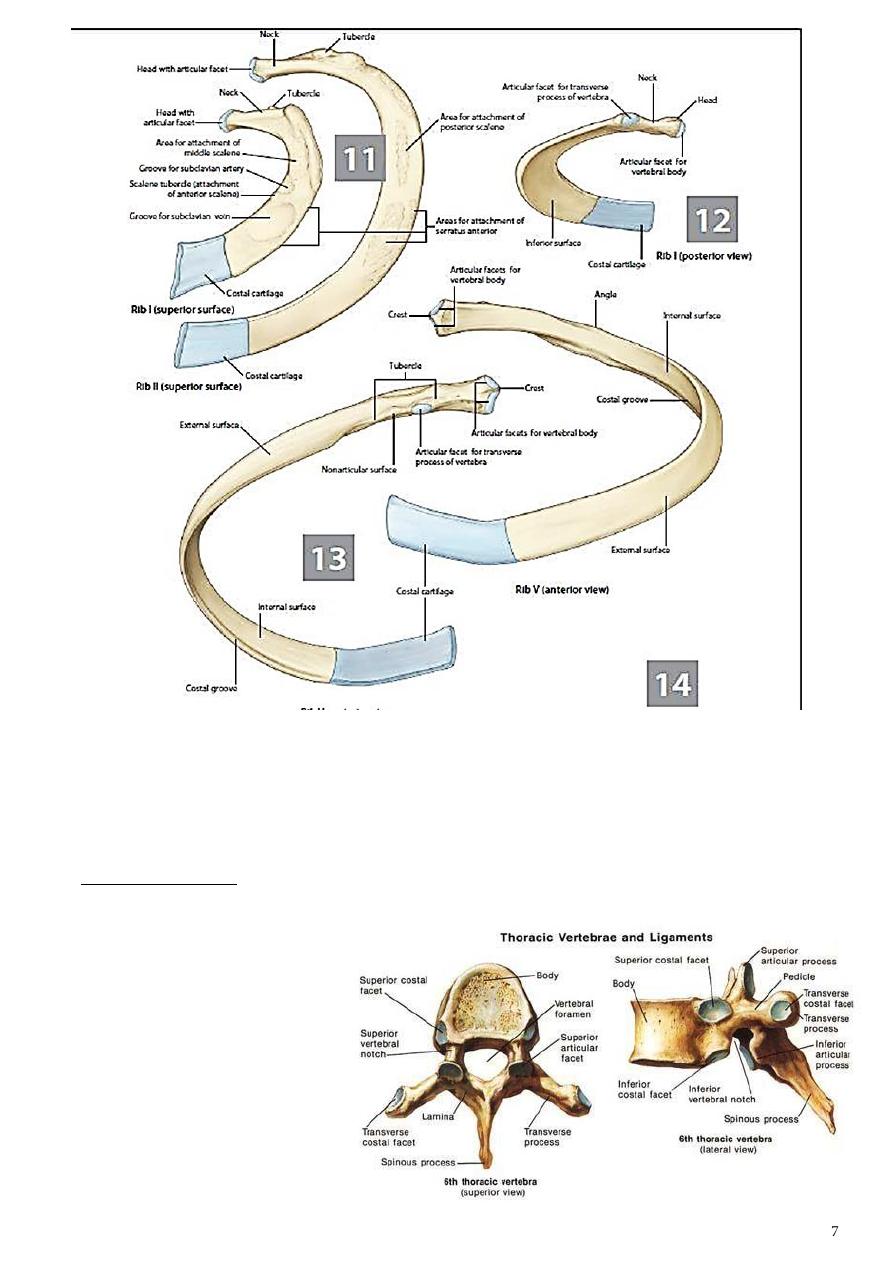
Atypical ribs
The first rib:
-
Short, acutely curved, has superior &
inferior surfaces instead of medial &
lateral surfaces
-
The head has single facet for T1
-
The superior surface is rough &
characterized by the scalene tubercle
for insertion of Scalenus anterior
muscle which separates the area of subclavian vein in front from that of subclavian artery
behind
-
No costal groove
The second rib: Is midway in position between the 1st & typical ribs
The tenth rib: Has only single articular facet on the head.
The eleventh rib: Single head facet, No tubercle facet, poorly defined angle.
The twelfth rib: Is a small & thin piece of bone lacking most of the costal features
General Characteristics of a Vertebra
- The typical vertebra consists of a rounded body anteriorly and a vertebral arch
posteriorly.
- These enclose a space called the vertebral foramen, through which run the spinal cord
and its coverings.
- The vertebral arch gives rise to seven processes: one spinous, two transverse, and four
articular processes are vertically arranged and consist of two superior and two inferior
processes.
- The spinous process, or spine,
is directed posteriorly.
The thoracic spines are:
1- long
2- inclined downward
The body is:
1- medium size
2- heart shaped
Openings of the Thorax
Thoracic outlet: It is narrow aperture communicates the chest cavity with the root of the
neck.
- It is called an outlet because trachea, esophagous and important vessels and nerves
emerge from the thorax here to enter the neck and upper limbs.
- On either side of these structures, the outlet is closed by a dense fascial layer called the
suprapleural membrane.
- The opening is attached at its apex to the tip of the transverse process of the C7,
laterally by the medial borders of the 1st ribs and their costal cartilages, and anteriorly
by the superior border of the manubrium sterni.
- It is obliquely placed.
- It protects the underlying cervical pleura and resists the changes in intrathoracic
pressure occurring during respiratory movements.
The thoracic cavity communicates with the abdomen through a large opening which is
bounded
1- posteriorly by the 12th thoracic vertebra
2- laterally by the curving costal margin
3- and anteriorly by the xiphisternal joint.
- Through this large opening, which is closed by the diaphragm, pass the esophagus and
many large vessels and nerves, all of which pierce the diaphragm.

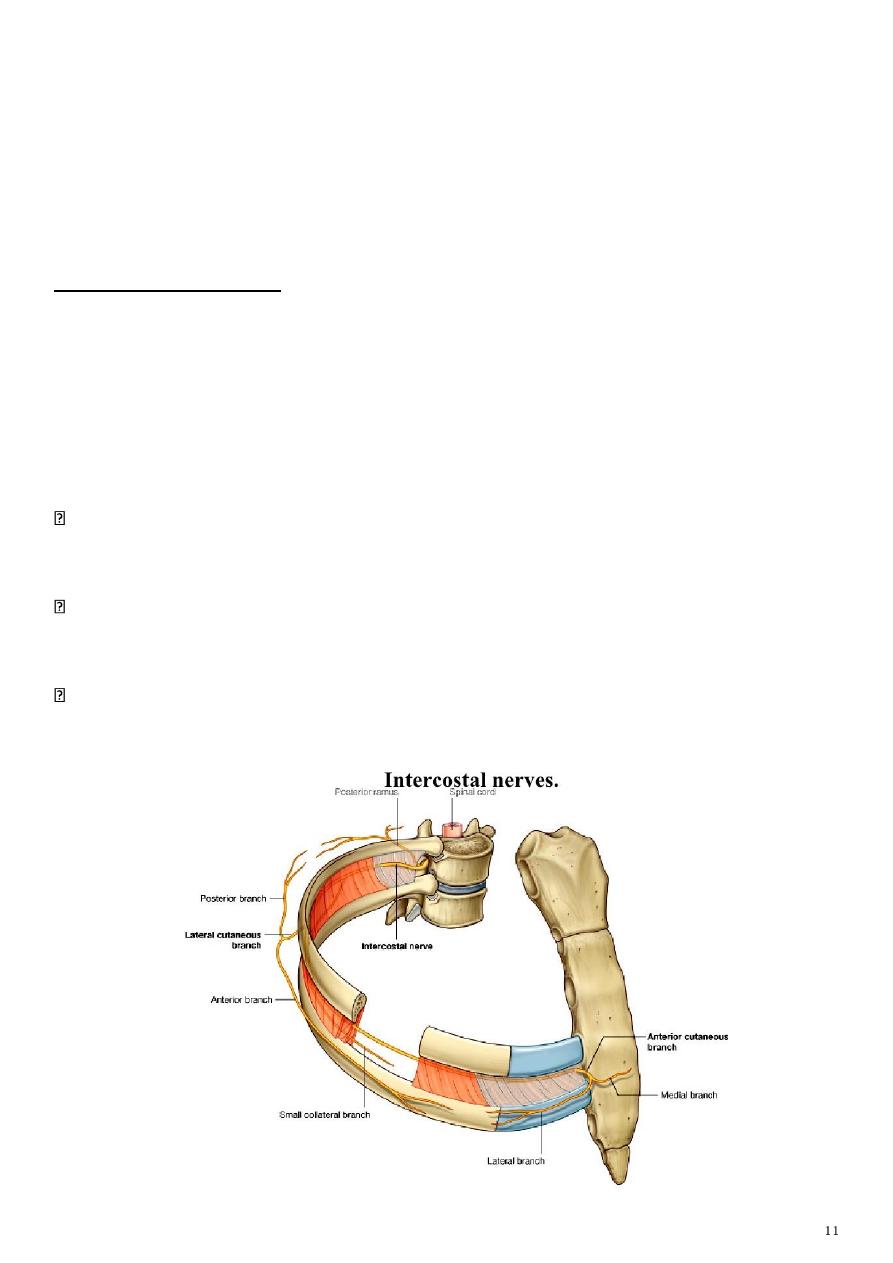
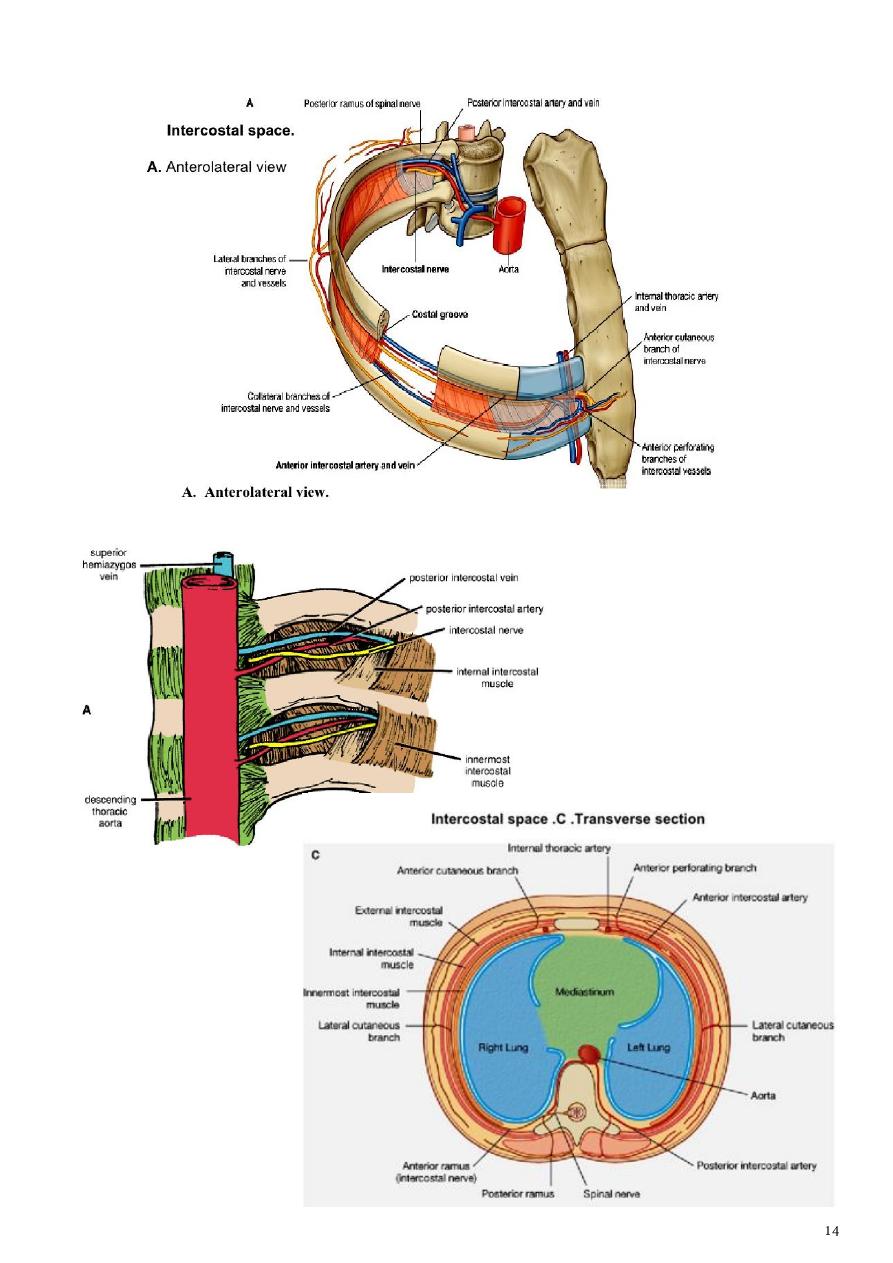
Intercostal Spaces
The spaces between the ribs contain three muscles of respiration:
1. The external intercostal m.
2. The internal intercostal m.
3. The innermost intercostal m. This muscle is lined internally by the endothoracic fascia,
which is lined internally by the parietal pleura.
- The intercostal nerves and blood vessels run between the intermediate and deepest
layers of muscles
- They are arranged in the following order from above downward: intercostal vein,
intercostal artery, and intercostal nerve (i.e., VAN).
The external intercostal muscle
1. It forms the most superficial layer.
2. Its fibers are directed downward and forward from the inferior border of the rib above to
the superior border of the rib below.
3. The muscle extends forward to the costal cartilage where it is replaced by an
aponeurosis, which is named as the anterior (external) intercostal membrane
The internal intercostal muscle
1. It forms the intermediate layer.
2. Its fibers are directed downward and backward from the subcostal groove of the rib
above to the upper border of the rib below.
3. The muscle extends backward from the sternum in front to the angles of the ribs behind,
where the muscle is replaced by an aponeurosis, which is named as the posterior (internal)
intercostal membrane
The innermost intercostal muscle
1. It forms the deepest layer. It is an incomplete muscle layer and crosses more than one
intercostal space within the ribs.
2. It is related internally to endothoracic fascia and parietal pleura and externally to the
intercostal nerves and vessels. The innermost intercostal muscle can be divided into three
portions, which are more or less separate from one another.
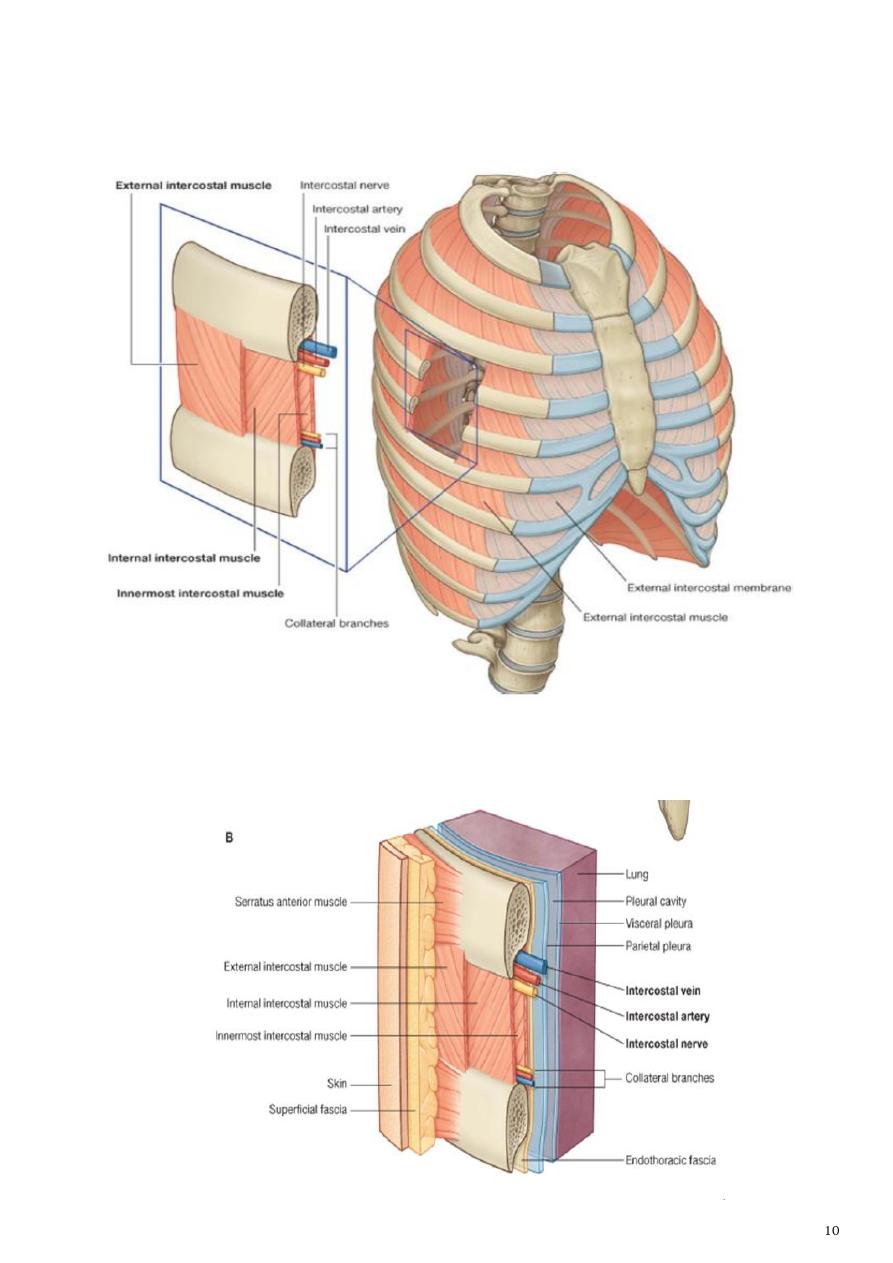
Nerve Supply of I.C.M
1- The intercostal muscles are supplied by the corresponding intercostal nerves.
2- The intercostal nerves and blood vessels (the neurovascular bundle) run between the
middle and innermost layers of muscles .
3- They are arranged from above downward: intercostal vein, intercostal artery, and
intercostal nerve (i.e., VAN).
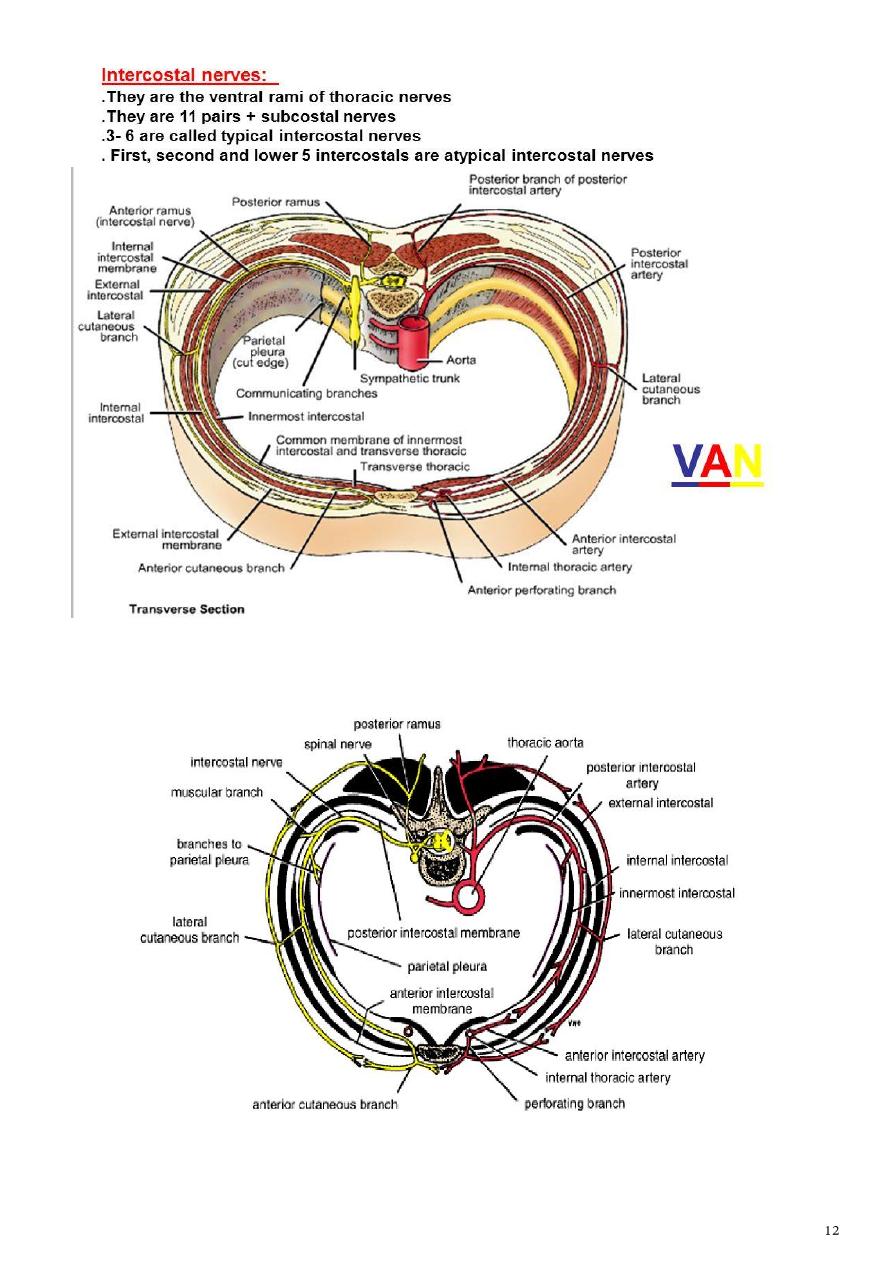
The intercostal nerves:
a- The upper 6 thoracic nerves will be distributed to the thorax supplying the thoracic wall
and intercostal muscles
b- while T7, T8, T9 leave their intercostal spaces anteriorly (after innervating the structures
within) and pass to the anterior abdominal wall.
c- T10 and T11ribs pass directly into the abdominal wall because of the fact that the
corresponding ribs are floating. will pass deep and inter to the abdomen.
They give branches:
Collateral branches; each nerve gives a collateral branch which passes below & parallel to
the main nerve, these branches contain most of the motor fibers & they are the nerves
which supply the intercostal muscles.
Lateral cutaneous branches; arise at the midaxillary line from the remaining part of the
nerve, each divides into anterior & posterior branches which meet the lateral branches of
the anterior & posterior cutaneous nerves.
Anterior cutaneous branches; are the remaining part of the spinal nerve, pierce the
muscles lateral to the sternum & ends into lateral (large) & medial (small) branches.
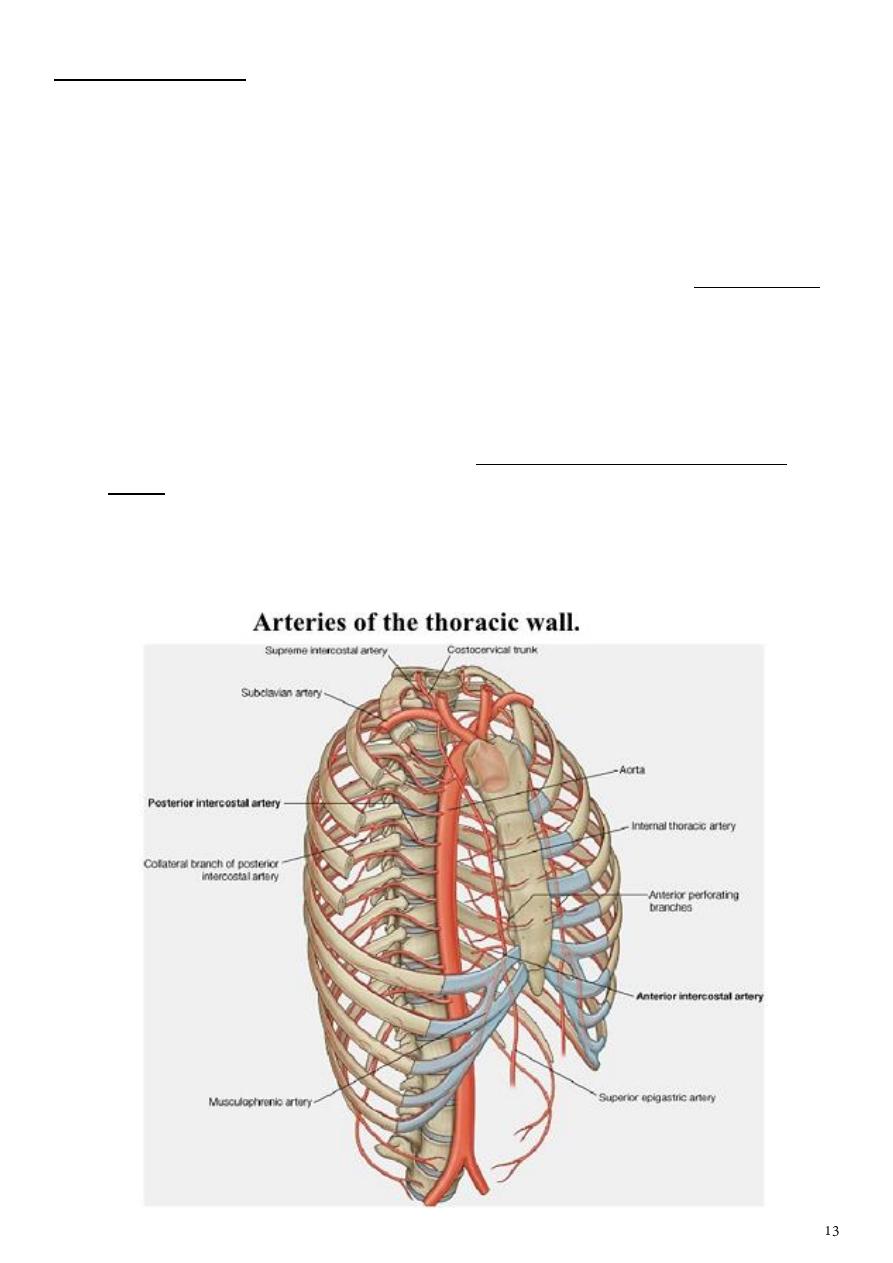
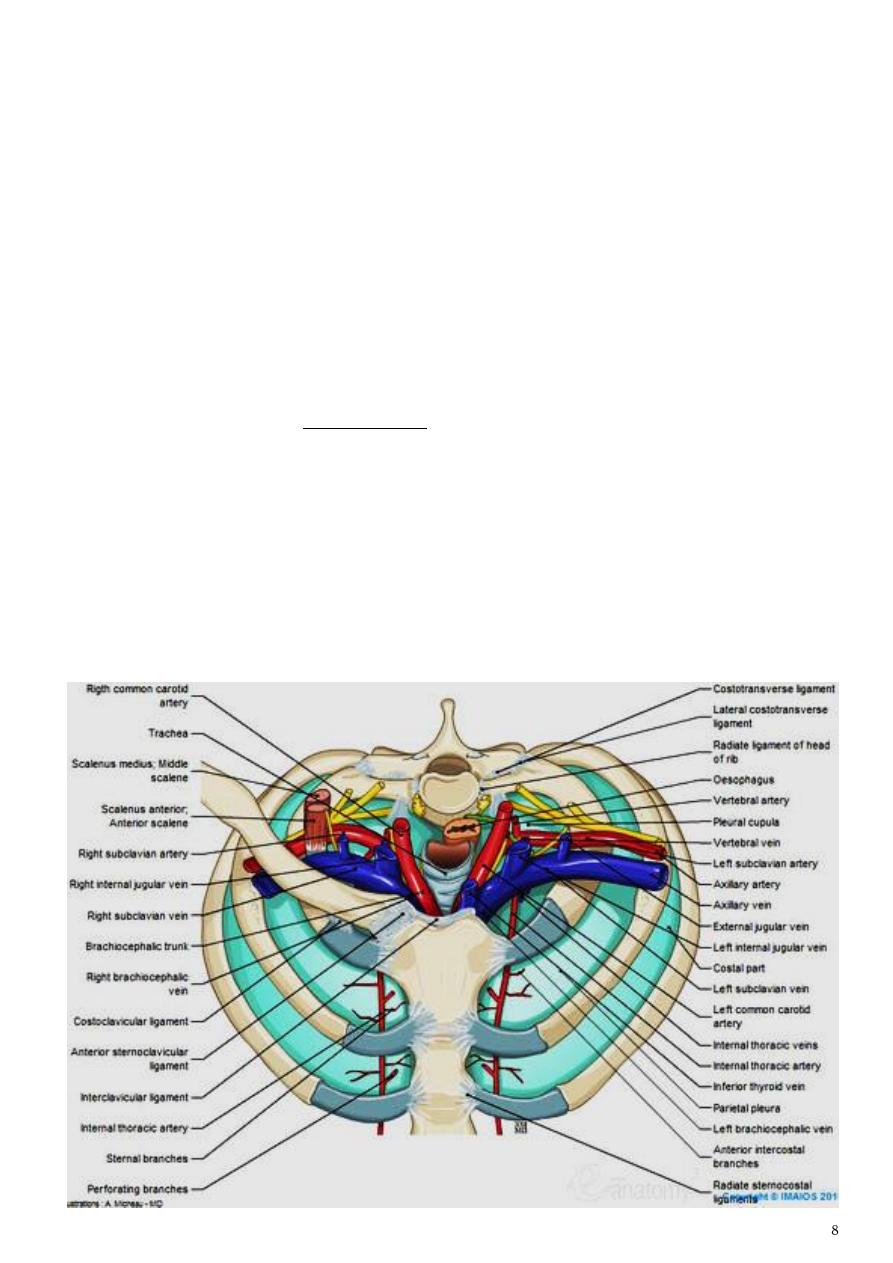
Intercostal Arteries
Each intercostal space contains a large single posterior intercostal artery and two small
anterior intercostal arteries.
1- The anterior intercostal arteries
a- The anterior intercostal arteries of the first six spaces are branches of the internal
thoracic artery, which arises from the first part of the subclavian artery.
b- The anterior intercostal arteries of the lower spaces are branches of the
musculophrenic artery, one of the terminal branches of the internal thoracic artery.
- Each intercostal artery gives off branches to the muscles, skin, and parietal pleura. Those
of the 2nd, 3rd & 4th spaces supply the mammary gland in female.
2- The posterior intercostal arteries
a- The posterior intercostal arteries of the first two spaces are branches from the
superior intercostal artery, a branch of the costocervical trunk of the subclavian
artery.
b- The posterior intercostal arteries of the lower nine spaces are branches of the
descending thoracic aorta.
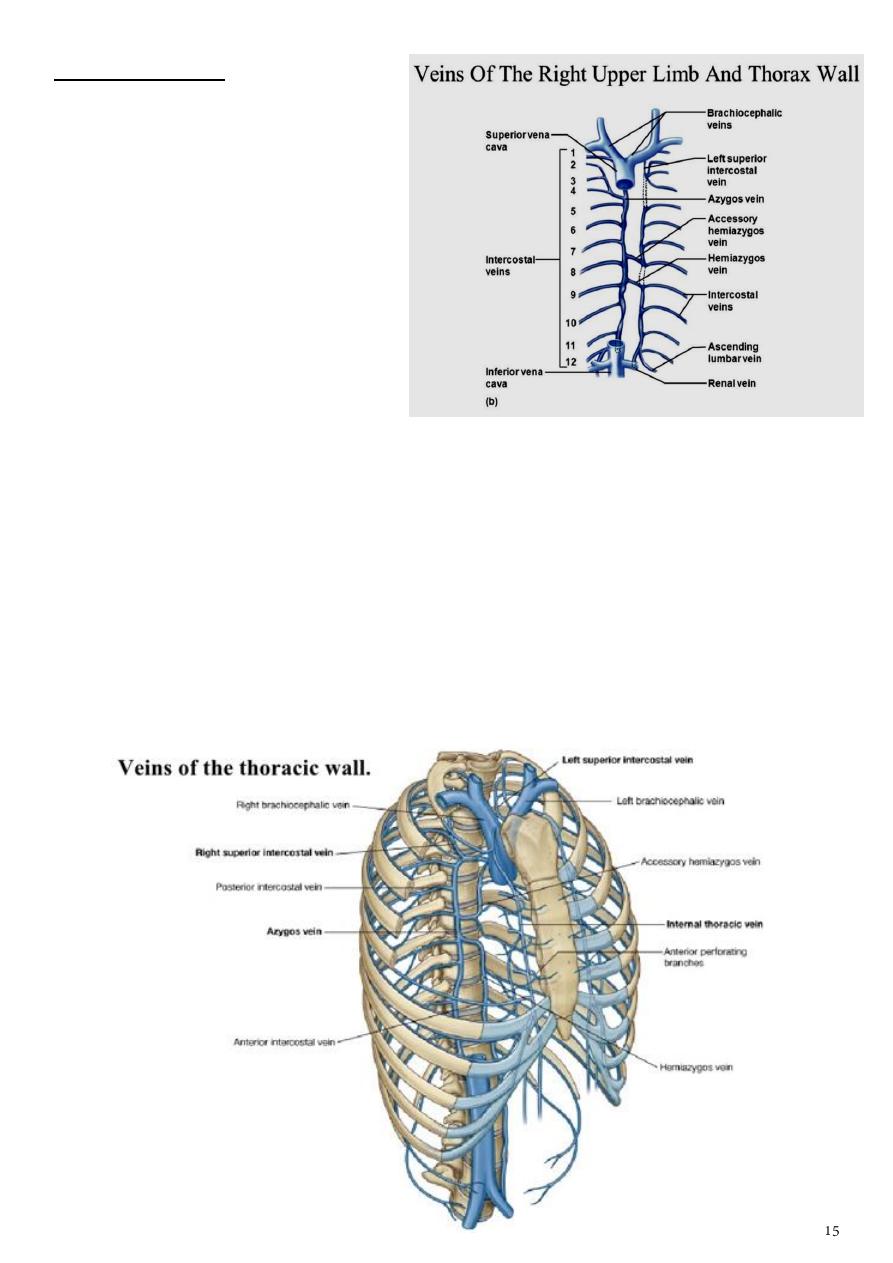
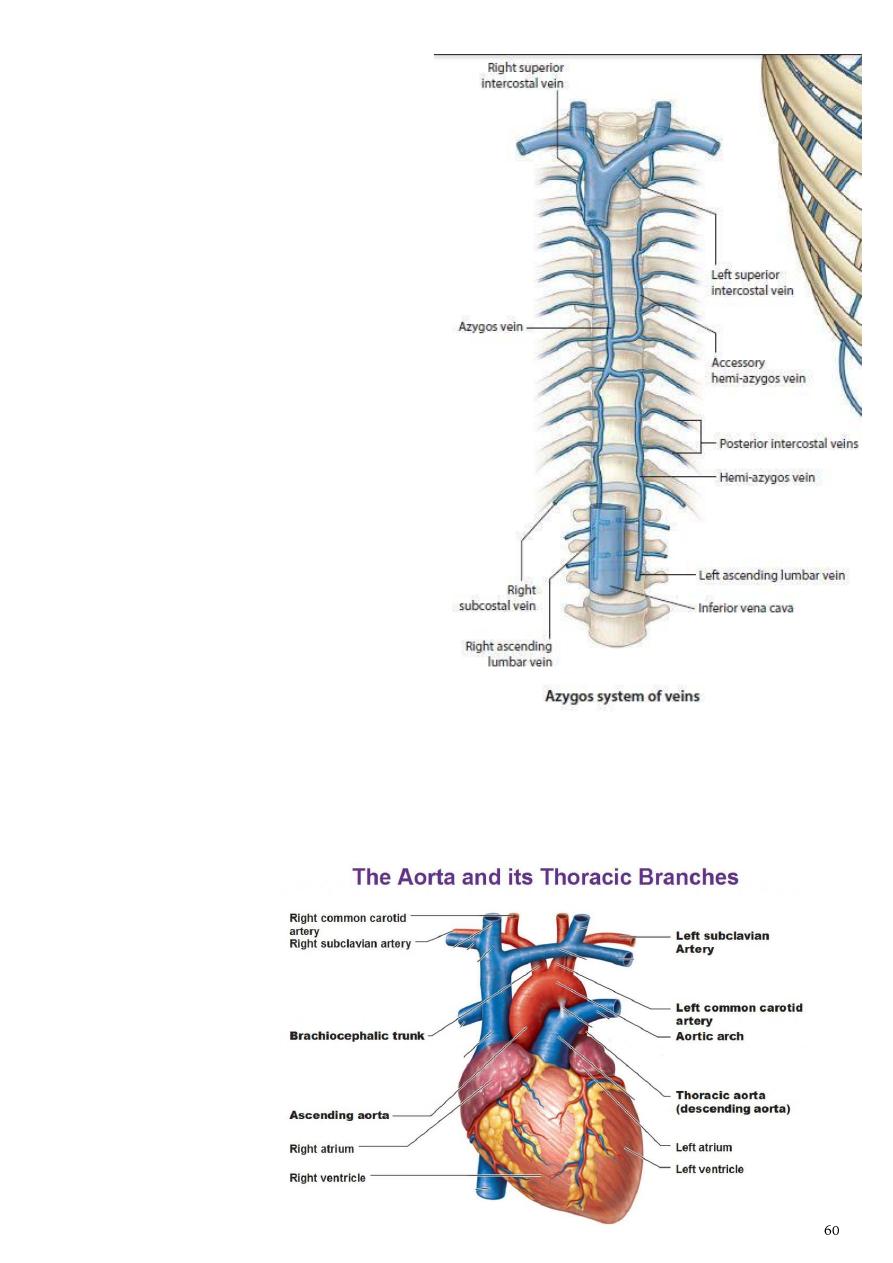
Intercostal veins:
- They accompany the arteries & have
the same course, with some variations:
1- The anterior intercostal veins
drain into the internal thoracic and
the musculophrenic veins. The
internal thoracic veins end in the
corresponding brachiocephalic vein
2- The posterior intercostal veins
a-
The highest intercostal vein (1st
posterior intercostal) drains on
each side to the brachiocephalic or
vertebral veins after passing over the pleura of the lung apex
b-
The 2nd & 3rd and sometimes the 4 th posterior intercostal veins unite to form the
superior intercostal vein which drains on the left in the brachiocephalic vein & on the
right in the azygos arch.
c-
The eight lower right intercostal veins drain to azygos vein.
d-
The fourth to the eighth left intercostal veins will unite to form the Accessory
Hemiazygos Vein which joins the azygos vein at the level of the seventh thoracic
vertebra
e-
The 9th to 11 th post. left intercostal veins drain into the Hemiazygos Vein which join
the azygos vein that empty to superior vena cava.
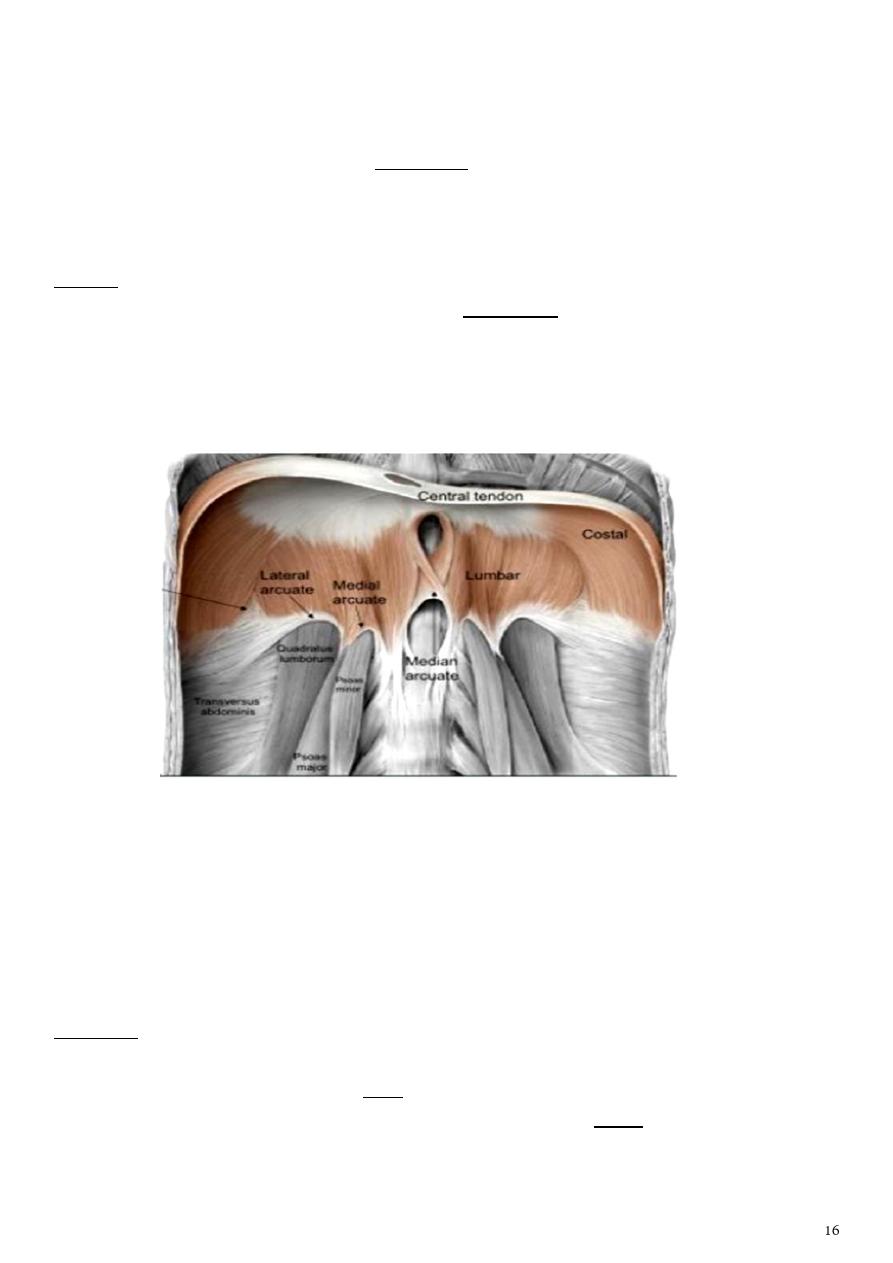
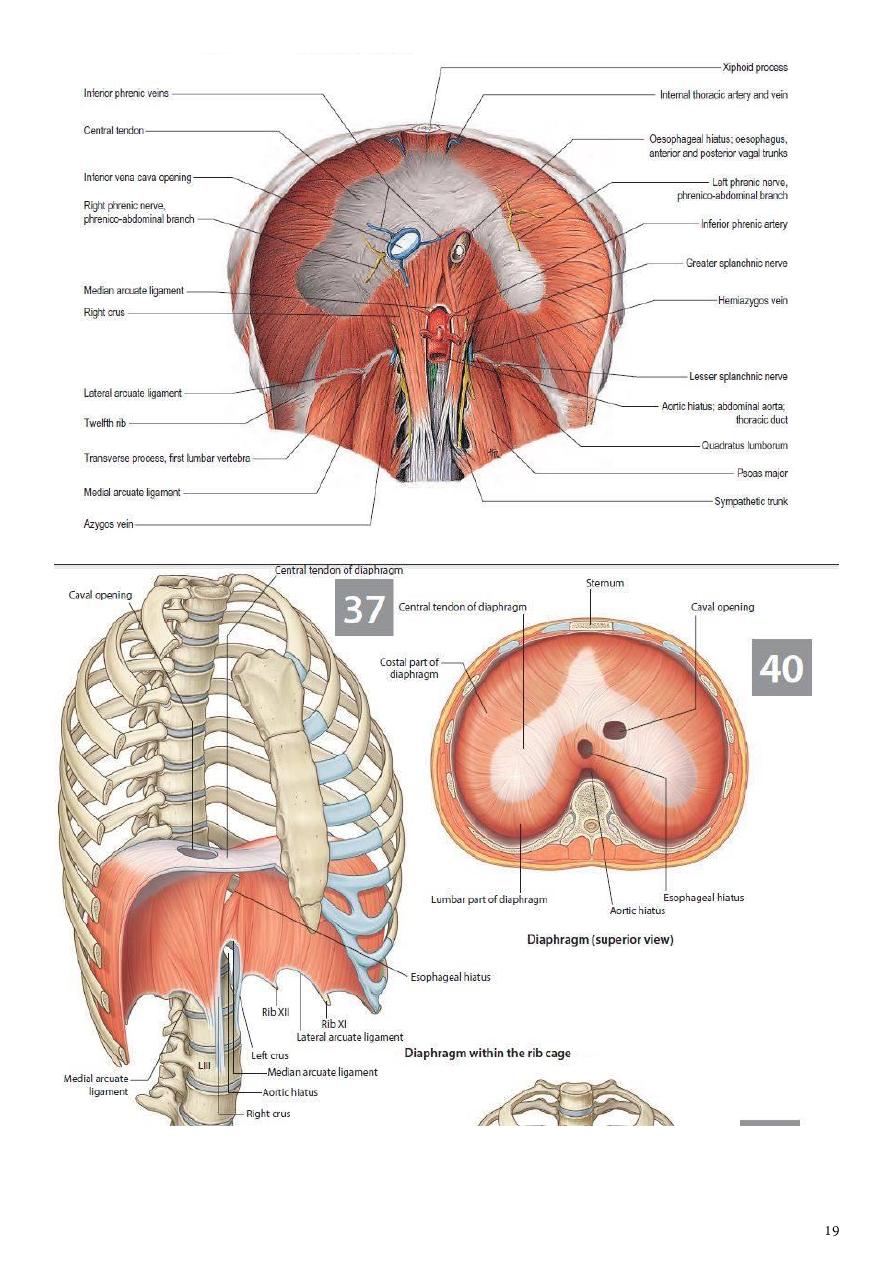
Diaphragm
1- The diaphragm is a thin muscular and tendinous septum, dome shaped that separates
the chest cavity above from the abdominal cavity below.
2- It is the most important muscle of respiration.
3- It consists of a peripheral muscular part, which arises from the margins of the thoracic
opening, and a centrally placed tendon.
Origin :
The origin of the diaphragm can be divided into three parts:
1. Sternal part arising from the posterior surface of the xiphoid process.
2. Costal part arising from the deep surfaces of the lower six ribs and their costal
cartilages.
3. Vertebral part arising by vertical columns or crura and from the arcuate ligaments.
- The right crus arises from the sides of the bodies of the first three lumbar vertebrae and
the intervertebral discs
- the left crus arises from the sides of the bodies of the first two lumbar vertebrae and the
intervertebral disc.
- Lateral to the crura the diaphragm arises from the medial and lateral arcuate ligaments
- The two crura are connected by a median arcuate ligament
Insertion:
The diaphragm is inserted into a central tendon , which is shaped like three leaves.
- Some of the muscle fibers of the right crus pass up to the left and surround the
esophageal orifice in a slinglike loop. These fibers appear to act as : a sphincter and
possibly assist in the prevention of regurgitation of the stomach contents into the
thoracic part of the esophagus.
Nerve Supply of the Diaphragm
1. Motor nerve supply: The right and left phrenic nerves (C3, 4, 5).
2. Sensory nerve supply: The parietal pleura and peritoneum covering the central surfaces
of the diaphragm are from the phrenic nerve and the periphery of the diaphragm is from
the lower six intercostal nerves.
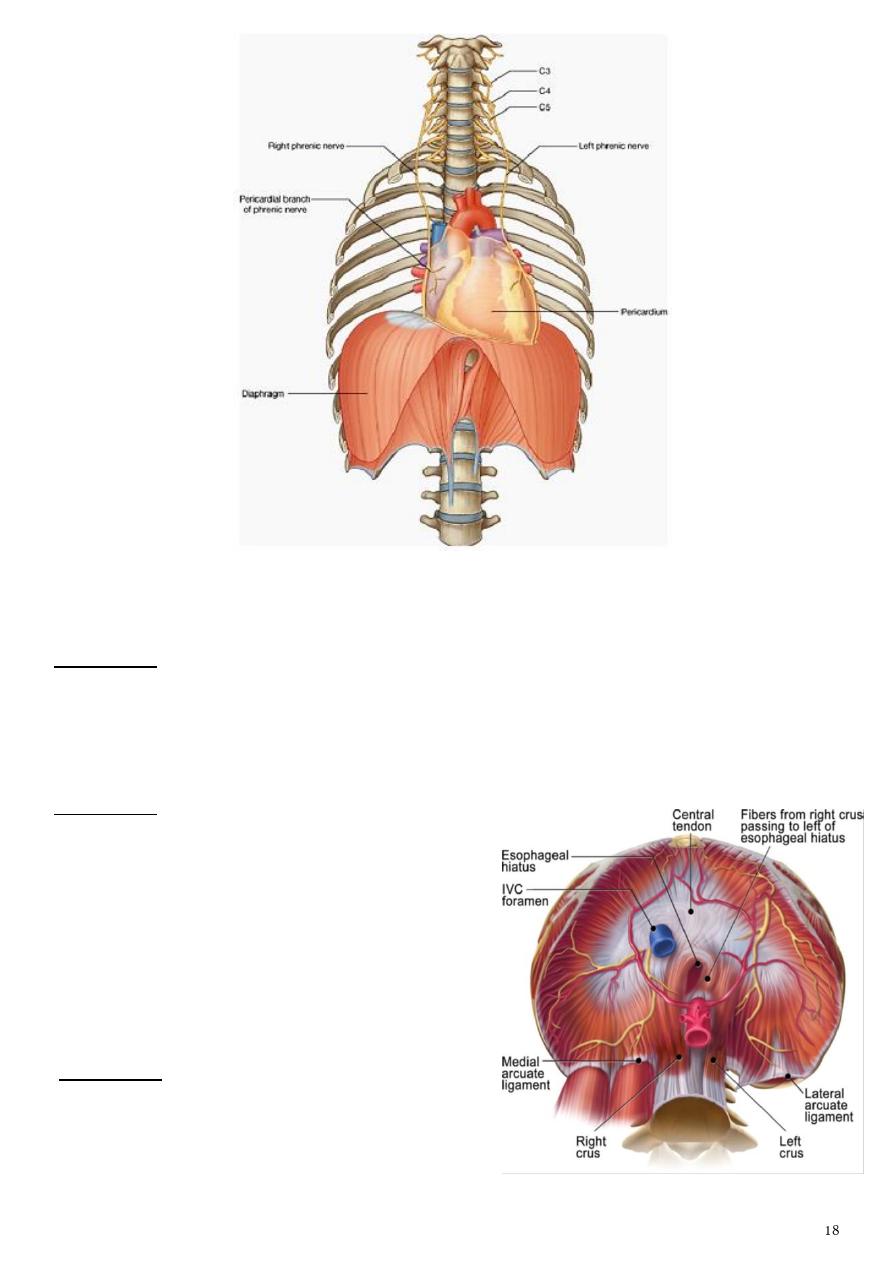
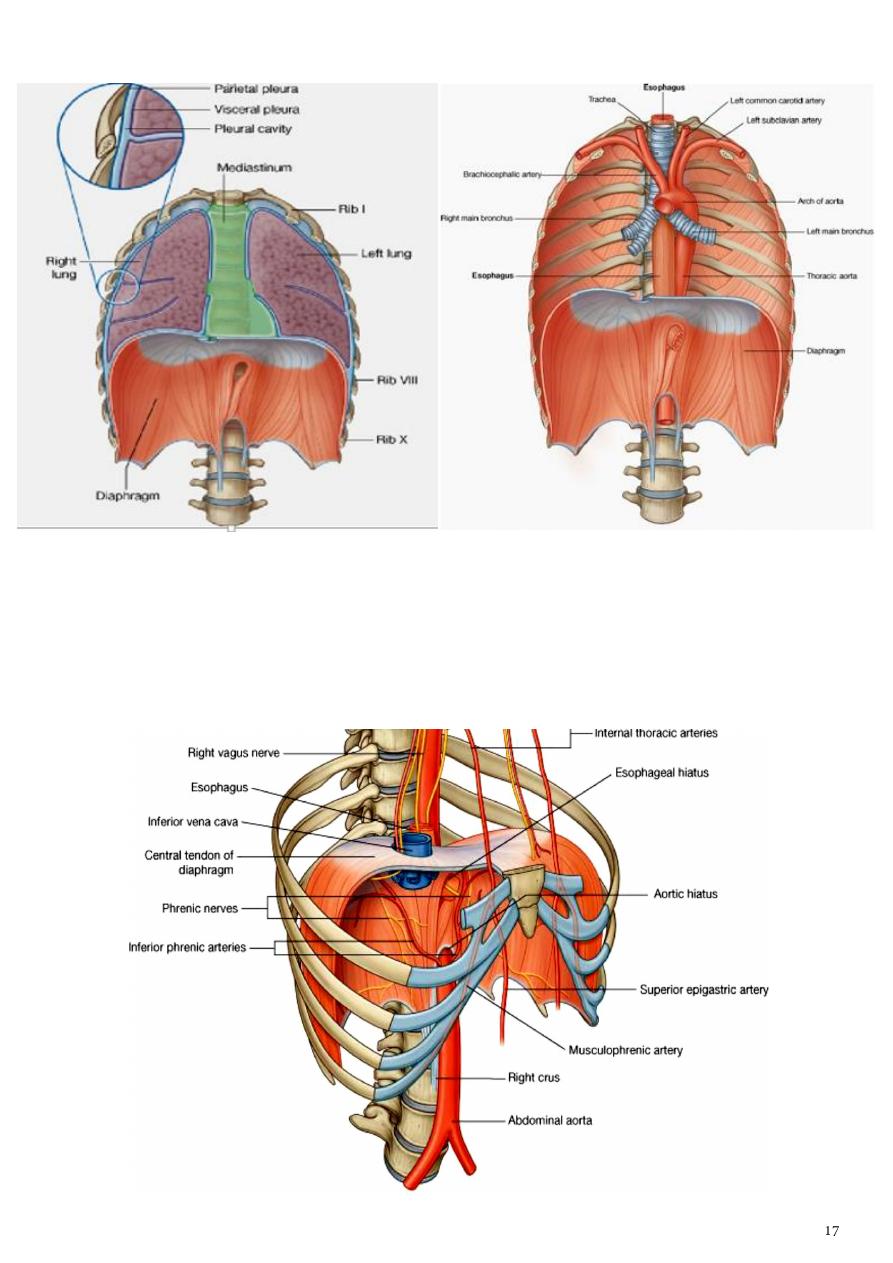
Openings in the Diaphragm:
A- Caval: T8 , on the Rt of the central tendon
It transmits:
1-
the inferior vena cava
2-
terminal branches of the right phrenic nerve.
B- Oesophageal: T10, in the fibers of the Lt crus.
It transmits:
1-
the esophagus
2-
the right and left vagus nerves
3-
the esophageal branches of the left gastric
vessels
4-
the lymphatics from the lower third of the
esophagus.
C- Aortic: T12, in between the 2 crura.
It transmits:
1-
the aorta
2-
the thoracic duct
3-
the azygos vein.
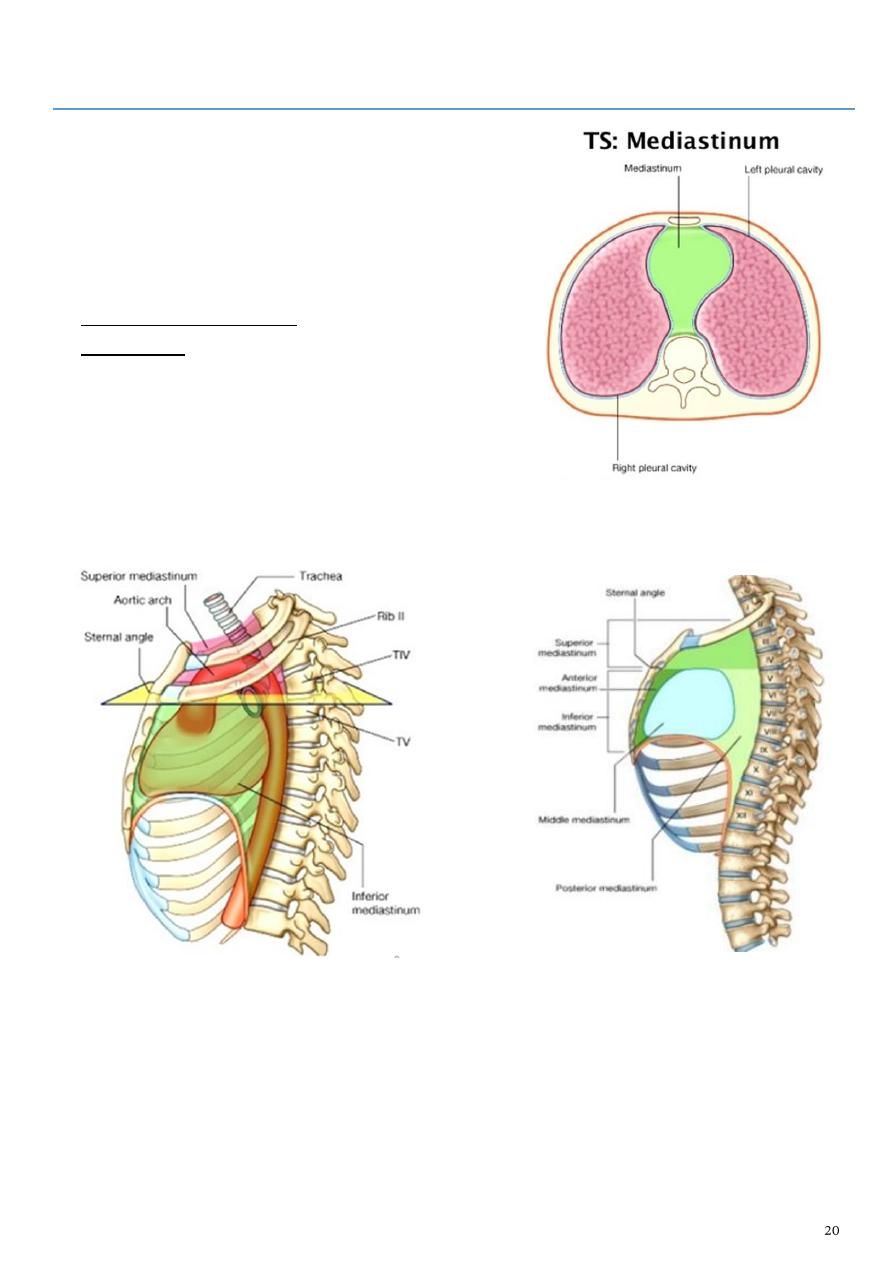
Part2
: Mediastinum
- The mediastinum is divided into superior and
inferior mediastina by an imaginary plane passing
from the sternal angle anteriorly to the lower border
of the body of the T4 posteriorly.
- The inferior mediastinum is subdivided by
pericardium into :
1- the middle mediastinum, which consists of the
pericardium and heart
2- the anterior mediastinum, which is a space between
the pericardium and the sternum
3- the posterior mediastinum, which lies between the
pericardium and the vertebral column.
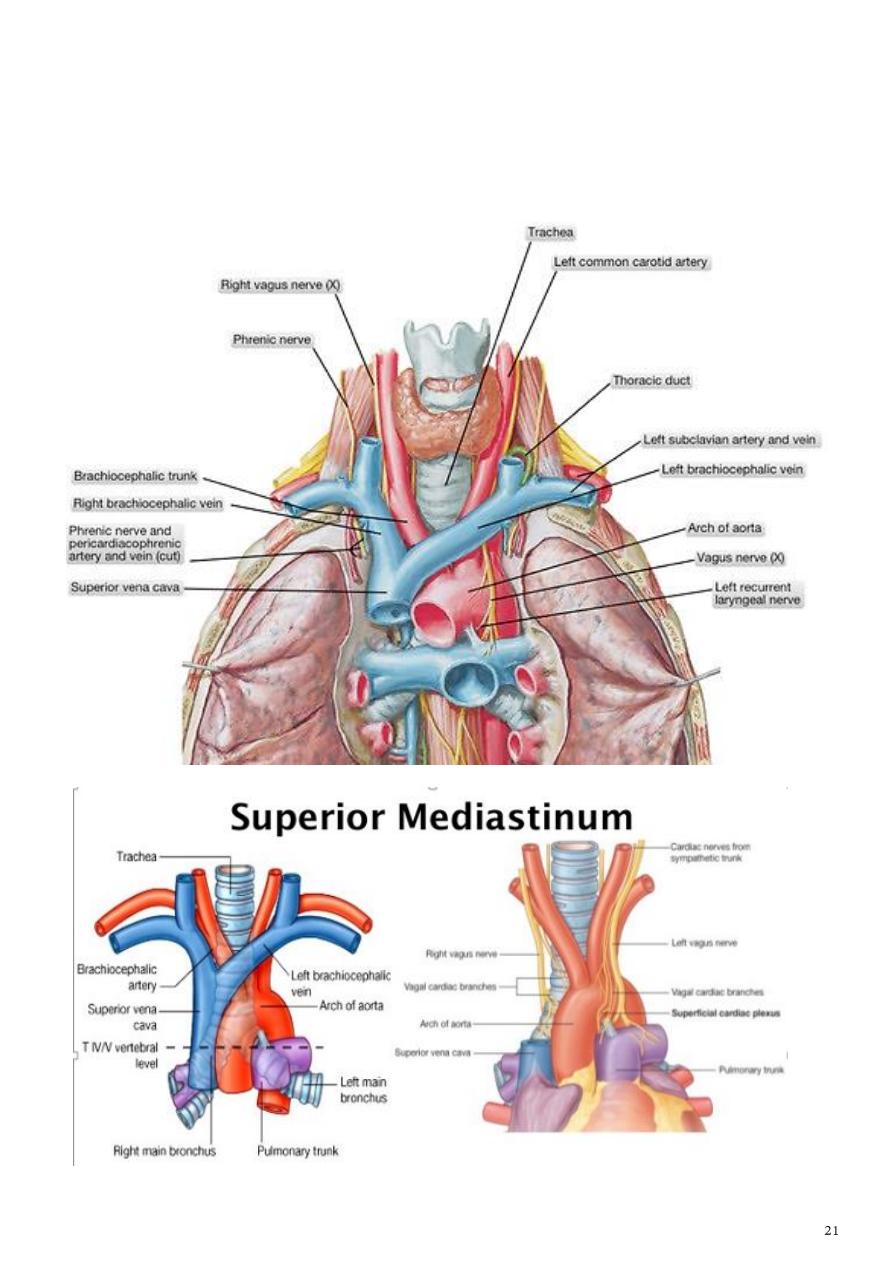
For purposes of orientation, it is convenient to remember that the major mediastinal
structures are arranged in the following order from anterior to posterior:
1- Superior Mediastinum
(a) Thymus, (b) large veins, (c) large arteries, (d) trachea, (e) esophagus and thoracic duct
(f) sympathetic trunks.
2- Inferior Mediastinum
(a) Thymus, (b) heart within the pericardium with the phrenic nerves on each side,
(c) esophagus and thoracic duct, (d) descending aorta, (e) sympathetic trunks.
Anterior mediastinum Middle mediastinum
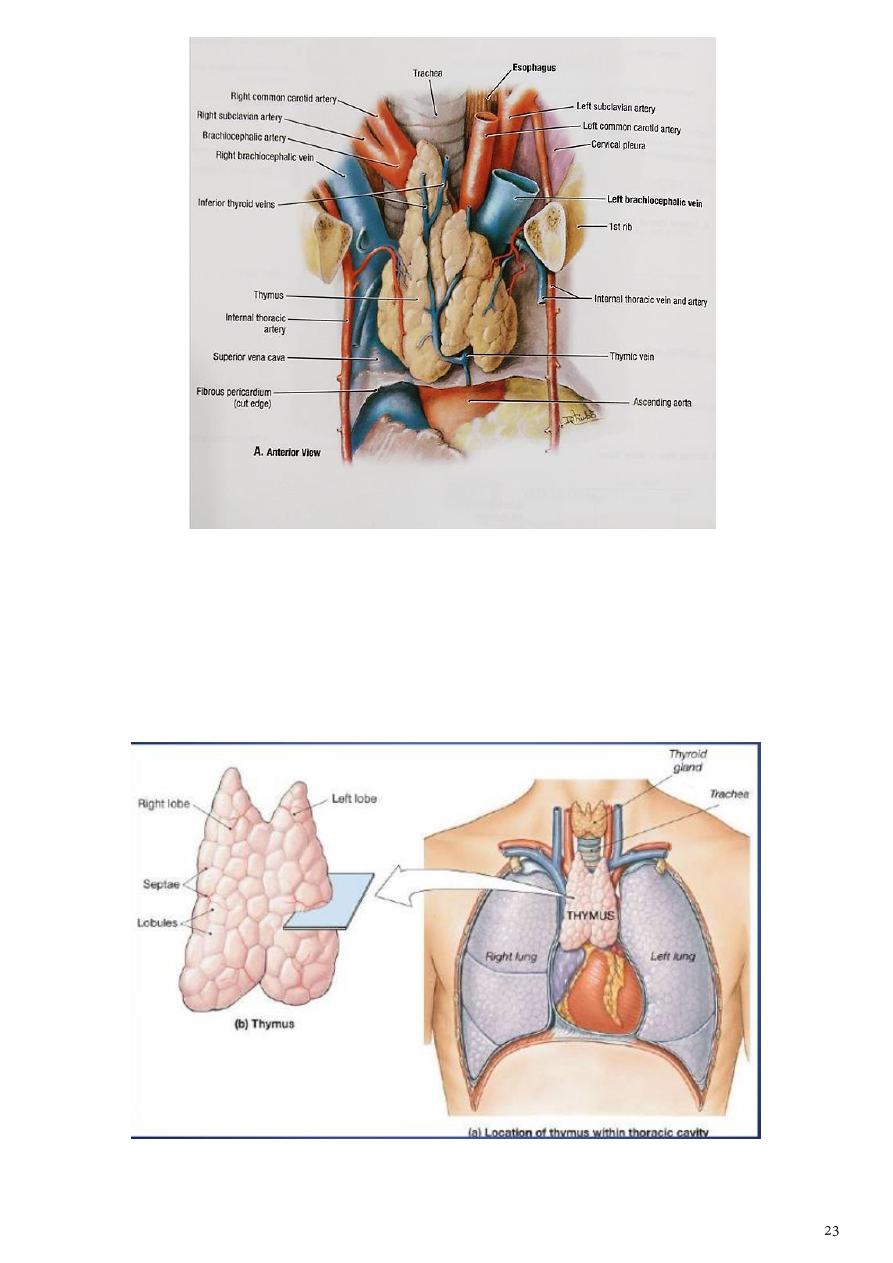
Thymus:
1- Is a flattened, bilobed gland related to the immune system of the body
2- well developed in children &rudimentary in adults.
3- It may extends to the superior mediastinum.
4- The thymus continues to grow until puberty but thereafter undergoes involution.
5- It has a pink, lobulated appearance and is the site for development of T lymphocytes.
6- It is supplied by inferior thyroid A. & internal thoracic artery.
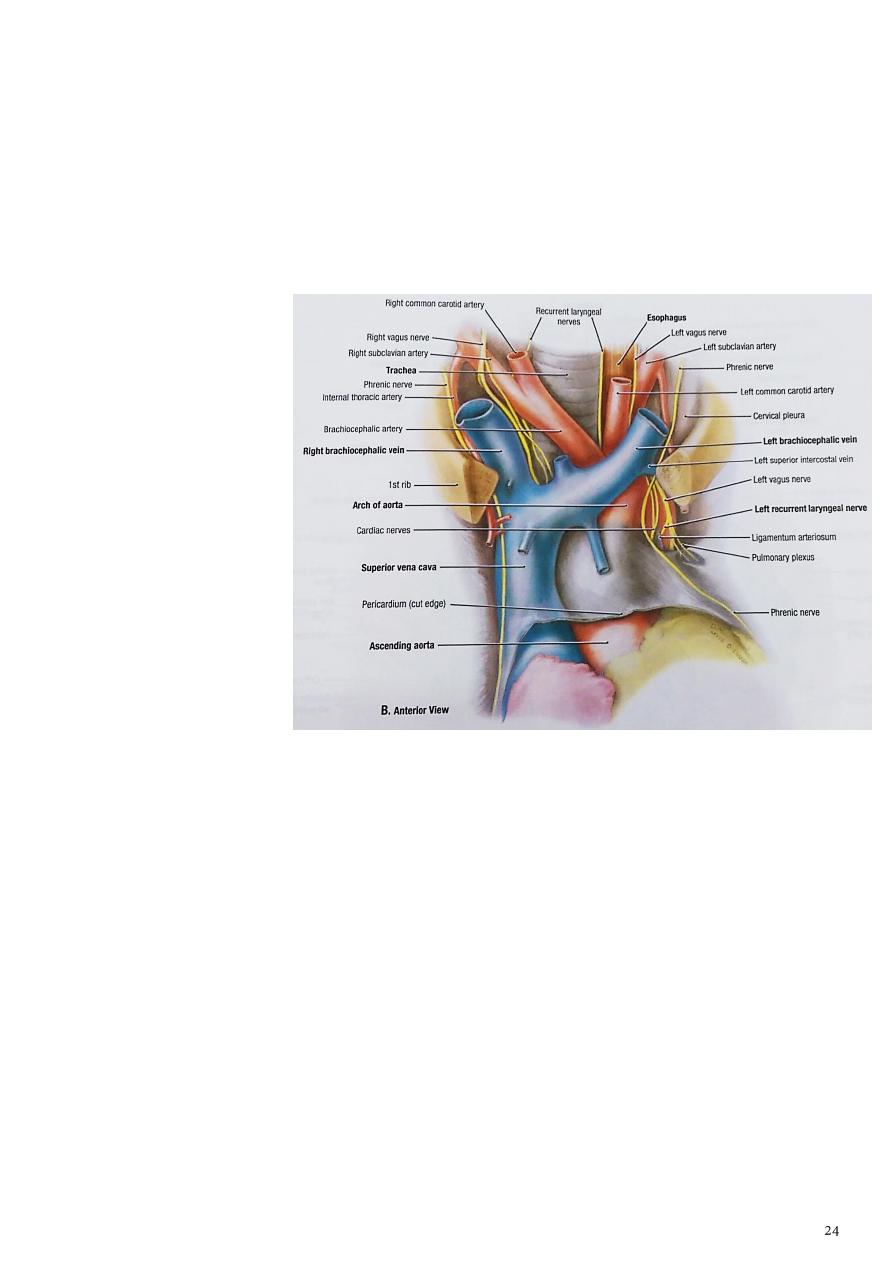
Trachea:
1- It is midline structure begins in the neck as a continuation of the larynx at the lower
border of the cricoid cartilage at the level of the 6th cervical vertebra and ends below at
the carina by dividing into right and left principal (main) bronchi at the level of the
sternal angle (opposite the disc between T4 and T5) n adults
2- the trachea is about (11.25 cm) long and 1 inch (2.5 cm) in diameter.
3- Its wall is reinforced by C-shaped cartilagenous rings which open posteriorly, the gap is
being closed by a muscle strip (trachealis m.)
4- In the chest it is
relatedanteriorly to :
a- the back of sternum
b- thymus gland
c- L.Brachiocephalic v.
d- arch of Aorta
e- L. Subclavian
f- left common carotid
arteries.
Posteriorly to :
a- the esophagus
b- L.recurrent laryngeal
nerve
c- azygos V.
d- Vagi nerves.
Blood Supply of the Trachea
1- The upper two thirds are supplied by the inferior thyroid arteries
2- the lower third is supplied by the bronchial arteries.
Lymph Drainage of the Trachea
The lymph drains into the pretracheal and paratracheal lymph nodes and the deep cervical
nodes.
Nerve Supply of the Trachea
1- The sensory nerve supply is from the vagi and the recurrent laryngeal nerves.
2- Sympathetic nerves supply the trachealis muscle.
The esophagus
:
1- It is muscular tube, 25 cm long
2- lies in the midline with tendency to incline to
the left side as it descends.
3- It pierces the diaphragm to the left of the
midline.
4- It starts at C6 level, and passes through the
diaphragm at the level of the T10 to join the
stomach.
5- It has 3 main constrictions,at C6, where the
left main bronchus passes in front of it
compressing it & at the diaphragmatic
orifice.
6- The esophagus is related anteriorly to
trachea, left recurrent laryngeal n.
7- It lies on the Rt of the aortic arch &
descending thoracic aorta, as the esoph.
8- tends to attain Lt position & the aorta tends
to take midline position, the esopha. will
pass anterior to the thoracic aorta crossing it
at the level of T8 vertebra.
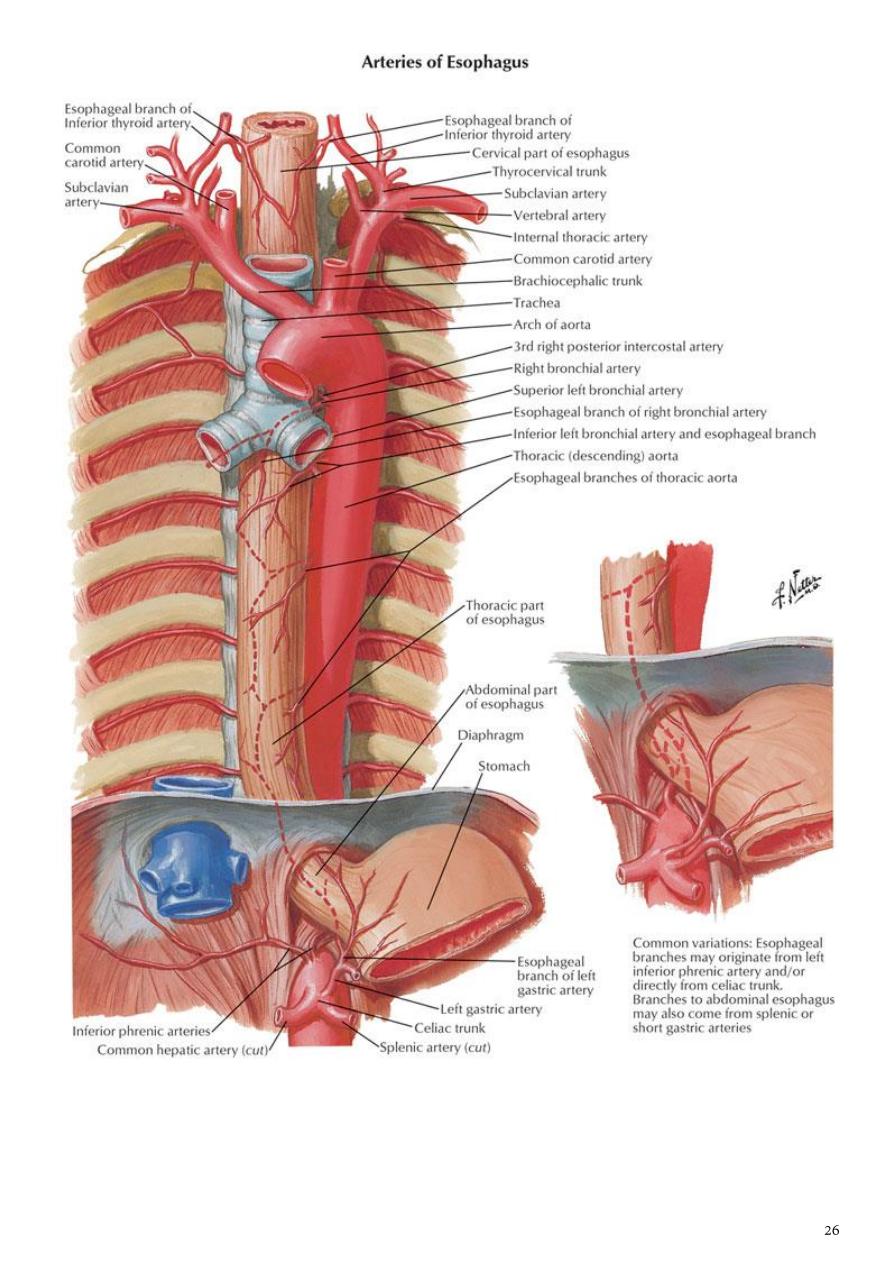
Blood Supply of the Esophagus
a- The upper third of the esophagus is supplied by the inferior thyroid artery
b- the middle third by esophageal branches from the bronchial arteries & descending
thoracic aorta
c- the lower third by branches from the left gastric artery.
- The veins from the upper third drain into the inferior thyroid veins, from the middle third
into the azygos veins, and from the lower third into the left gastric vein, a tributary of the
portal vein.
Lymph Drainage of the Esophagus
Lymph vessels:
a- from the upper third of the esophagus drain into the deep cervical nodes
b- from the middle third into the superior and posterior mediastinal nodes
c- from the lower third into nodes along the left gastric blood vessels and the celiac nodes.
Nerve Supply of the Esophagus
The esophagus is supplied by parasympathetic and sympathetic fibers via the vagi and
sympathetic trunks and the esophageal nerve plexus.
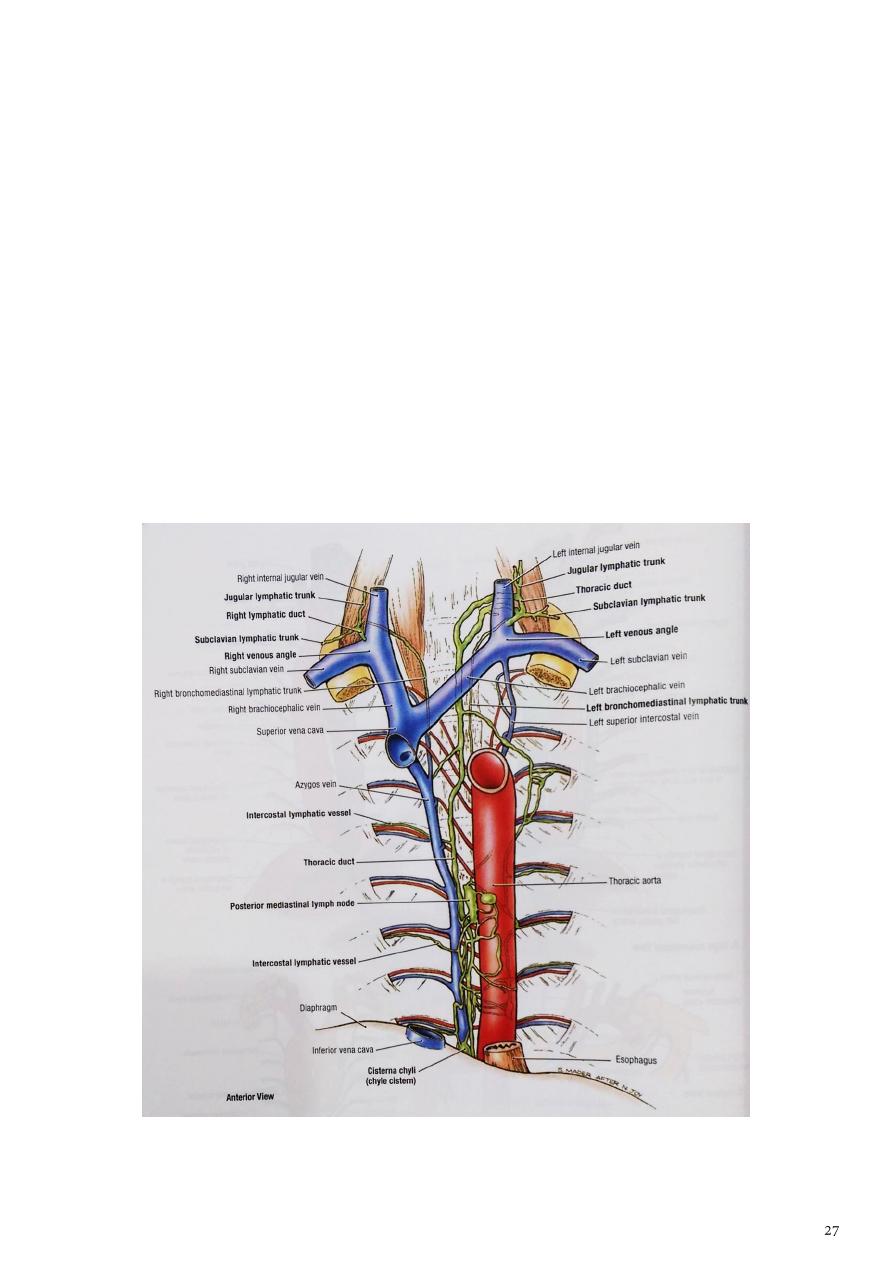
Thoracic Duct
1- The thoracic duct begins in the abdomen as a dilated sac, the cisterna chyli which is
formed in the posterior abdominal wall at L2 level by union of the lumbar & intestinal
lymph trunks.
2- It ascends through the aortic opening in the diaphragm, on the right side of the
descending aorta.
3- It then runs upward to enter the root of the neck. Here, it bends laterally behind the
carotid sheath and in front of the vertebral vessels.
4- It crosses the subclavian artery to enter the beginning of the left brachiocephalic
vein.
5- At the root of the neck, the thoracic duct receives the left jugular, subclavian, and
bronchomediastinal lymph trunks, although they may drain directly into the adjacent
large veins.
6- The thoracic duct drains the lymph from the whole body except the right side above
the diaphragm which drain by Rt lymphatic duct.
Part3
: The lung
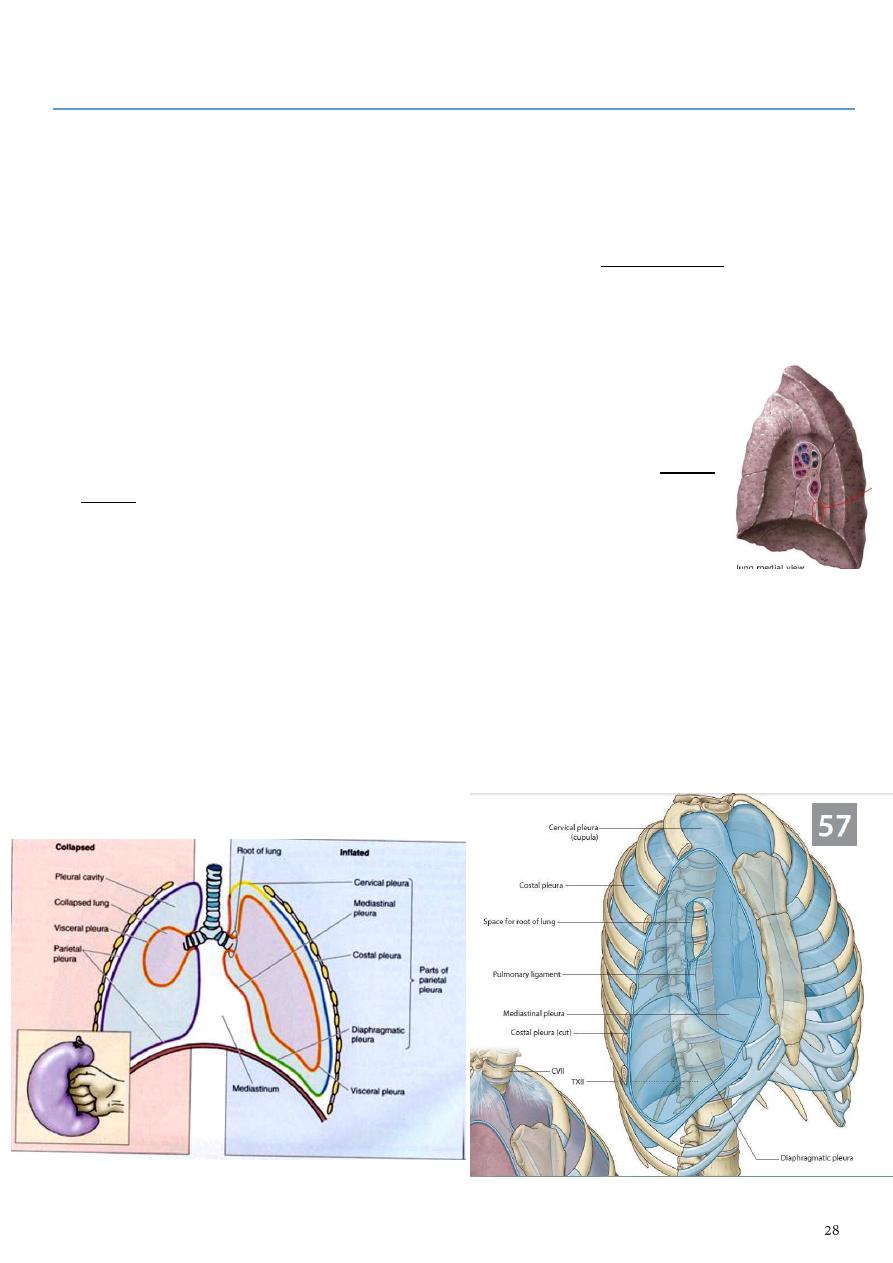
Pleura
1- This is a closed serous sac
2- invaginated from the mediastinal side by the lung as if a balloon is invaginated by a fist.
3- It consists of 2 layers which become continuous with each other around the lung hilum.
a- The inner layer is in direct contact with the lung is the visceral pleura which is
adherent to the lung tissue& it enters lung fissures.
b- The outer layer (parietal pleura) lines the thoracic wall so it is divided according to
its position into: costal, diaphragmatic, mediastinal & cervical pleura.
4- The two layers are separated from one another by a slit like space (pleural
cavity) which normally contains a small amount of tissue fluid (pleural
fluid) which forms a thin film to reduce friction.
5- The two layers become continuous with one another by means of a cuff of
pleura that surrounds the structures at the hilum of lung. (To allow
movement of the pulmonary vessels and large bronchi during respiration)
the pleural cuff hangs down as a loose fold called the pulmonary ligament.
A-
The cervical pleura extends up into the neck, lining the undersurface of the
suprapleural membrane. It reaches a level 1 to 1.5 inch (2.5 to 4 cm) above the
medial third of the clavicle.
B-
The costal pleura lines the inner surfaces of the ribs, the costal cartilages, the
intercostal spaces, the sides of the vertebral bodies, and the back of the sternum.
C-
The diaphragmatic pleura covers the thoracic surface of the diaphragm.
D-
The mediastinal pleura covers and forms the lateral boundary of the mediastinum.
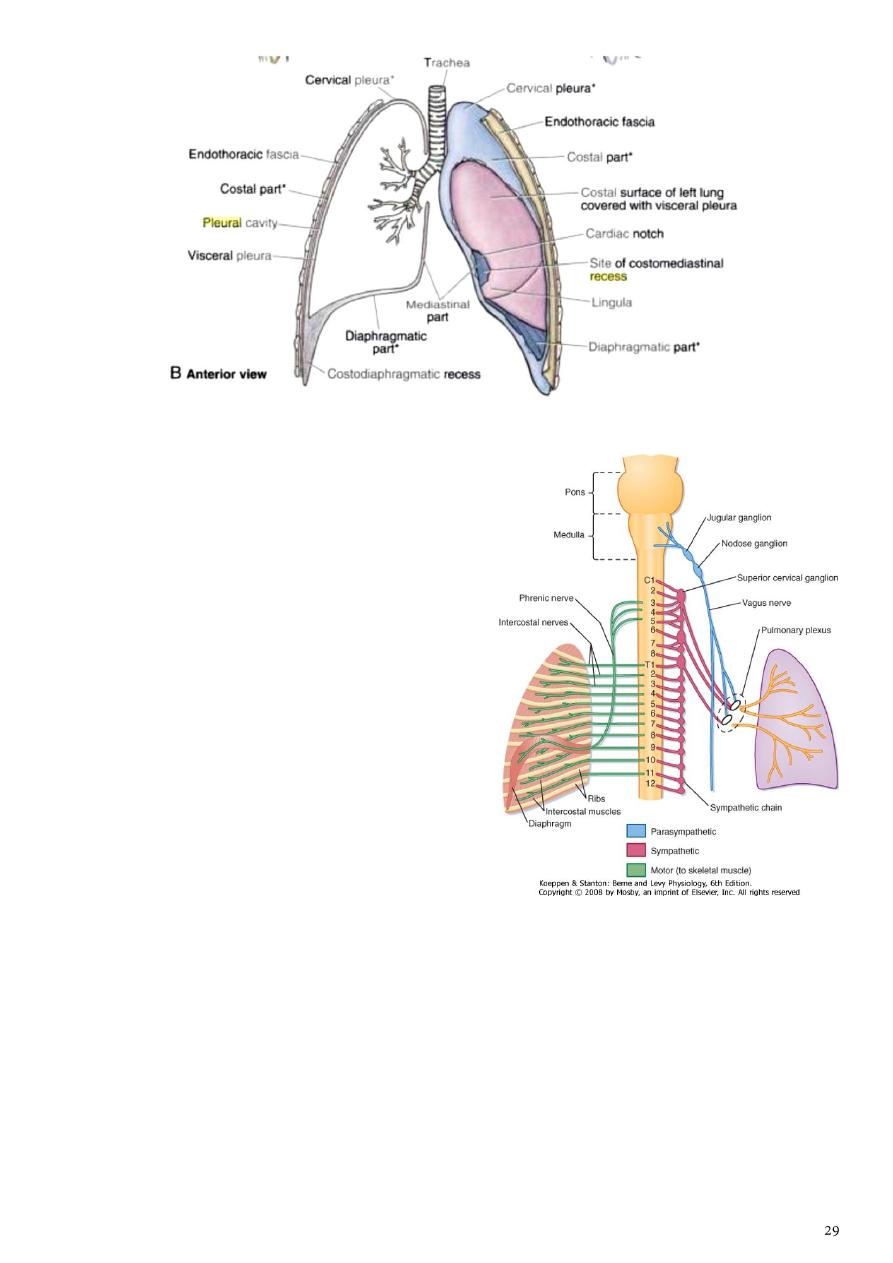
Nerve Supply of the Pleura
The nerve supply of the
1- visceral pleura is by autonomic fibers from
pulmonary plexus
2- the parietal layer is supplied by
a- intercostal nerves for the costal part
b- phrenic nerve for the mediastinal part &
diaphragmatic part of parietal pleura
c- the peripheral parts of diaphragmatic pleura
by intercostal.
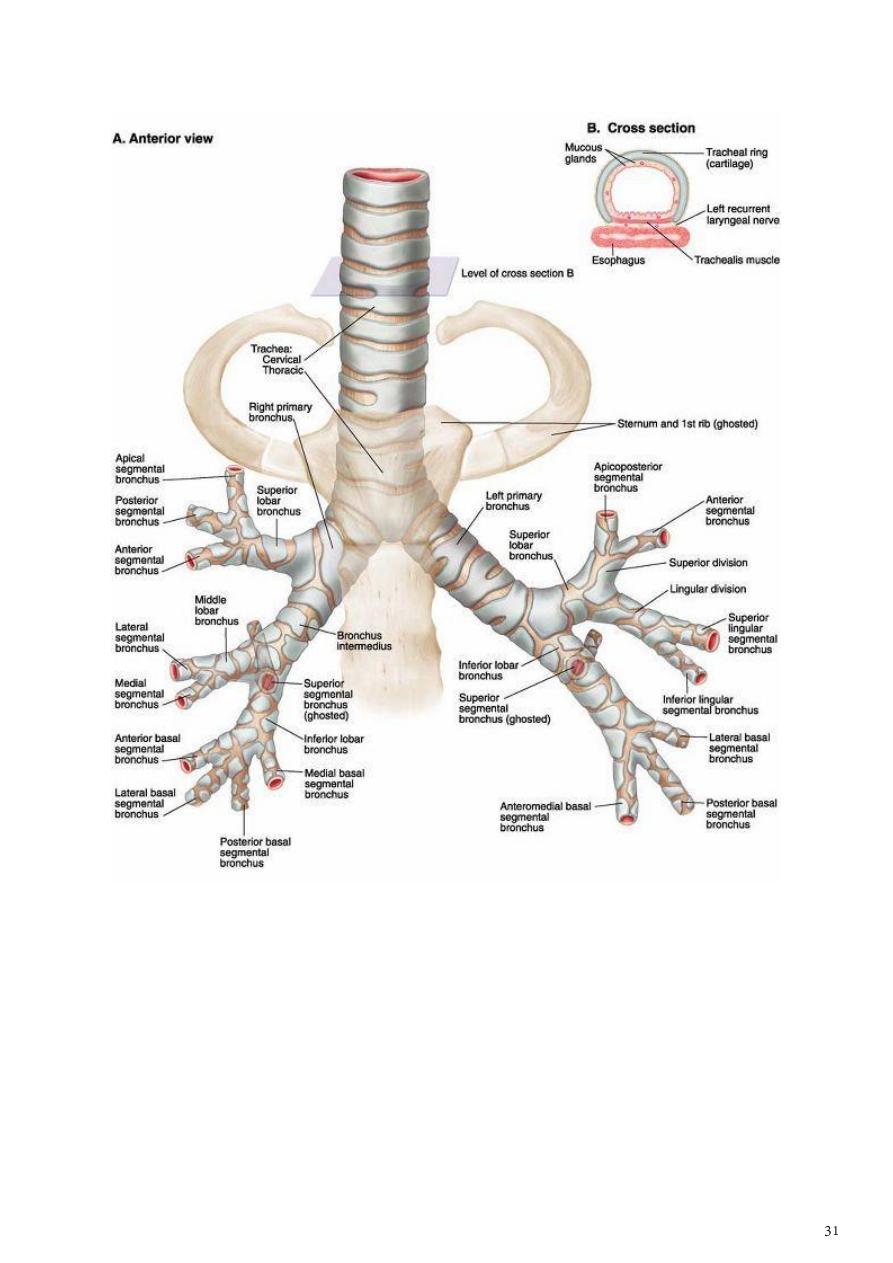
The Bronchi
1.
The trachea bifurcates behind the arch of the aorta into
the right and left principal (primary or main) bronchi
which divide giving rise to several million terminal
bronchioles that terminate in one or more respiratory
bronchioles.
2.
Each respiratory bronchiole divides into 2 to 11 alveolar
ducts that enter the alveolar sacs.
3.
The right principal main bronchus is wider, shorter, and
more vertical than the left and is about 1 inch (2.5 cm)
long.
A-
Before entering the hilum of the right lung, the principal bronchus gives off the
superior lobar bronchus or (eparterial bronchus).
B-
On entering the hilum, it divides into a middle and an inferior lobar bronchus.
4.
The left principal (main) bronchus is narrower, longer, and more horizontal than the
right and is about 2 inch (5 cm) long.
A-
It passes to the left below the arch of the aorta and in front of the esophagus.
B-
On entering the hilum of the left lung, the principal bronchus divides into a
superior and an inferior lobar bronchus.
Blood supply of bronchial tree
A- Two left bronchial arteries arise from the descending thoracic aorta
B- while there is only one Rt bronchial A. arising from the upper left bronchial A. or from
intercostal arteries.
Lymphatics of the bronchial tree: All drain to Bronchomediastinal lymph trunks which
drain:
1- on the Rt to the Rt lymph duct
2- on the Lt to the thoracic duct.
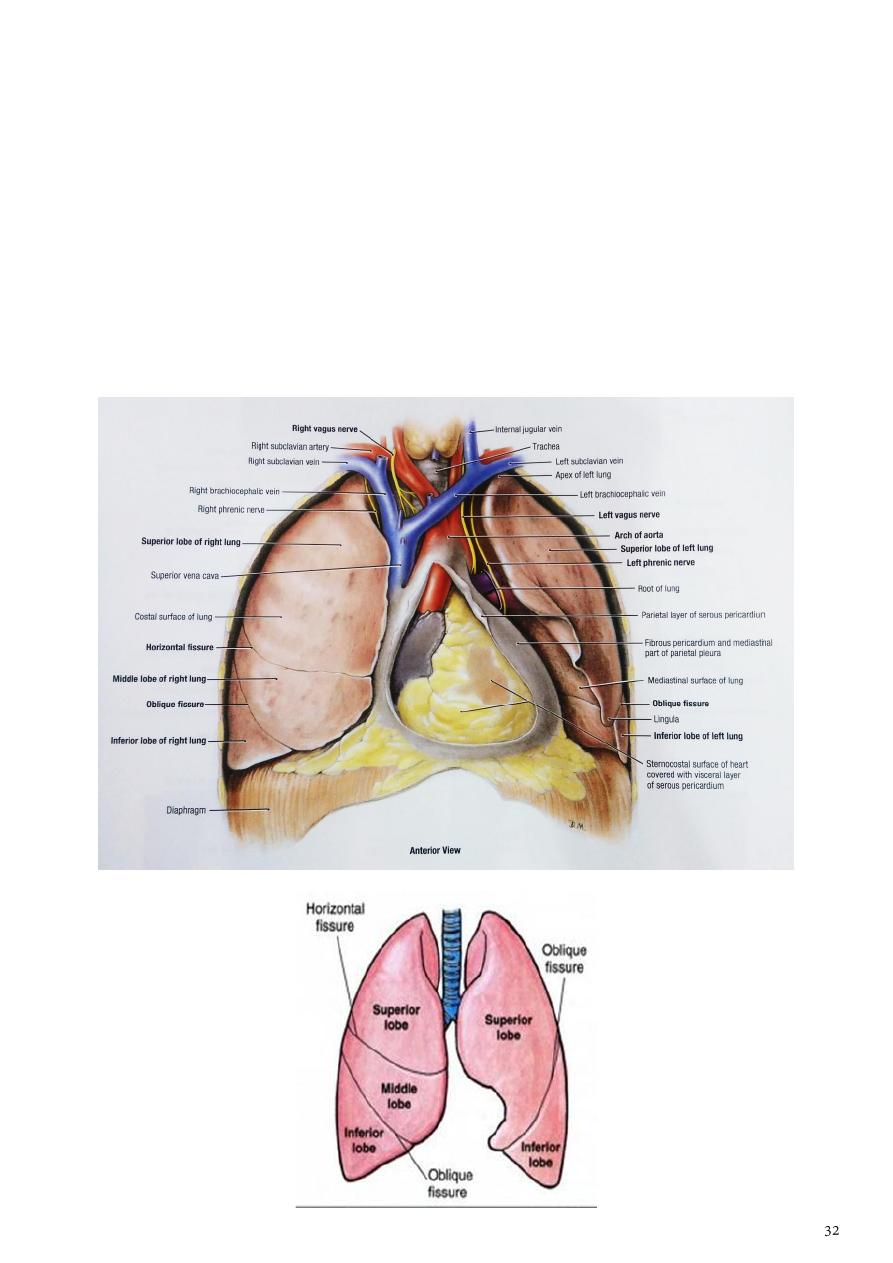
Lung
-
During life, the lungs are soft, spongy and very elastic.
-
In the child, they are pink, but with age, they become dark and mottled because of the
inhalation of dust particles.
-
The lung is conical in shape and has
a-
a blunt apex, which projects upward into the neck for about 1 inch (2.5 cm) above
the clavicle
b-
a concave base that sits on the diaphragm
c-
a convex costal surface, which corresponds to the concave chest wall
d-
and a concave mediastinal surface, which is molded to the pericardium and other
mediastinal structures.
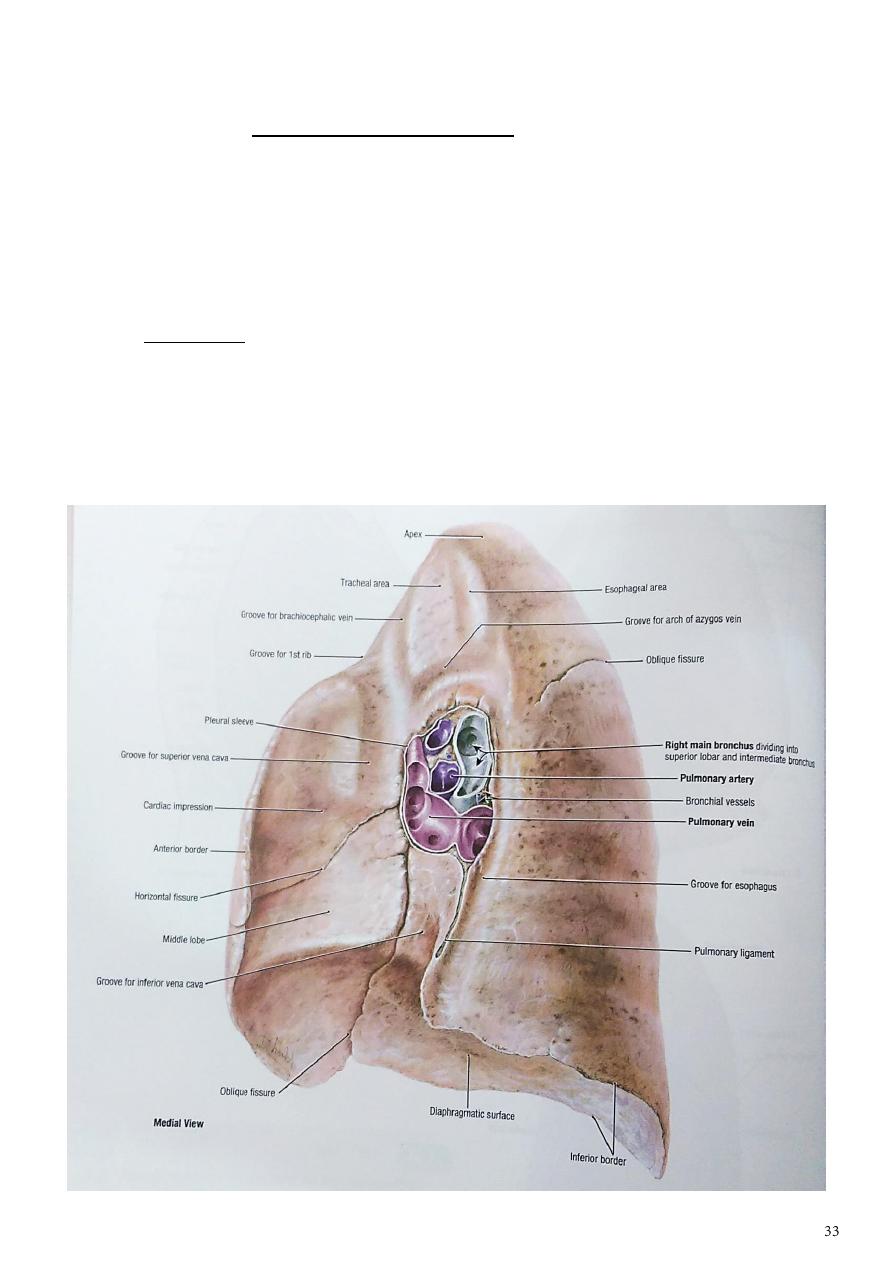
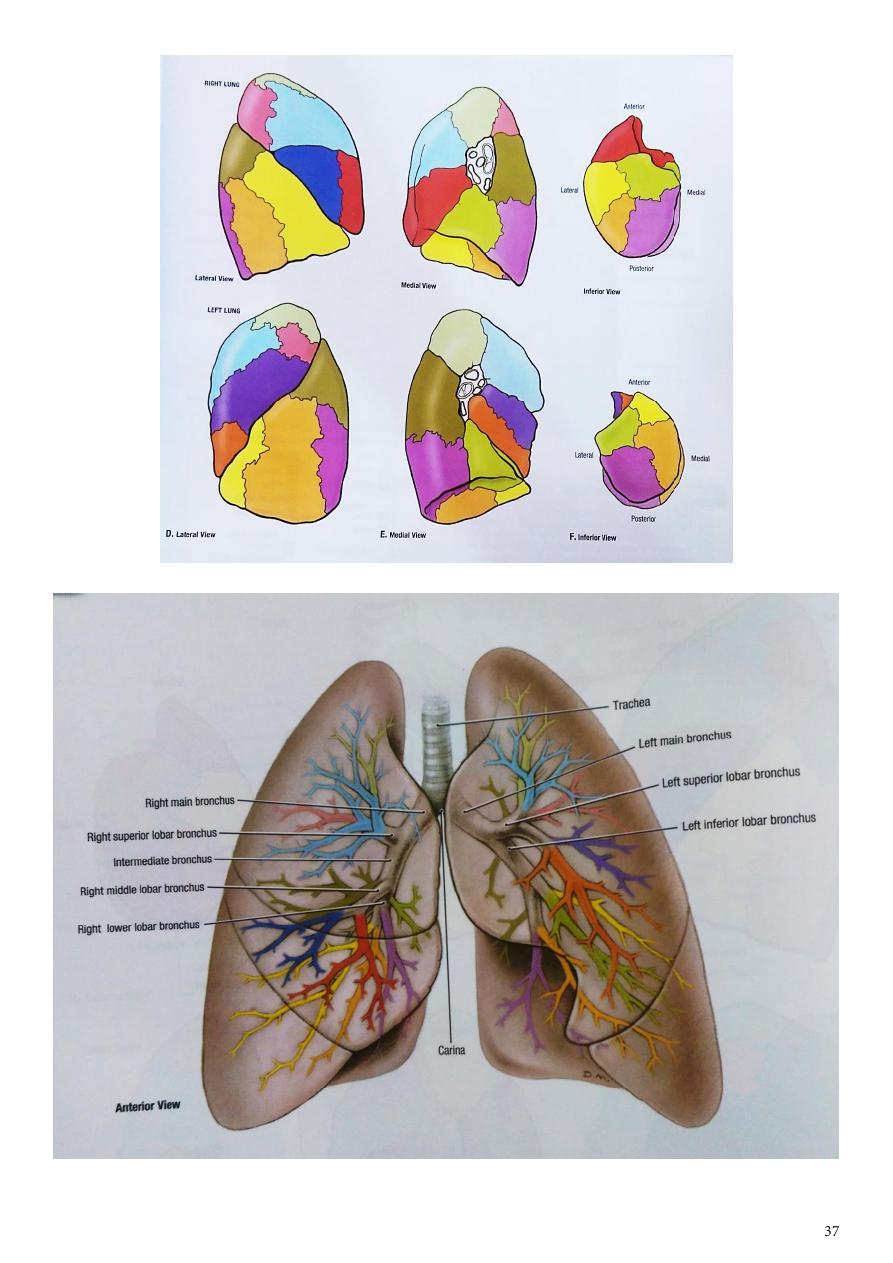
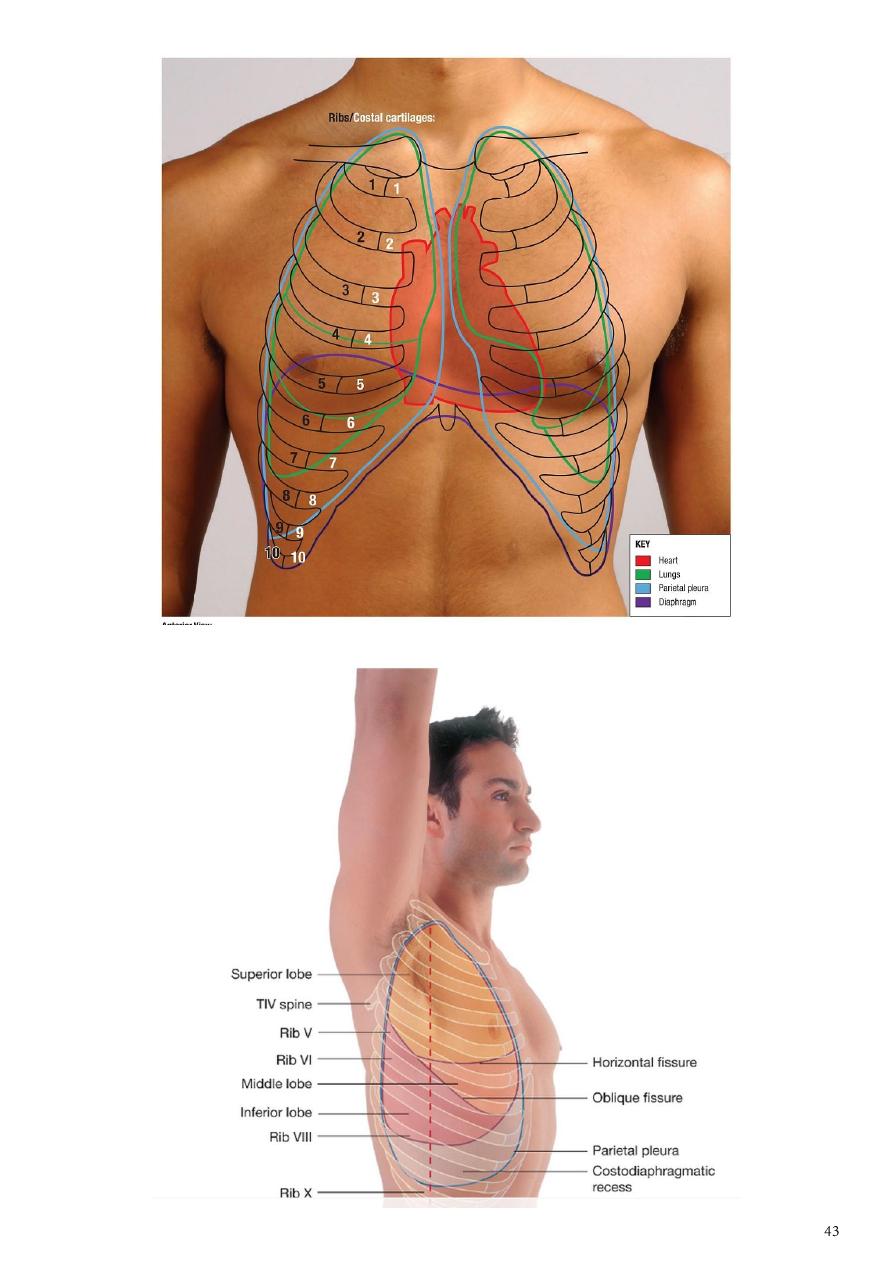
Right Lung
1- The right lung is slightly larger than the left
2- is divided by the oblique and horizontal fissures into three lobes: the upper, middle,
and lower lobes.
3- The oblique fissure runs from the inferior border upward and backward across the
medial and costal surfaces until it cuts the posterior border about 2.5 in. (6.25 cm)
below the apex.
4- The horizontal fissure runs horizontally across the costal surface at the level of the
4th cc to meet the oblique fissure in the midaxillary line.
5- The middle lobe is thus a small triangular lobe bounded by the horizontal and oblique
fissures.
6- Related to the root of right lung:
a-
the arch of a zygos vein above the lung root
b-
the azygos vein behind the lung root
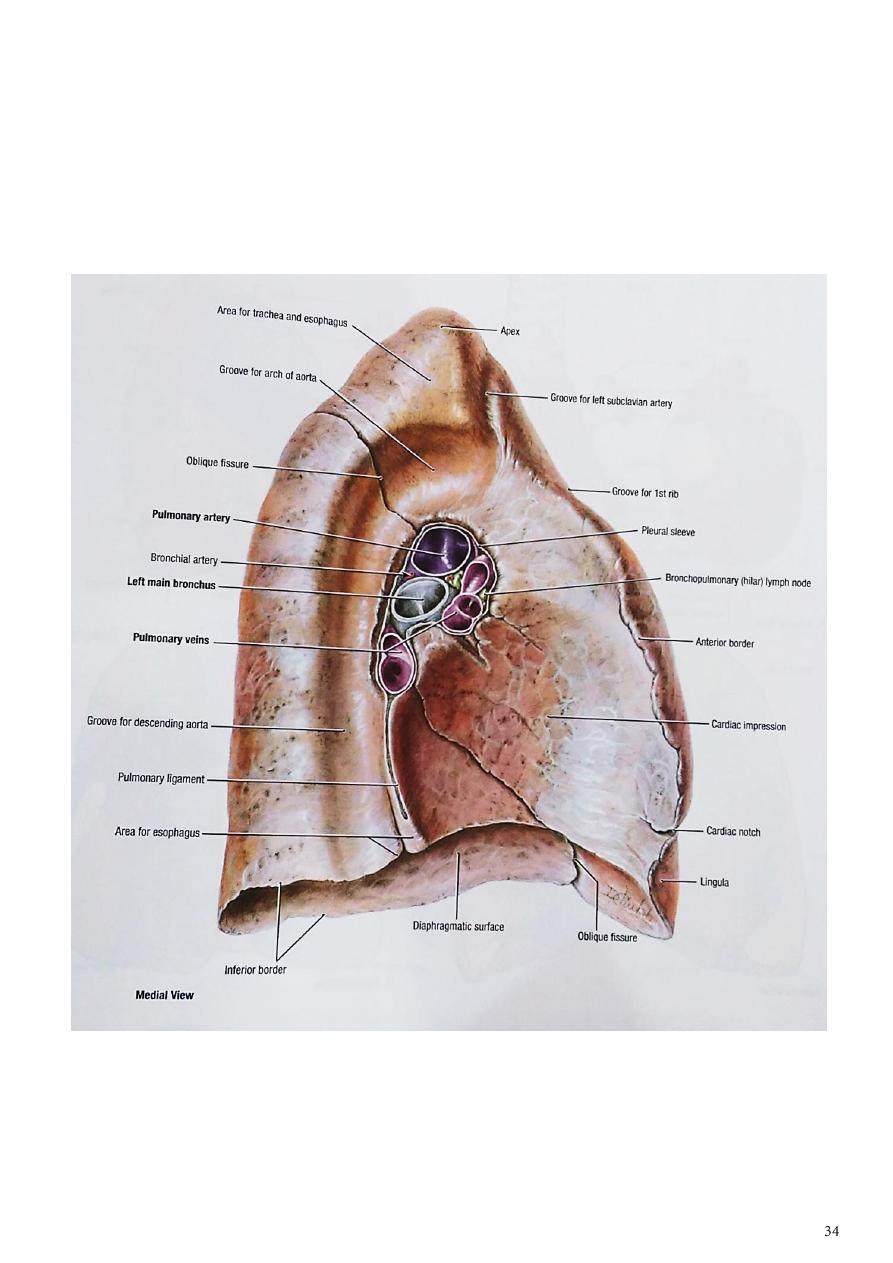
Left Lung
1- The left lung is divided by a similar oblique fissure into two lobes: the upper and
lower lobes.
2- There is no horizontal fissure in the left lung.
3- The root of left lung is related to
a-
the arch of aorta above the lung root
b-
descending thoracic aorta behind the lung root.

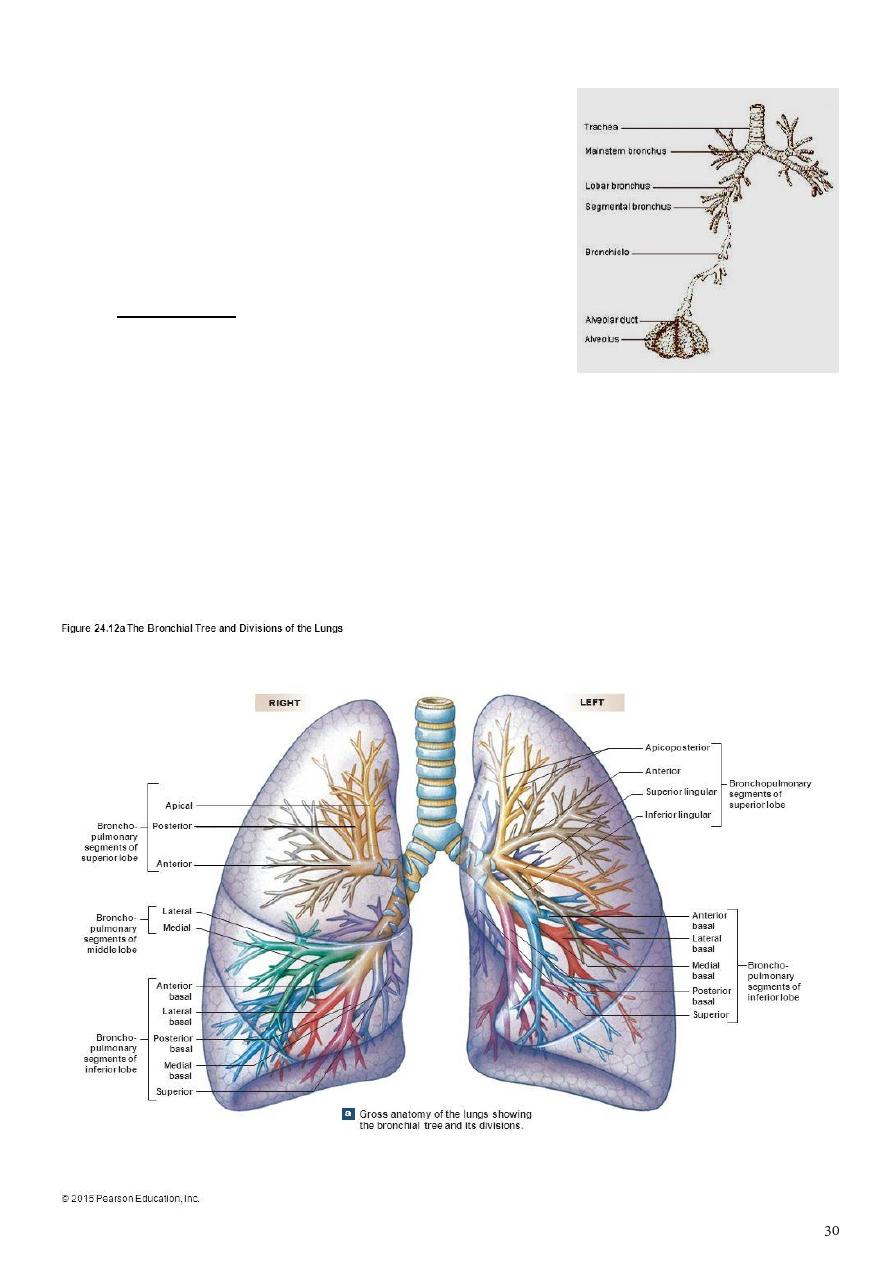
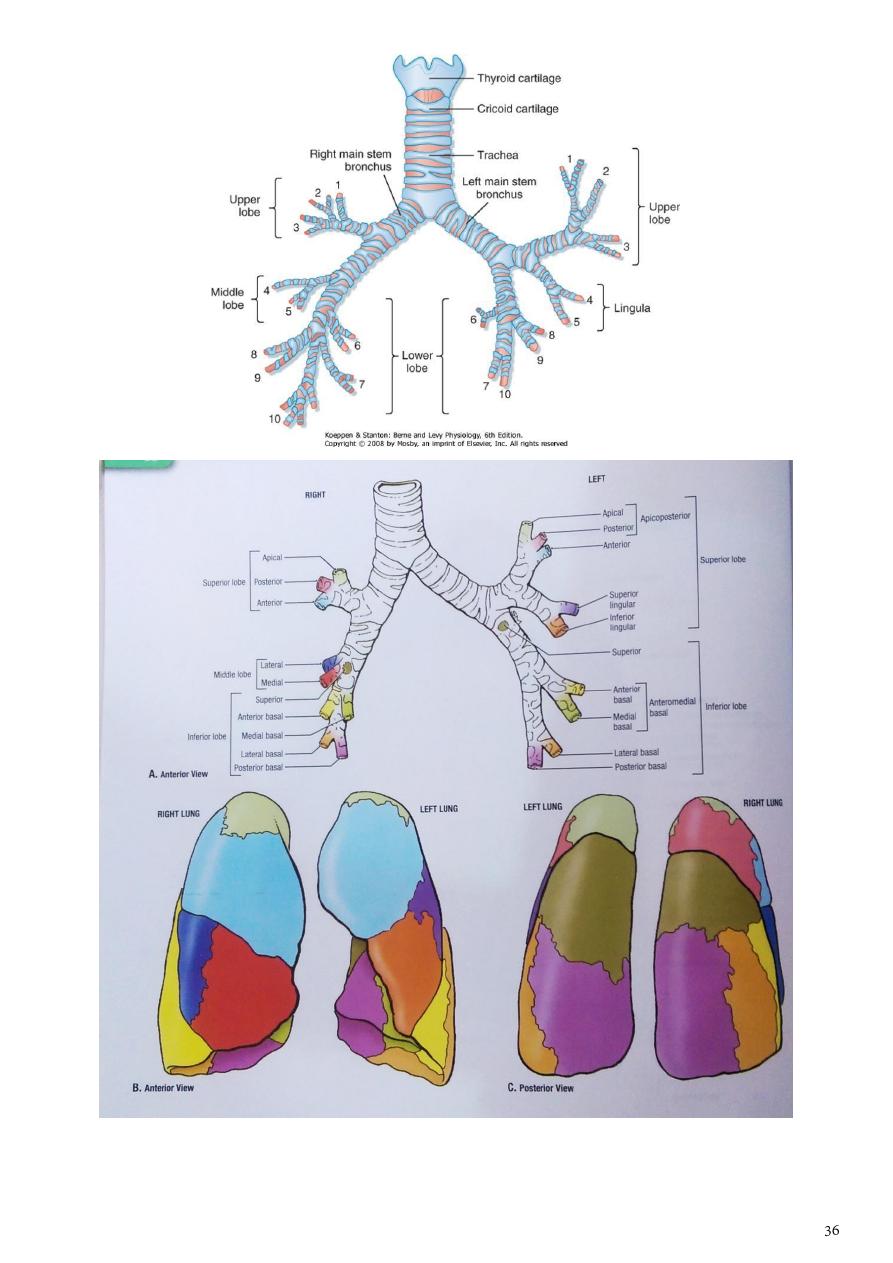
Bronchopulmonary Segments
The bronchopulmonary segments : are the anatomic, functional units of the lungs.
1- Each lobar (secondary) bronchus, which passes to a lobe of the lung, gives off
branches called segmental (tertiary) bronchi.
2- Each segmental bronchus passes to a structurally and functionally independent unit
of a lung lobe called a bronchopulmonary segment, which is surrounded by
connective tissue.
3- The segmental bronchus is accompanied by a branch of the pulmonary artery, but
the tributaries of the pulmonary veins run in the connective tissue between adjacent
bronchopulmonary segments.
4- Each segment has its own lymphatic vessels and autonomic nerve supply.
A- On entering a bronchopulmonary segment, each segmental bronchus divides
repeatedly& become smaller,
B- The smallest bronchi divide and give rise to bronchioles, which are <1 mm in
diameter & with no cartilage in their walls.
C- The bronchioles then divide and give rise to terminal bronchioles which show
delicate outpouchings from their walls named respiratory bronchiole.
D- The respiratory bronchioles end by branching into alveolar ducts, which lead into
tubular passages with numerous thin-walled sacs called alveolar sacs which consist
of several alveoli (sites of gaseous exchange).
The main bronchopulmonary segments are as follows:
Right lung has the following B-P segments:
Superior lobe: Apical, posterior, anterior
Middle lobe: Lateral, medial
Inferior lobe: Superior (apical), medial basal, anterior basal, lateral basal, posterior basal.
Left lung has the following B-P segments:
Superior lobe: Apical, posterior, anterior, superior lingular, inferior lingular.
Inferior lobe: Superior (apical), medial basal, anterior basal, lateral basal, posterior basal.
The root of the lung is formed of structures that are entering or leaving the lung. It is made
up of the bronchi, pulmonary artery and veins, lymph vessels, bronchial vessels, and nerves.
The root is surrounded by a tubular sheath of pleura, which joins the mediastinal parietal
pleura to the visceral pleura covering the lungs.
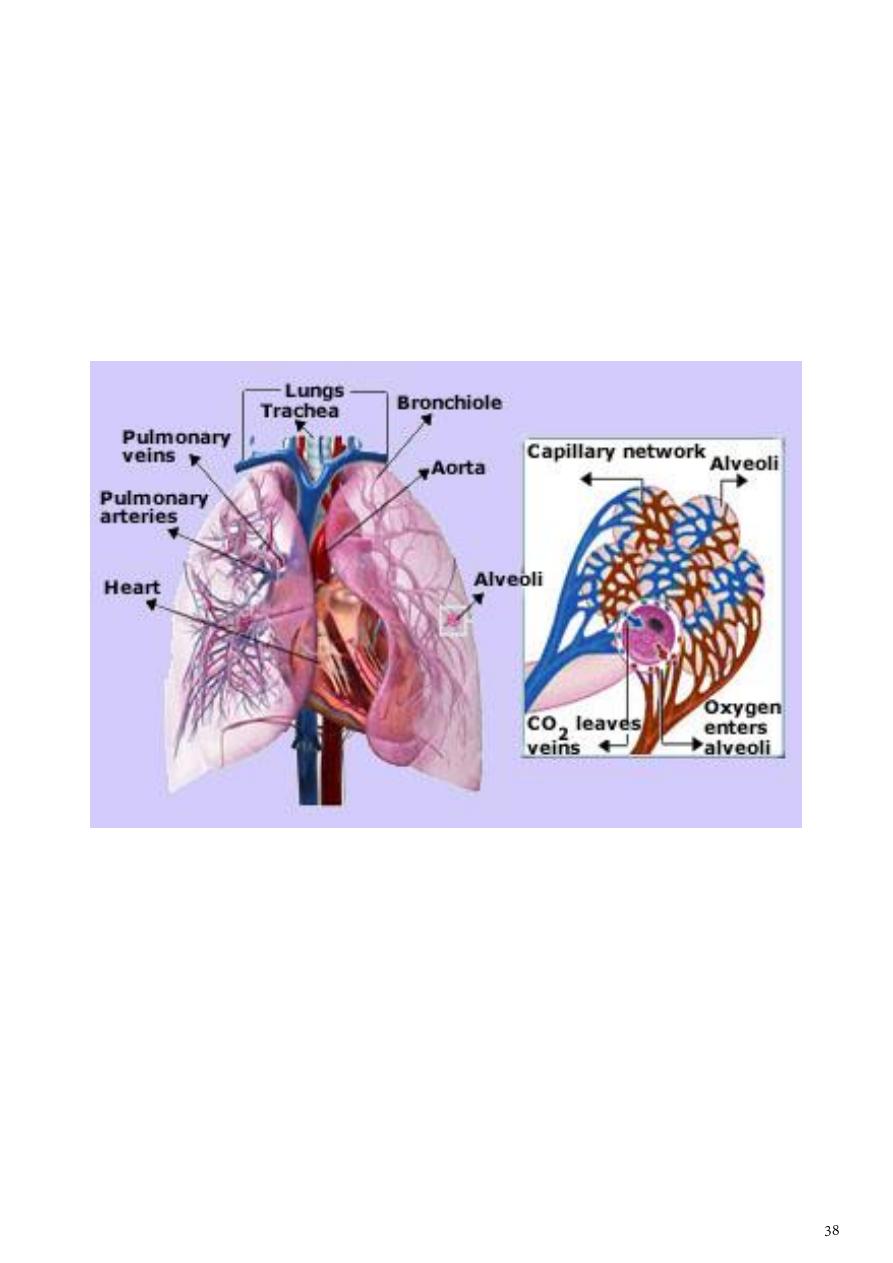
Blood Supply of the Lungs
Bronchial arteries, which are branches of the descending aorta.
The bronchial veins (which communicate with the pulmonary veins) drain into the azygos
and hemiazygos veins.
Note: The alveoli receive deoxygenated blood from the terminal branches of the pulmonary
arteries.
The oxygenated blood leaving the alveolar capillaries drains into the tributaries of the
pulmonary veins, which follow the intersegmental connective tissue septa to the lung root.
Two pulmonary veins leave each lung root to empty into the left atrium of the heart.
Lymph Drainage of the Lungs
1- The superficial (subpleural) plexus lies beneath the visceral pleura and drains over
the surface of the lung toward the hilum, where the lymph vessels enter the
bronchopulmonary nodes.
2- The deep plexus travels along the bronchi and pulmonary vessels passing through
pulmonary nodes located within the lung substance toward the hilum of the lung,
the lymph then enters the bronchopulmonary nodes in the hilum of the lung.
All the lymph from the lung leaves the hilum and drains into the tracheobronchial nodes
and then into the bronchomediastinal lymph trunks.
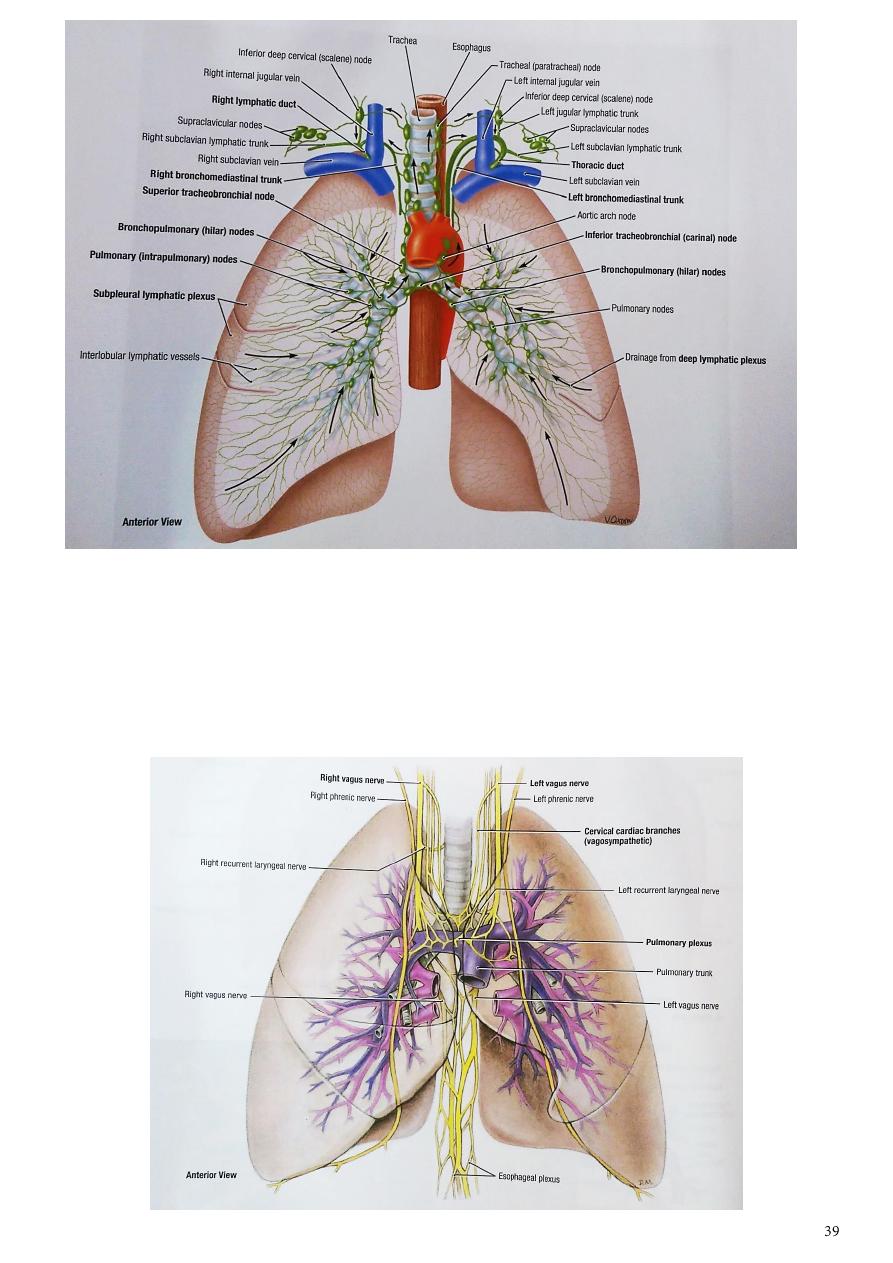
Nerve Supply of the Lungs
Nerves supply are from the pulmonary plexuses( Anterior & posterior) containing fibers
from both sympathetic & parasympathetic .The sympathetic causes bronchodilatation &
vasoconstriction
while the parasympathetic components causes Bronchoconstriction & Vasodilatation in
addition it increases the glandular secretion.
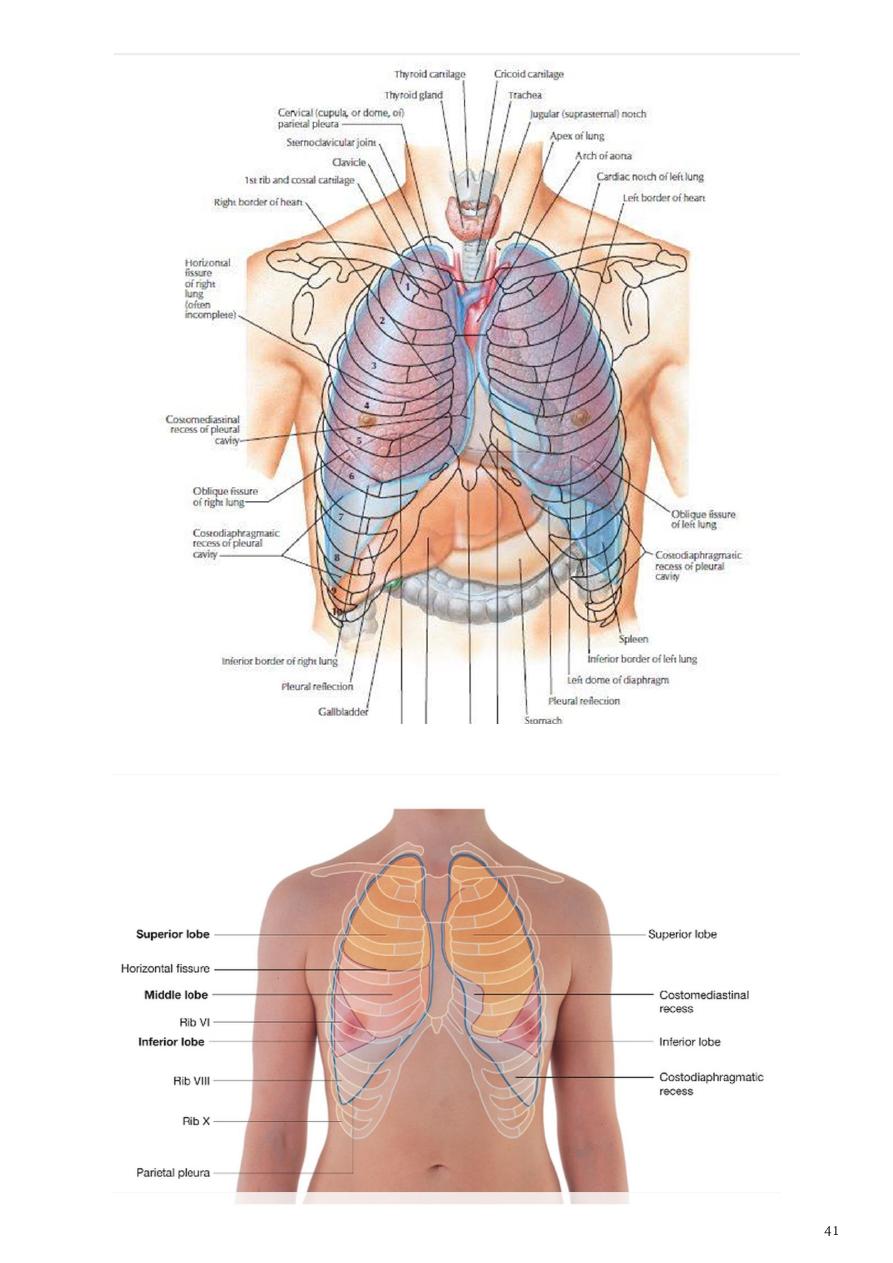
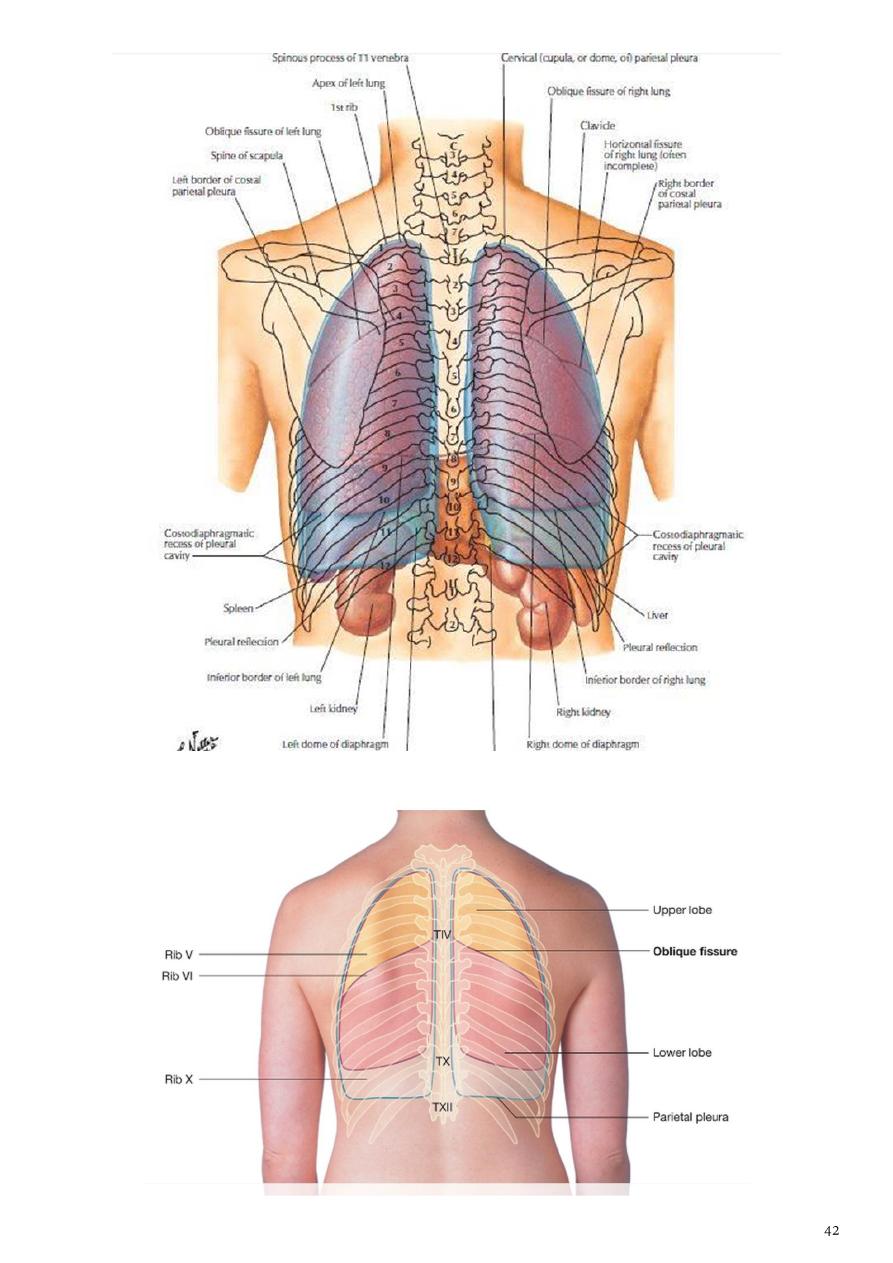
Surface marking of pleurae:
1- The cervical part of parietal pleura (Dome of pleura)
a- project through the inlet of thorax to the root of the neck (just like the apex of the
lung)
b- is being separated from the structures at the root of the neck by suprapleural
membrane which intervenes between these structures & the dome of the pleura.
It starts from sternoclavicular joint to appoint about 1 inch (2.5 cm) above the
junction between the medial & intermediate thirds of the clavicle.
2- The anterior border of parietal pleura( on Right side ) extends anteriorly & down
wards from the Right sternoclavicular joint to the level of the sternal angle and then
continues down ward to the level of Xiphisternal joint.
3- While on the left side the anterior border descends downward too till the level of the
4th costal cartilage, then deviates laterally along the lateral margin of the sternum to
reach the level of the cardiac notch. It then descends sharply to reach the level of 6th
costal cartilage.
4- The inferior border of the parietal pleura will passes downward and laterally from
Xiphisternal joint crossing the 8th Rib at the midclavicular line, the 10th Rib at
midaxillary line & the 12th Rib adjacent to the vertebral column
5- the posterior border of the parietal pleura extends from the back of the Dme of
pleura above to end just below the neck of the last rib where it meets the terminal
end of the line representing the anterior border of the pleura.
The lungs has the same surface markings as that of parietal pleura except that the inferior
border of the lung is 2 vertebral level of the pleura .Thus inferior border of the lung crosses
the 6th Rib at midclavicular line, the 8th rib at midaxillary line & 10th Rib adjacent to the
vertebral column.
-
The space between the inferior border of the lung & the parietal pleura represents the
COSTODIAPHRAGMATIC pleural recess which the lung is going to occupy it completely
only in deep inspiration as in cases of a cute attacks of Asthma.
-
The Pleural recess are in fact a gap or small spaces forms due to reflection of one part of
parietal pleura against another part and normally these recesses are not occupied by
lung tissues and there are 3 recess :
1- Costodiaphragmatic due to reflection of costal against diaphragmatic parts of the
parietal pleura.
2- Costomediastinal due to reflection of costal against the mediastinal part of the parietal
pleura.
3- Mediastinodiaphragmatic forms due to reflection of the mediastinal against the
diaphragmatic part of parietal pleura (this recess is not important and is the smallest
one among the 3 recesses).

Part4
: The heart
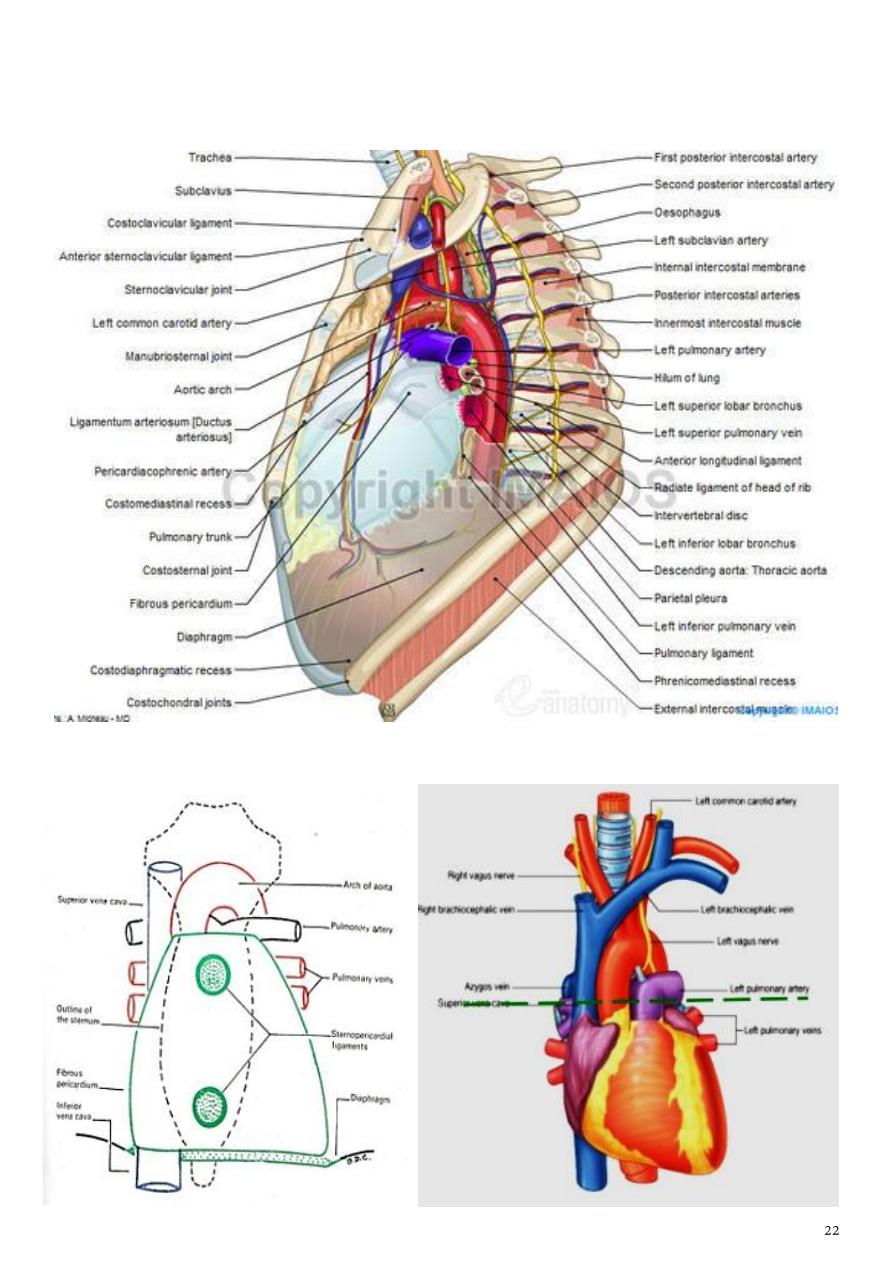
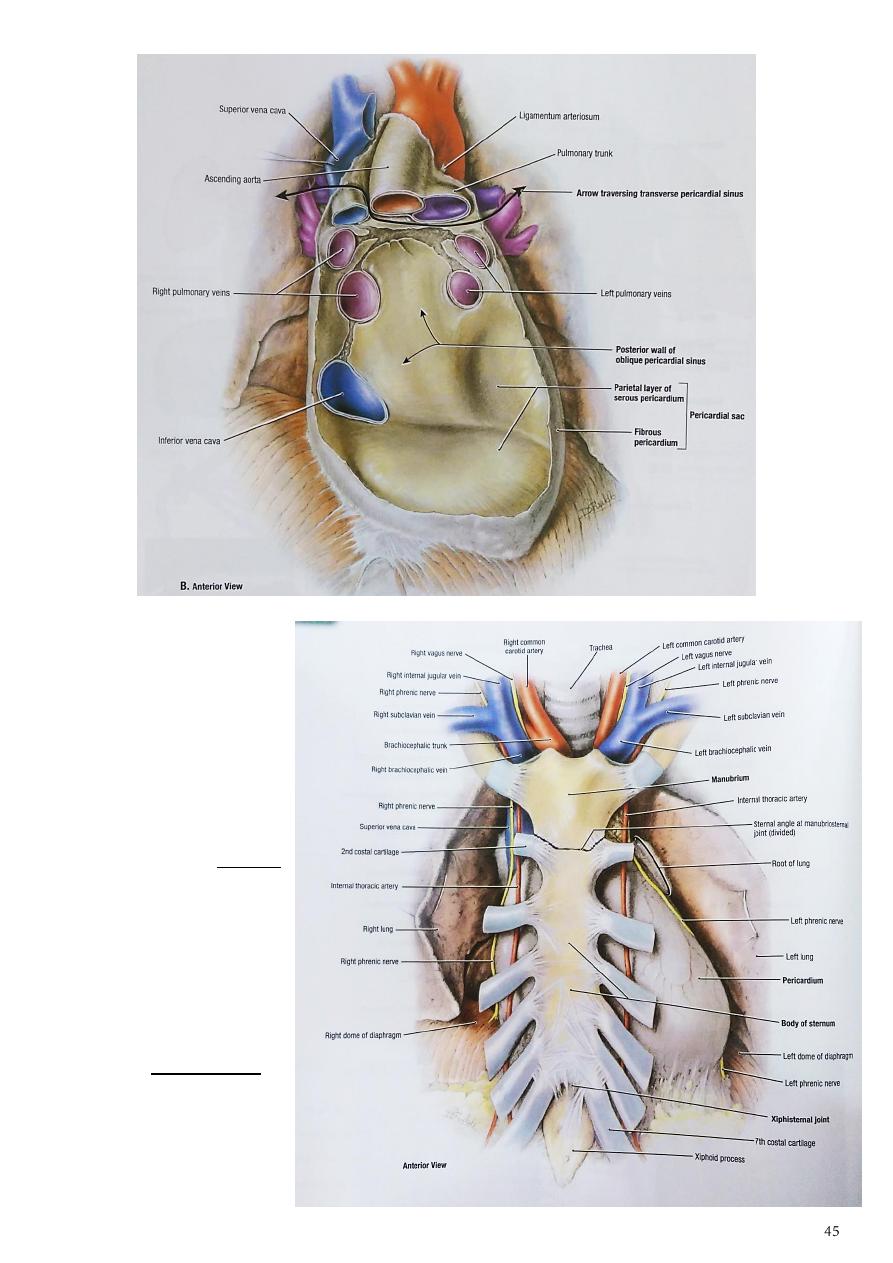
Pericardium
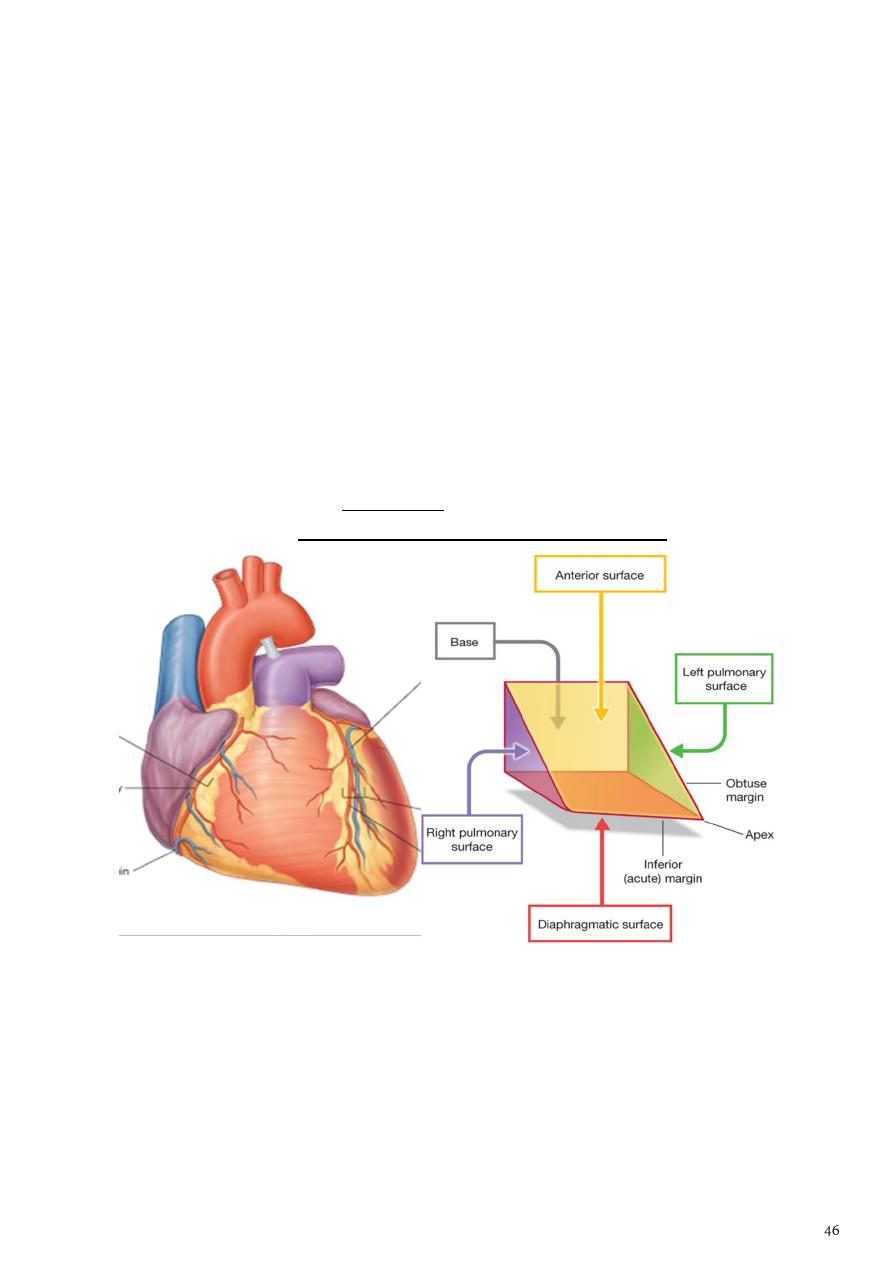
The pericardium : is a fibroserous sac that encloses the heart and the roots of the great
vessels lies within the middle mediastinum posterior to the body of the sternum and the
2nd to the 6th costal cartilages.
Fibrous Pericardium
The fibrous pericardium :
1- is the strong fibrous part of the sac.
2- It is firmly attached below to the central tendon of the diaphragm & in front to the
sternum by the sternopericardial ligaments.
3- It fuses with the outer coats of the great blood vessels: the aorta, the pulmonary
trunk, the superior and inferior venae cavae, and the pulmonary veins.
Serous Pericardium
The serous pericardium:
1- lines the fibrous pericardium and coats the heart.
2- It is divided into parietal and visceral layers.
a- The parietal layer lines the fibrous pericardium and is reflected around the roots of the
great vessels to become continuous with the visceral layer of serous pericardium that
closely covers the heart.
b- The visceral layer is closely applied to the heart and is often called the epicardium.
The slitlike space between the parietal and visceral layers is referred to as the pericardial
cavity. Normally, the cavity contains a small amount of tissue fluid (about 50 mL), the
pericardial fluid, which acts as a lubricant to facilitate movements of the heart.
Pericardial Sinuses
1- On the posterior surface of the heart, the
reflection of the serous pericardium around
the large veins (four pulmonary veins and the
superior and inferior venae cavae) forms a
recess called the oblique sinus.
2- The transverse sinus, which is a short passage
that lies between the reflection of serous
pericardium around the aorta and pulmonary
trunk and the reflection around the large
veins.
Nerve Supply of the
Pericardium
1- The fibrous
pericardium and the
parietal layer of the
serous pericardium are
supplied by the phrenic
nerves.
2- The visceral layer of
the serous pericardium
is innervated by
branches of the
sympathetic trunks
and the vagus nerves.
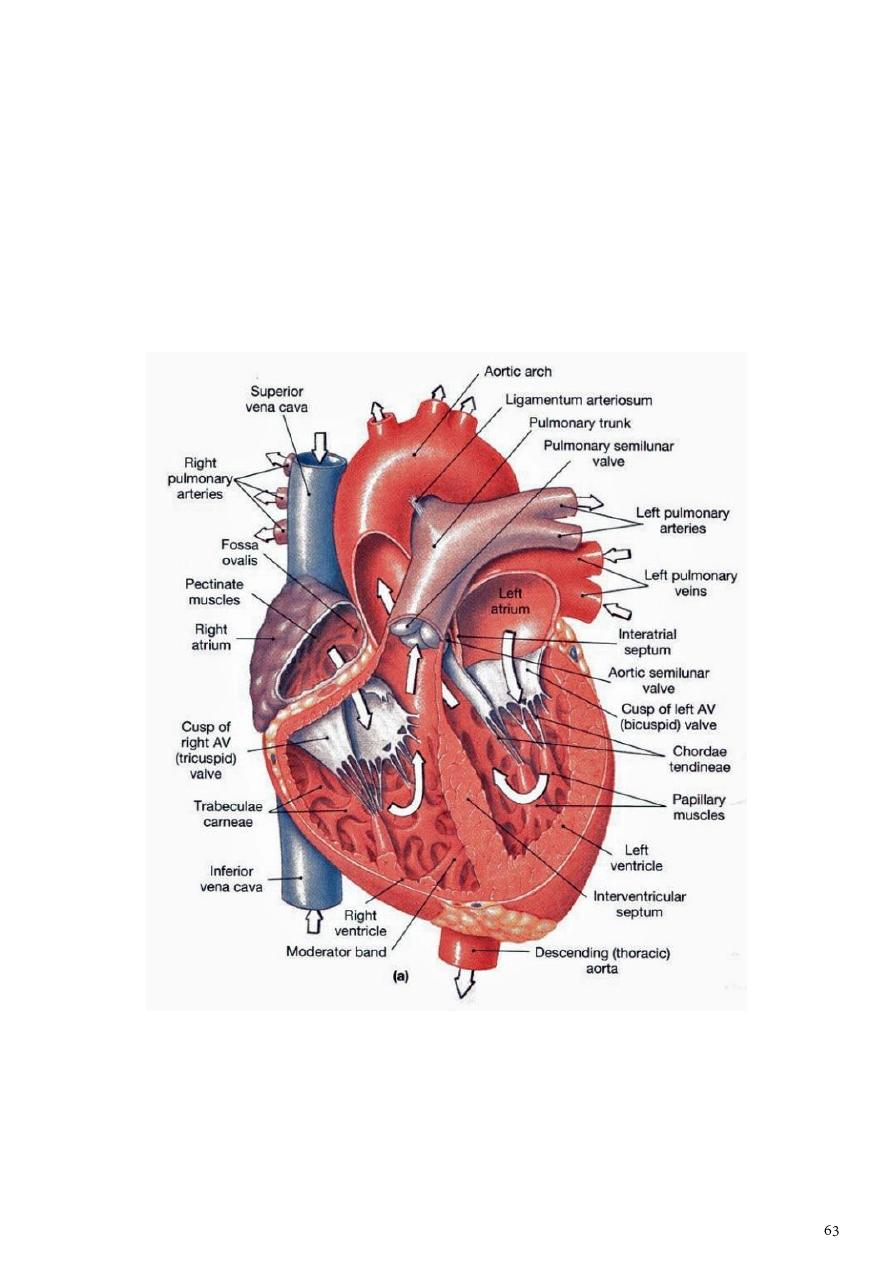
Heart
The heart : is a hollow muscular organ that is somewhat pyramid shaped and lies within the
pericardium in the mediastinum.
Surfaces of the Heart :
The heart has three surfaces:
1- sternocostal (anterior): is formed mainly by the right atrium and the right ventricle,
which are separated from each other by the atrioventricular groove
2- Diaphragmatic (inferior): is formed mainly by the right and left ventricles.
3- The base (posterior): is formed mainly by the left atrium
The apex of the heart, formed by the left ventricle, is directed downward, forward, and to
the left. It lies at the level of the fifth left intercostal space, (9 cm) from the midline. In the
region of the apex, the apex beat can usually be seen and palpated in the living person.
Borders of the heart:
The right border is formed by the right atrium.
The left border is formed by the left ventricle and part of the left auricle.
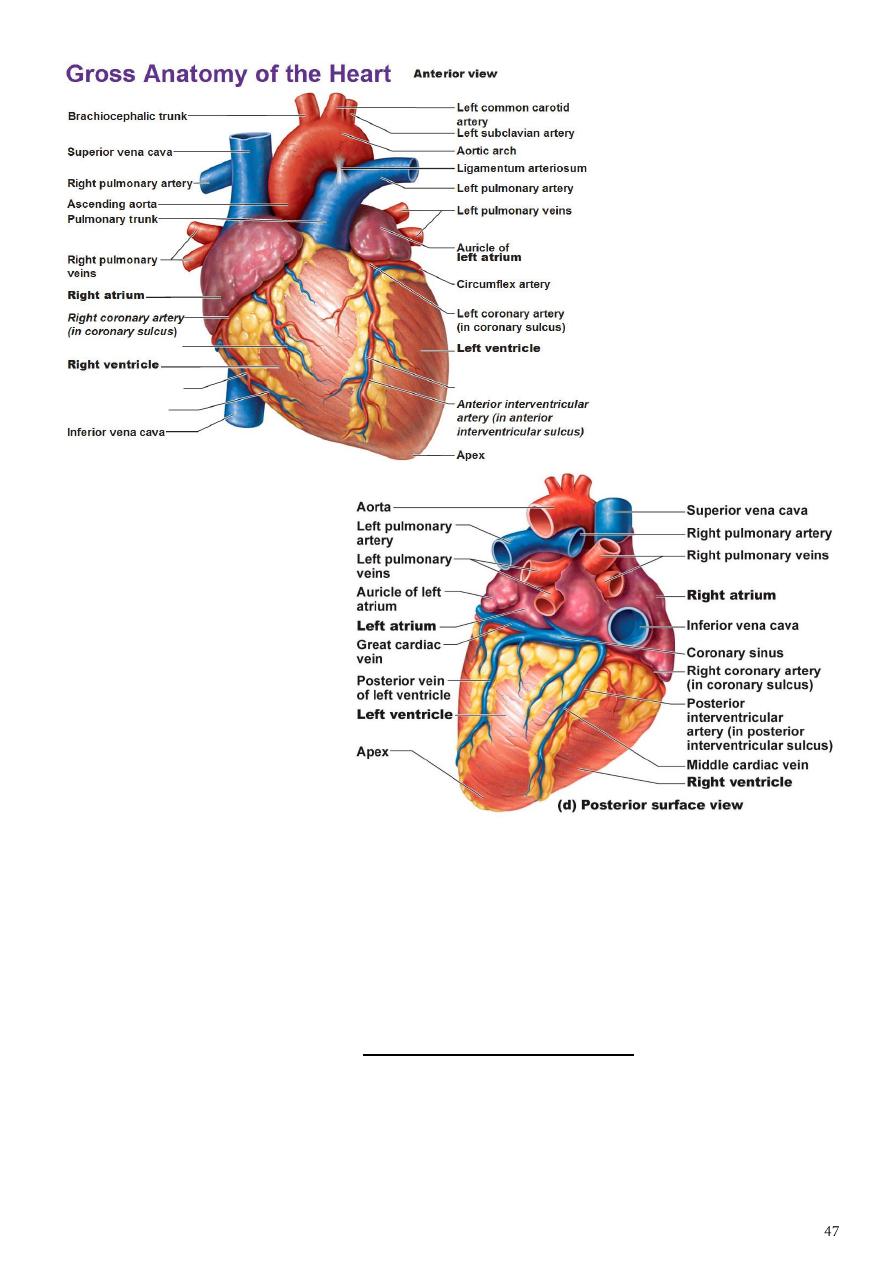
Chambers of the Heart
-
The heart is divided into four chambers: the right and left atria and the right and left
ventricles.
-
The 2 atria are separated from the 2 ventricles by Atrioventricular groove (Coronary
sulcus).
-
The 2 ventricles separated by anterior interventricular groove contains the great
cardiac vein & anterior interventricular artery.
-
The walls of the heart are composed of
1- cardiac muscle ,the myocardium
2- covered externally with serous pericardium, the epicardium
3- and endocardium which lined internally with a layer of endothelium.
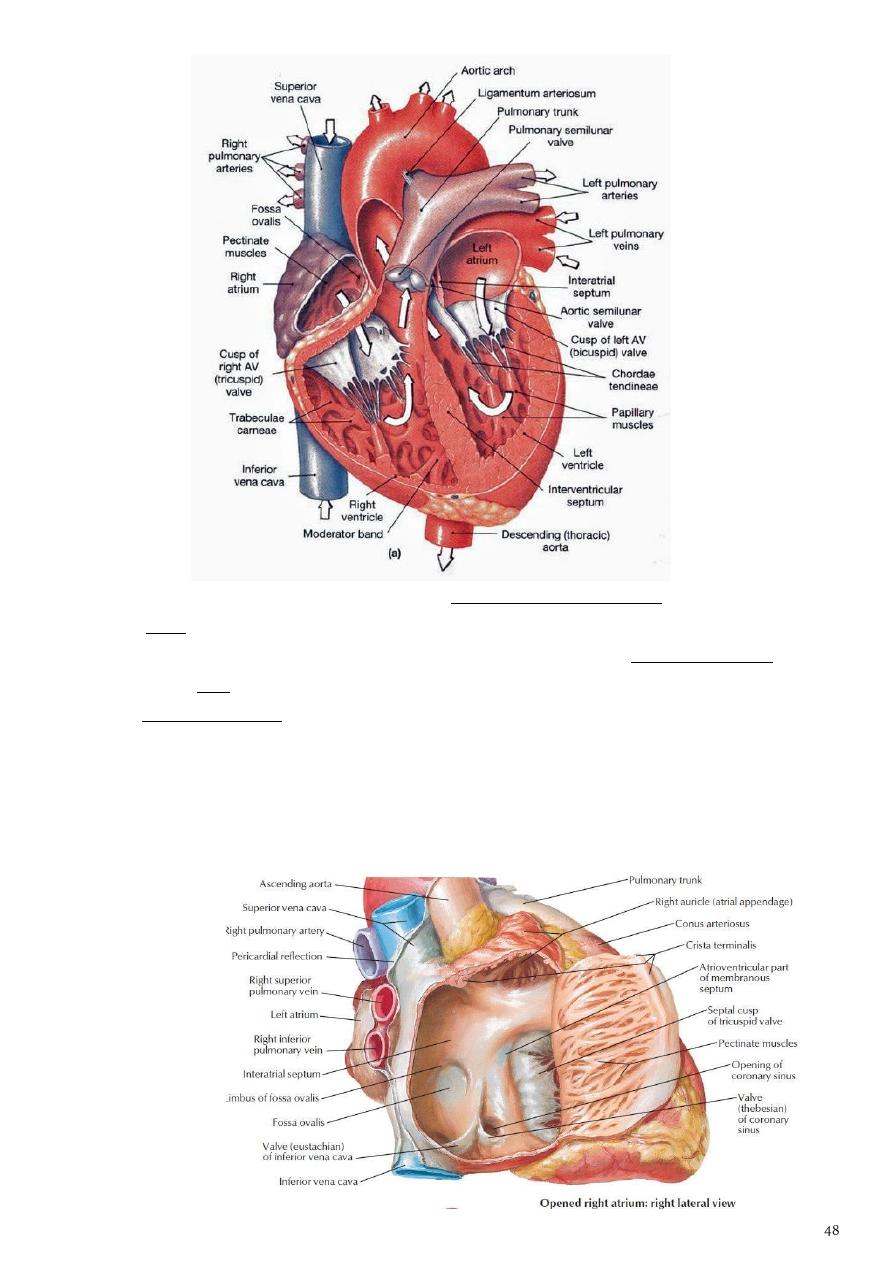
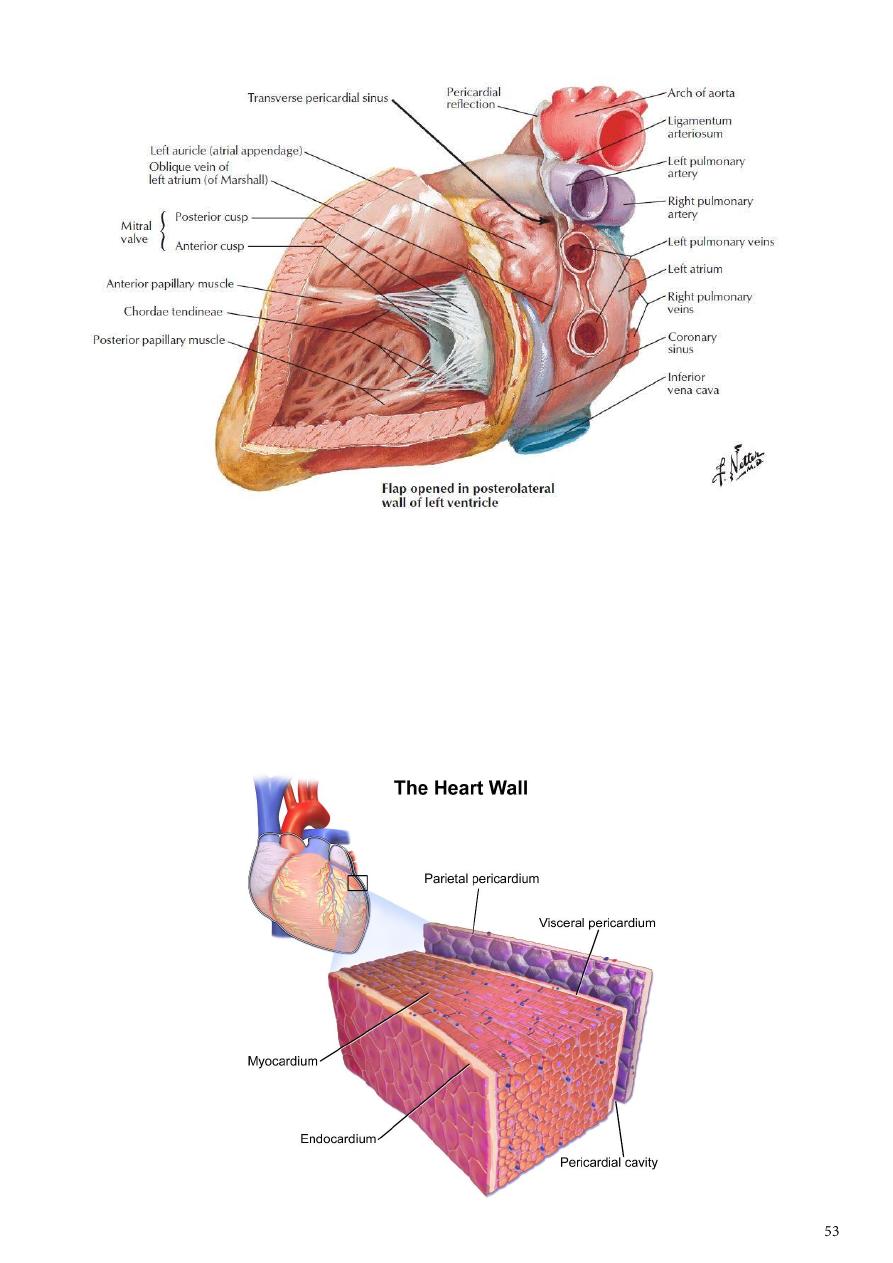
Each Atria leads to its corresponding ventricle by Atrioventricular Valve
a- the right one is Tricuspid consists of 3 cusps connected to 3 papillary muscles on the
inside of the right ventricle via thread like structur known as Chorda tendinae,
b- while the left valve is Bicuspid (Mitral ) has 2 cusps connected to 2 papillary muscles
via chorda tendinae.
-
The R.A consists of 2 part
1- a smooth (sinus venosus)
2- rough part ( Musculae pectinatae) separated by Crista terminalis.
It receives the openings of superior vena cava (from above), inferior vena cava ( from
below) and
opening of the
coronary venous
sinus..
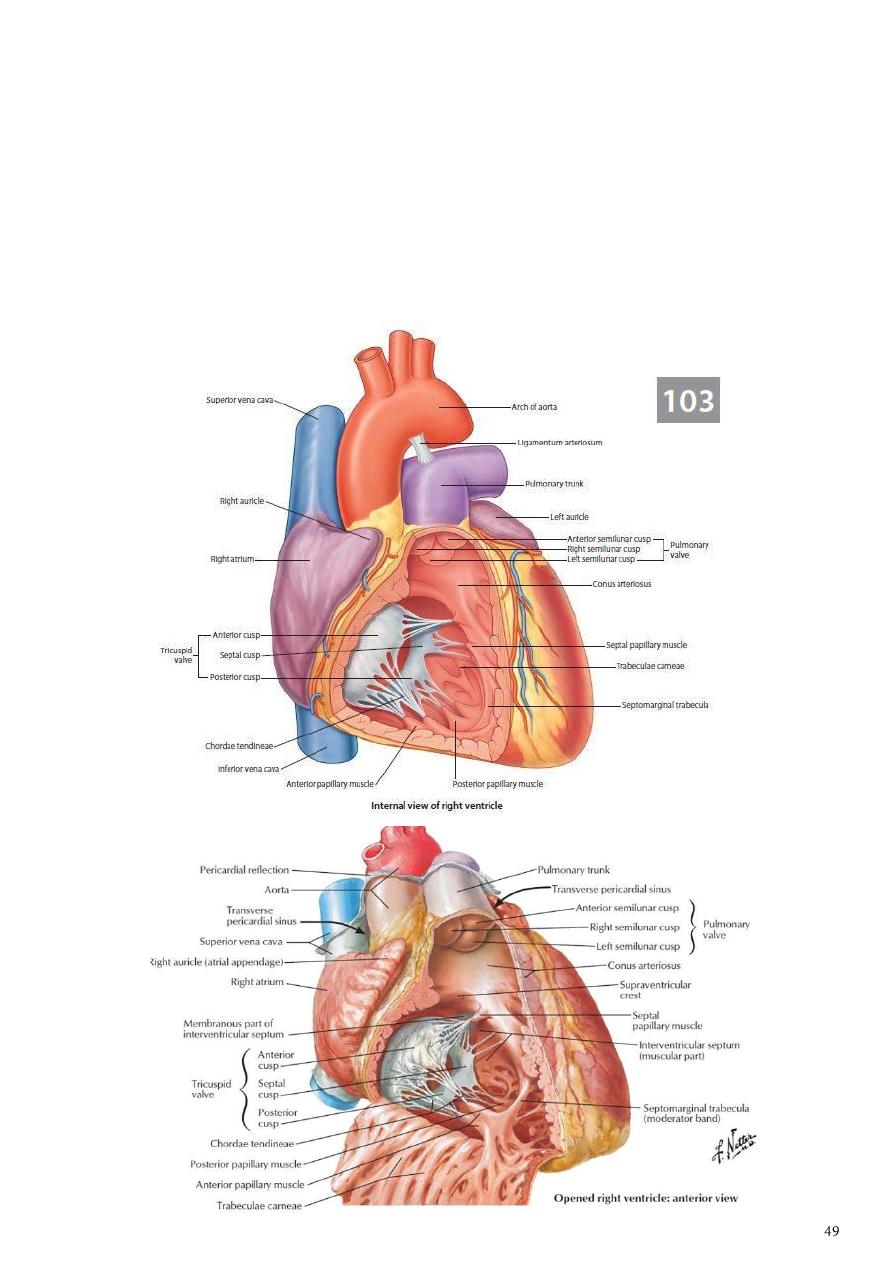
Right Ventricle
1- The walls of the right ventricle are much thicker than those of the right atrium and
show several internal projecting ridges formed of muscle bundles known as
trabeculae carneae.
2- The papillary muscles, are attached by their bases to the ventricular wall, their apices
are connected by fibrous chords (the chordae tendineae) to the cusps of the tricuspid
valve.
3- The moderator band, crosses the ventricular cavity from the septal to the anterior
wall. It conveys the right branch of the atrioventricular bundle.
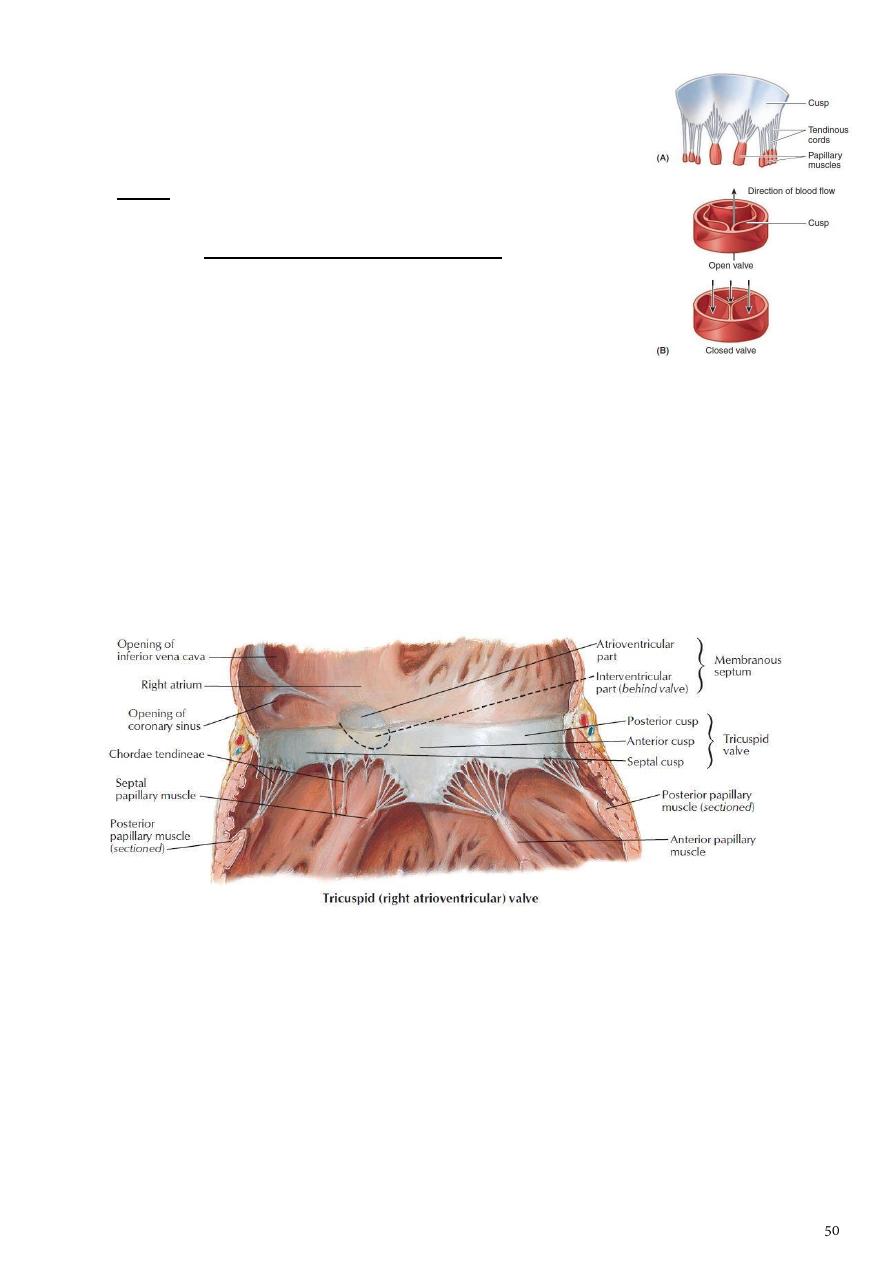
The tricuspid valve
1- guards the right atrioventricular orifice consists of three cusps
formed by a fold of endocardium with some connective tissue
enclosed: anterior, septal, and posterior cusps.
2- The bases of the cusps are attached to the fibrous ring of the
skeleton of the heart,
3- whereas their free edges and ventricular surfaces are attached
to the chordae tendineae.
4- The chordae tendineae connect the cusps to the papillary
muscles.
a- When the ventricle contracts, the papillary muscles contract
and prevent the cusps from being forced into the atrium and turning inside out as the
intraventricular pressure rises.
b- To assist in this process, the chordae tendineae of one papillary muscle are
connected to the adjacent parts of two cusps.
-
The right ventricle pumps the deoxygenated blood to the pulmonary trunk via the
pulmonary valve to reach the lungs for exchange of gasses ( Minor circuit)
-
while the L.V pumps the oxygenated blood to the Aorta via Aortic valve to be distributed
to different parts of the body as Systemic circulation
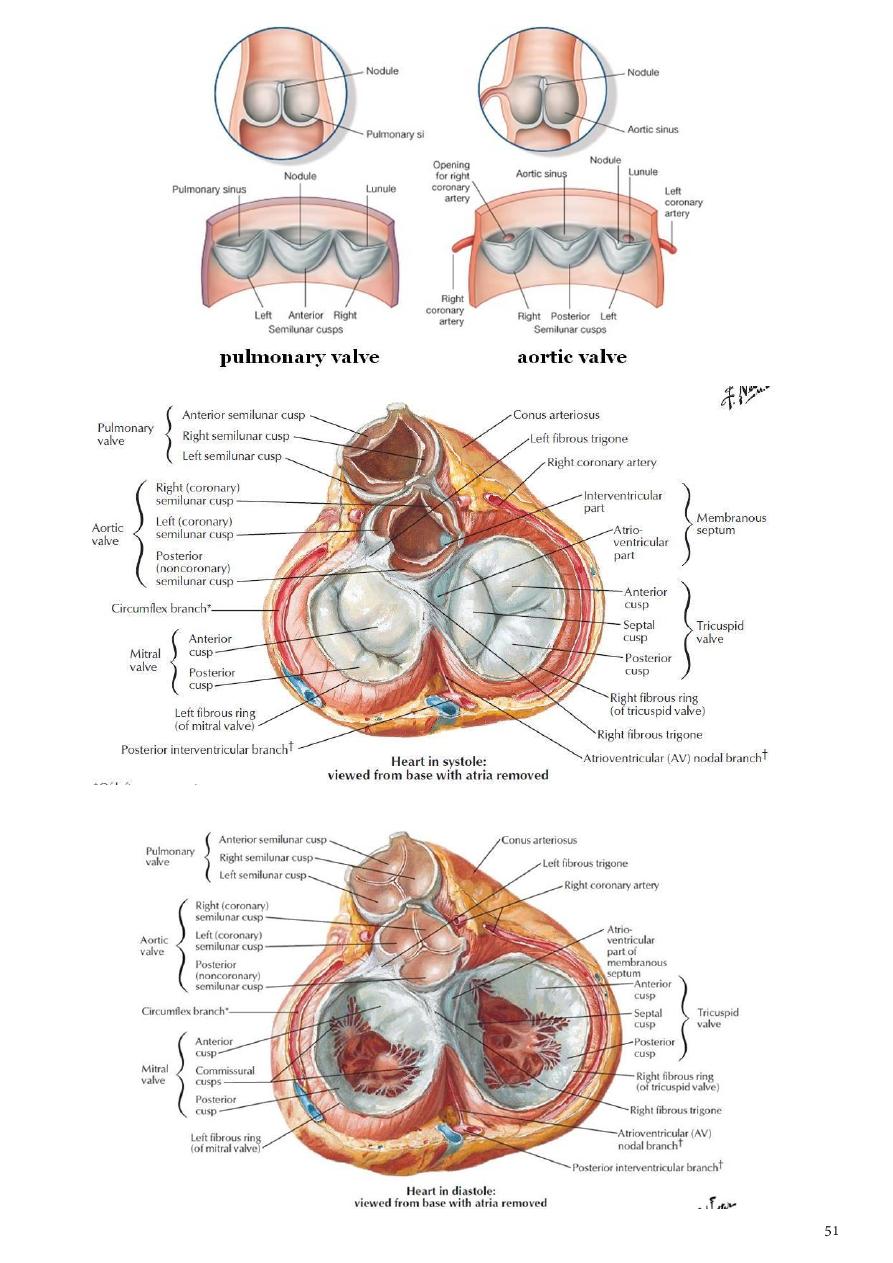
The pulmonary valve
1- guards the pulmonary orifice and consists of threesemilunar cusps formed by folds of
endocardium with connective tissue.
2- No chordae or papillary muscles are associated with these valve cusps; the attachments
of the sides of the cusps to the arterial wall prevent the cusps from prolapsing into the
ventricle.
3- At the root of the pulmonary trunk are three dilatations called the sinuses, and one is
situated external to each cusp.
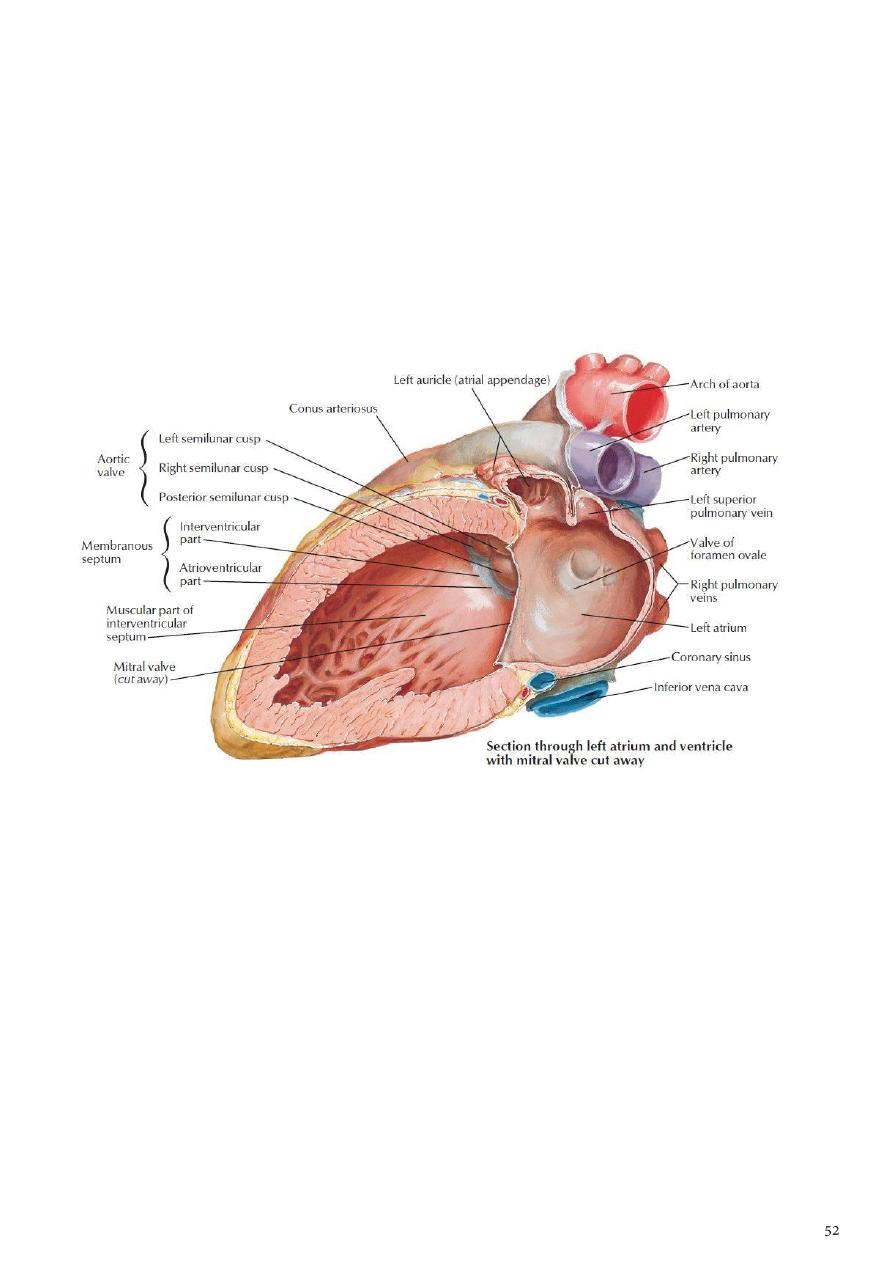
Left Atrium
1- Similar to the right atrium, the left atrium consists of a main cavity and a left auricle.
2- The interior of the left atrium is smooth, but the left auricle possessesmuscular ridges as
in the right auricle.
3- The left atrium is smooth& receives the opening of 4 pulmonary veins ( Oxygenated
blood from the lungs),2 left & 2 right pulmonary veins.
4- The 2 atria are separated by a septum showing the fossa ovalis ( Remnant of foramen
ovale during fetal life).
5- The left atrioventricular orifice is guarded by the mitral valve.
Left Ventricle
1- The walls of the left ventricle are three times thicker than those of the right ventricle.
2- In cross section, the left ventricle is circular; the right is crescentic.
3- The part of the ventricle below the aortic orifice is called the aortic vestibule.
4- The mitral valve guards the atrioventricular orifice. It consists of two cusps similar to
that of the cusps of the tricuspid valve, one anterior and one posterior, the anterior cusp
is the larger.
5- The aortic valve guards the aortic orifice and is precisely similar in structure to the
pulmonary valve. One cusp is anterior and two are posterior. Behind each cusp, the
aortic wall bulges to form an aortic sinus.
6- The anterior aortic sinus gives origin to the right coronary artery, and the left posterior
sinus gives origin to the left coronary artery.
Structure of the Heart
-
The walls of the heart are composed of a thick layer of cardiac muscle
1- the myocardium, covered externally by the epicardium and lined internally by the
endocardium.
2- The two atria are separated by interatrial septum.
3- The two ventricles are separated by interventricular septum.
4- The upper part of the septum is thin and membranous and attached to the fibrous
skeleton. The lower part of the septum is thick and formed of muscle.
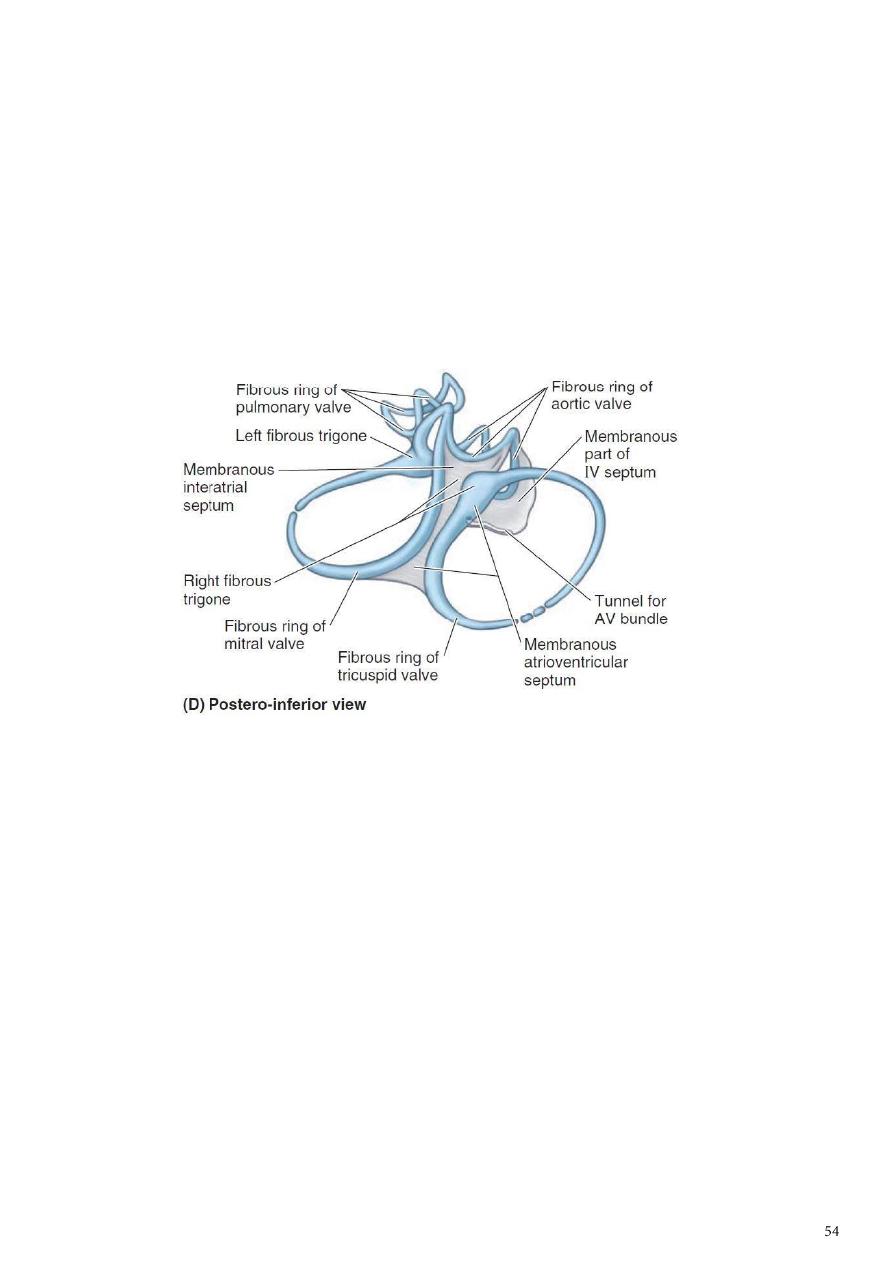
The skeleton of the heart
It consists of fibrous rings that surround the atrioventricular, pulmonary, and aortic orifices
and are continuous with the membranous upper part of the ventricular septum.
-
The fibrous rings around the atrioventricular orifices separate the muscular walls of the
atria from those of the ventricles.
-
They support the bases of the valve and prevent them from stretching and becoming
incompetent.
-
The skeleton of the heart forms the basis of electrical discontinuity between the atria
and the ventricles.
Conducting System of the Heart
1- The normal heart contracts rhythmically at about 70 to 90 beats per minute in the
resting adult.
2- The conducting system of the heart consists of specialized cardiac muscle present in the
sinuatrial node, the atrioventricular node, the atrioventricular bundle and its right and
left terminal branches, and the subendocardial plexus of Purkinje fibers (specialized
cardiac muscle fibers that form the conducting system of the heart).
Sinuatrial Node
The sinuatrial node is located on the anterior wall of the right atrium in the upper part of
the sulcus terminalis just to the right of the opening of the superior vena cava. It
spontaneously initiates rhythmic electrical impulses that spread in all directions through the
cardiac muscle of the atria and cause the muscle contraction.
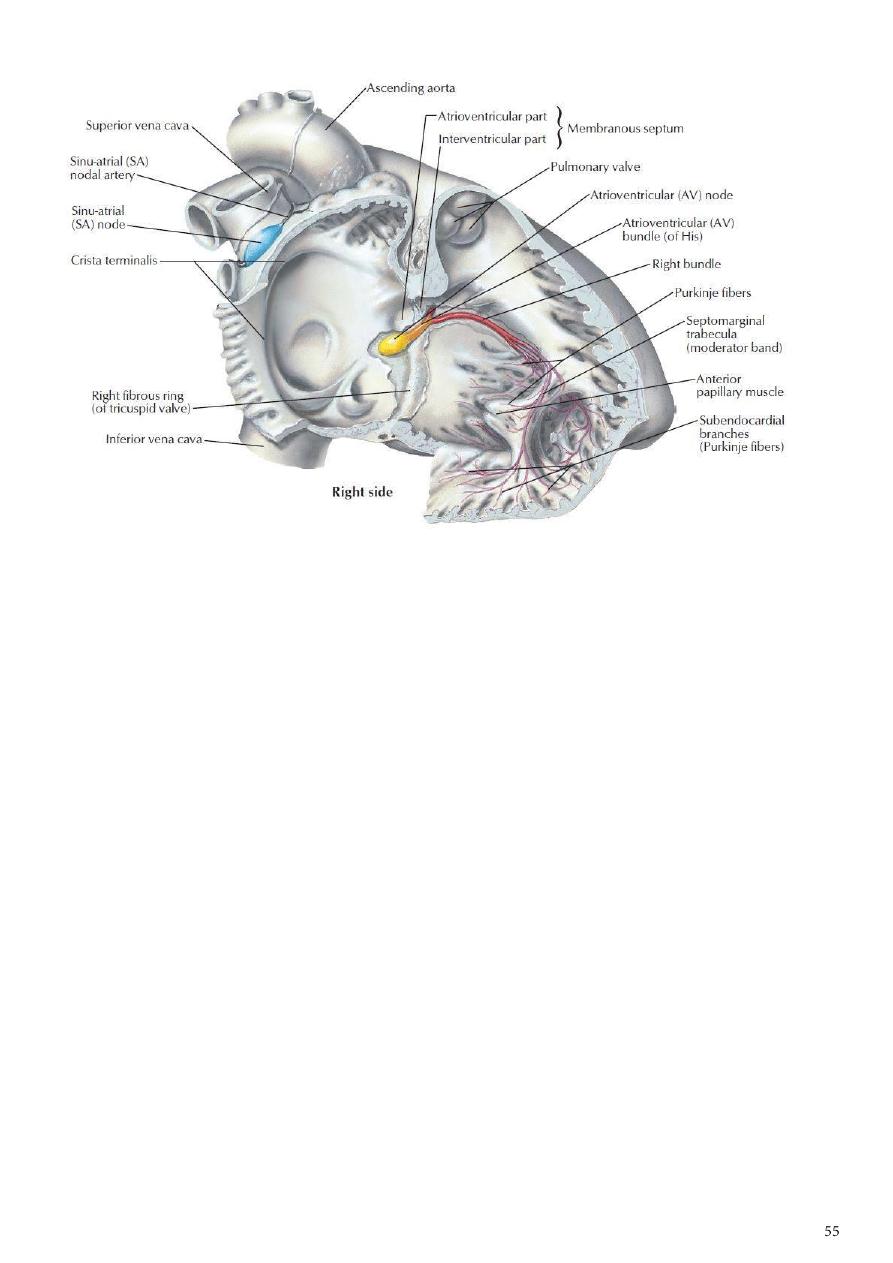
Atrioventricular Node (AV node)
The AV node is placed on the lower part of the atrial septum to the left side of the opening
of Coronary venous sinus. The cardiac impulse is conducted from AV node to the ventricles
by the atrioventricular bundle. It is stimulated by the excitation wave from atrial
myocardium.
Atrioventricular Bundle (AV bundle)
The atrioventricular bundle (bundle of His) is the only route along which the cardiac
impulse can travel from the atria to the ventricles. The bundle descends in the
membranous part of the ventricular septum and to the muscular part of septum where it
divides into two branches, one for each ventricle.
1- The right one toward the apex of the heart to inter the moderater band & finally
reaches the anterior papillary muscle and breaks into a number of Purkinje fibers to all
parts of the Right ventricular wall.
2- The left bundle branch goes to bases of papillary muscles & breaks into a number
Purkinje fibers in the wall of left ventricle.
The conducting system of the heart is responsible for
1- generating rhythmic cardiac impulses
2- conducting these impulses rapidly throughout the myocardium & the different
chambers contract in a coordinated and efficient manner.
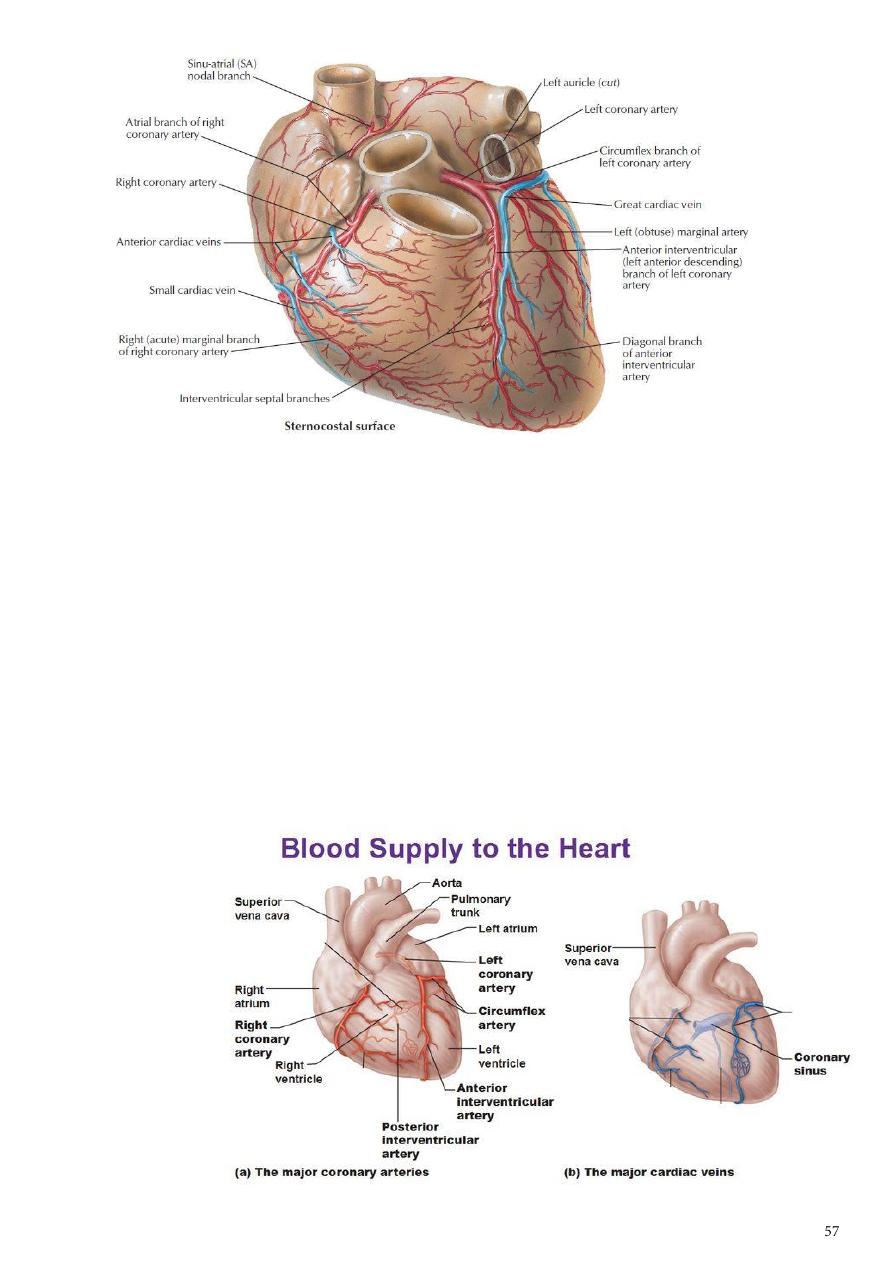
The Arterial Supply of the Heart
The arterial supply of the heart is provided by the right and left coronary arteries, which
arise from the ascending aorta & run within subepicardial connective tissue.
The right coronary artery
arises from the anterior aortic sinus
runs forward between the pulmonary trunk and the right auricle.
It descends vertically in the right atrioventricular groove
at the inferior border of the heart it continues posteriorly along the atrioventricular
groove to anastomose with the left coronary artery in the posterior interventricular
groove.
It supplies the right atrium and right ventricle and parts of the left atrium and left
ventricle and the atrioventricular septum. It gives the following branches:
1- Marginal
2- Posterior interventricular
3- S.A nodal
4- Anterior atrial &ventricular branches
The left coronary artery
is usually larger than the right coronary artery
supplies the major part of the heart, including the greater part of the left atrium, left
ventricle, and ventricular septum.
It arises from the left posterior aortic sinus and passes forward between the pulmonary
trunk and the left auricle.
It then enters the atrioventricular groove and divides into an anterior interventricular
branch and a circumflex branch.
Branches
1- Circumflex
2- Anterior interventricular
3- L.Marginal
4- L. conus
5- L.ventricular&atrial
The collateral circulation of the heart:
the terminal branches of the right and left coronary arteries Anastomoses between each
other, but they are usually not large enough to provide an adequate blood supply to the
cardiac muscle if one of the large branches become blocked by disease.
A sudden block of one of the larger branches of either coronary artery usually leads to
myocardial death (myocardial infarction), although sometimes the collateral circulation is
enough to sustain the muscle.
Venous Drainage of the Heart
Is mainly via Coronary venous sinus ( direct continuity of great cardiac vein).
The coronary sinus receives the following tributaries before opening into the R.A:
1-Great cardiac V
2-Middle cardiac
3-Small cardiac
4-Oblique V of L.A
5-Post. V of L.V .
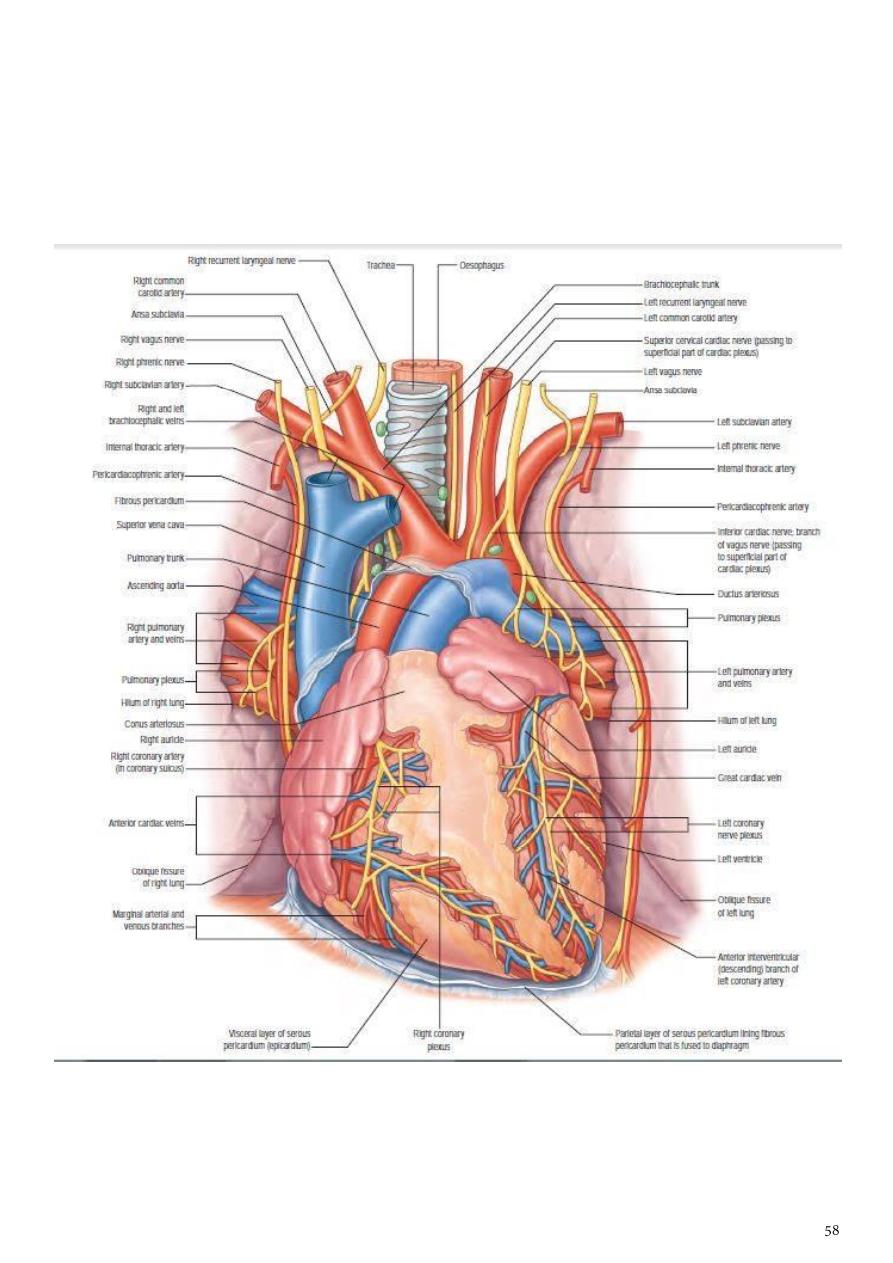
Nerve Supply of the Heart
1- Is achieved by Autonomic nervous system( sympathetic component coming from upper
4-5 thoracic segments of the spinal cord)
2- while parasympathetic component via cardiac branches of R & L vagus nerves.
3- Fibers from both sympathetic & parasympathetic communicates to form superficial &
deep cardiac plexuses which goes directly to supply the heart & coronary arteries.
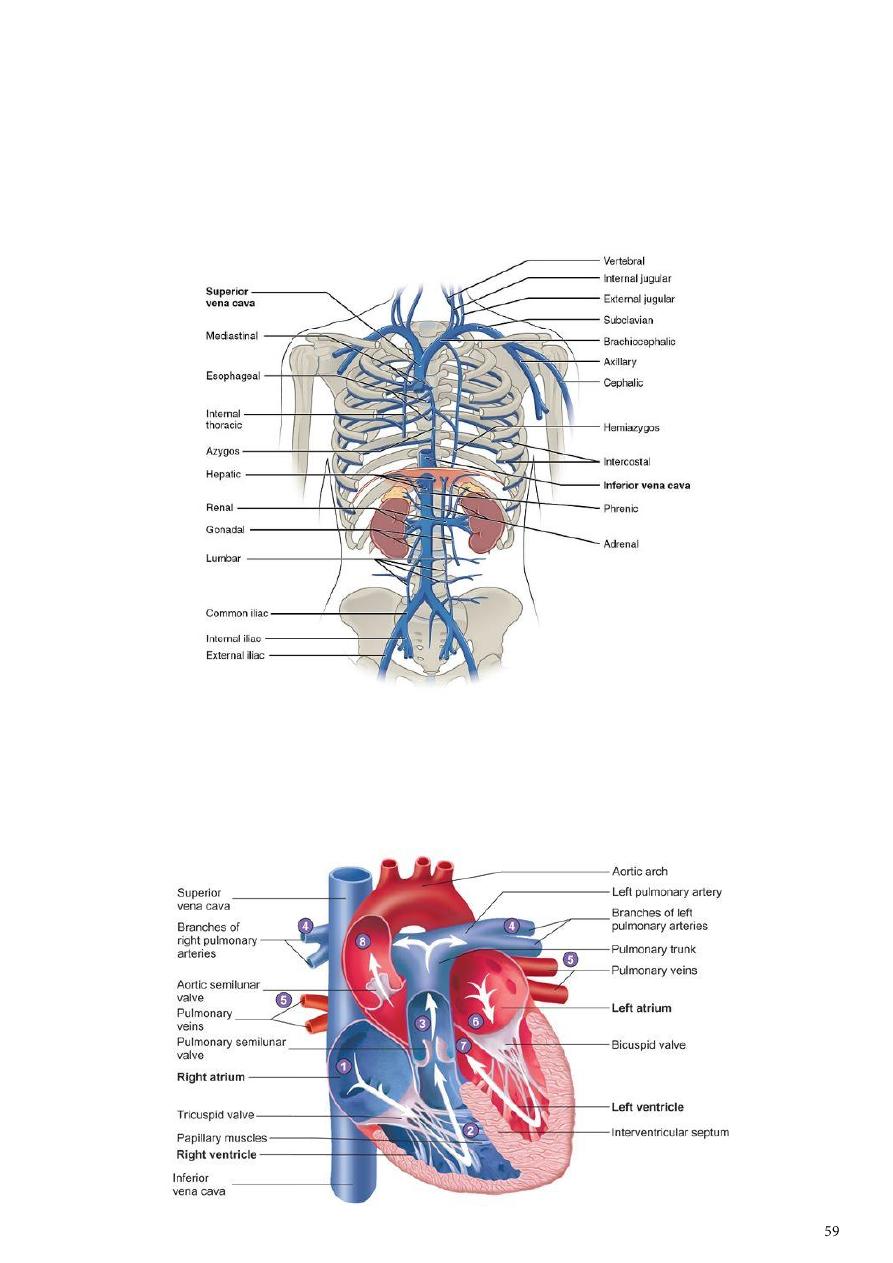
Brachiocephalic Veins
1- The right brachiocephalic vein is formed at the root of the neck by the union of the right
subclavian and the right internal jugular veins.
2- The left brachiocephalic vein has a similar origin. It passes obliquely downward and to
the right behind the manubrium sterni and in front of the large branches of the aortic
arch. It joins the right brachiocephalic vein to form the superior vena cava.
Superior Vena Cava
1- The superior vena cava contains all the venous blood from the head and neck and both
upper limbs
2- It is formed by the union of the two brachiocephalic veins.
3- It passes downward to end in the right atrium.
Azygos Vein
1- The origin of the azygos vein is variable.
It is often formed by the union of the
right ascending lumbar vein and the
right subcostal vein.
2- It ascends through the aortic opening in
the diaphragm on the right side of the
aorta to the level of the fifth thoracic
vertebra. Here it arches forward above
the root of the right lung to empty into
the posterior surface of the superior
vena cava.
3- The azygos vein has numerous
tributaries:
1-
the eight lower right intercostal
veins
2-
the right superior intercostal vein
3-
the superior and inferior
hemiazygos veins
4-
Numerous mediastinal veins
Aorta
1- The aorta is the main arterial trunk that
delivers oxygenated blood from the left ventricle of the heart to the tissues of the body.
2- It is divided for purposes of description into the following parts:
a- ascending aorta
b- arch of the aorta
c- descending
thoracic aorta
d- abdominal
aorta.
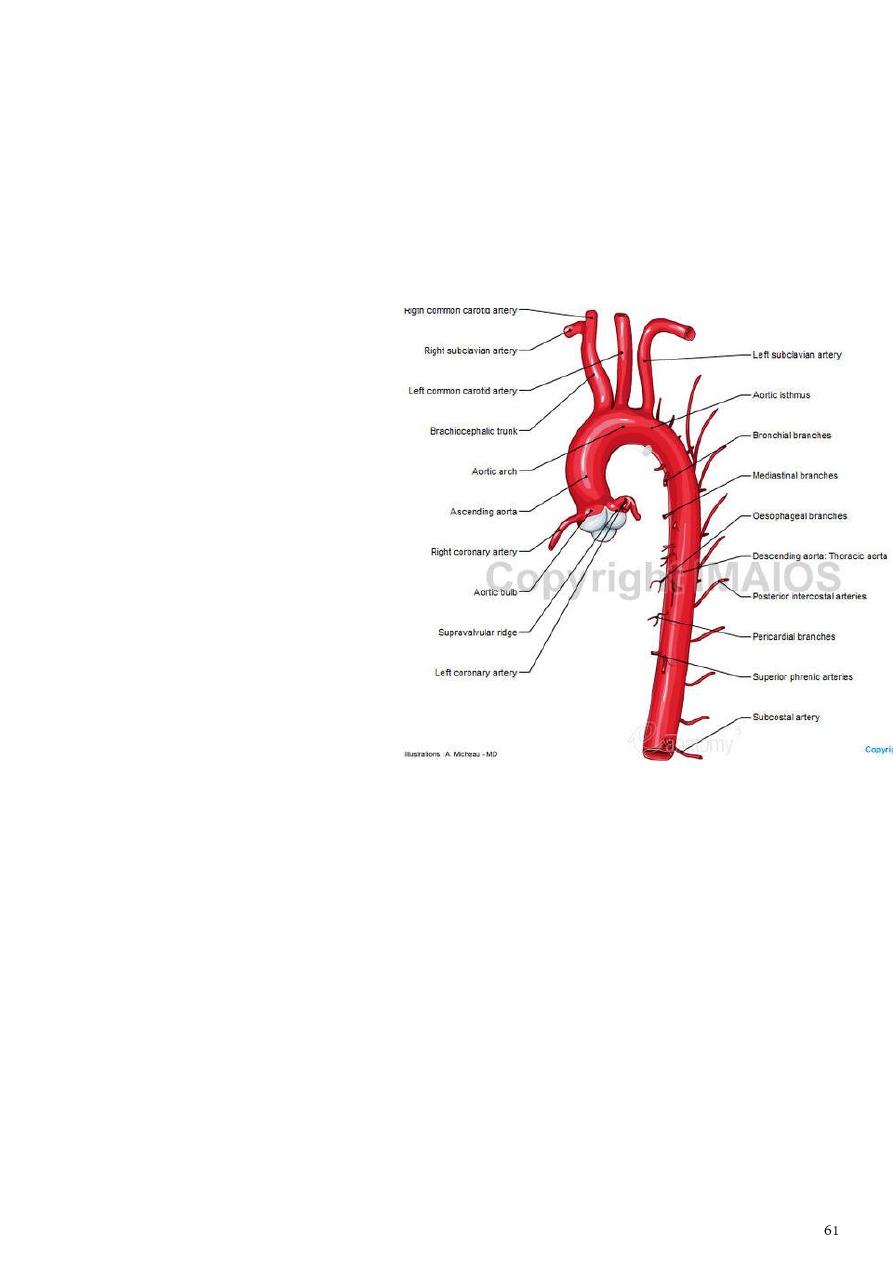
Ascending Aorta
The ascending aorta begins at the base of the left ventricle and runs upward and forward to
come to lie behind the right half of the sternum at the level of the sternal angle, where it
becomes continuous with the arch of the aorta.
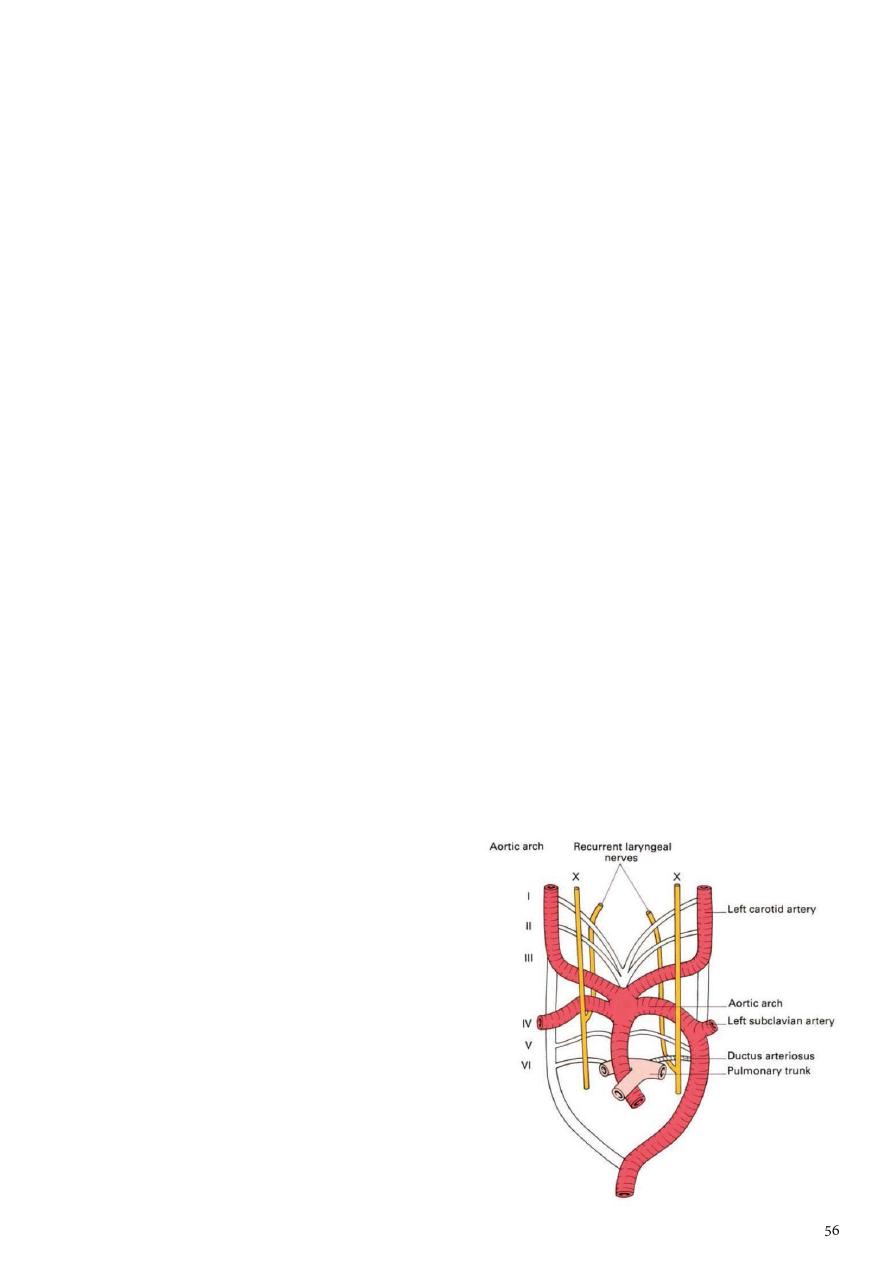
Arch of the Aorta
1- The arch of the aorta is a continuation of the ascending aorta.
2- It lies behind the manubrium sterni and arches upward, backward, and to the left in
front of the trachea.
3- It then passes downward to the left
of the trachea and, at the level of
the sternal angle, becomes
continuous with the descending
aorta.
Branches:
1-
The brachiocephalic artery
arises from the aortic arch. It
divides into the right subclavian
and right common carotid
arteries
2-
The left common carotid artery
3-
The left subclavian artery
Descending Thoracic Aorta
1- The descending thoracic aorta lies in the posterior mediastinum and begins as a
continuation of the arch of the aorta on the lower border of the body of the T4
(opposite sternal angle).
2- It runs downward in the posterior mediastinum, inclining forward and medially to reach
the anterior surface of the vertebral column.
3- At the level of the T12, it passes behind the diaphragm (through the aortic opening) in
the midline and becomes continuous with the abdominal aorta.
Branches :
1-
Posterior intercostal arteries are given off to the lower nine intercostal spaces on
each side.
2-
Subcostal arteries are given off on each side and run along the lower border of the
12th rib to enter the abdominal wall.
3-
Pericardial, esophageal, and bronchial arteries are small branches that are distributed
to these organs.
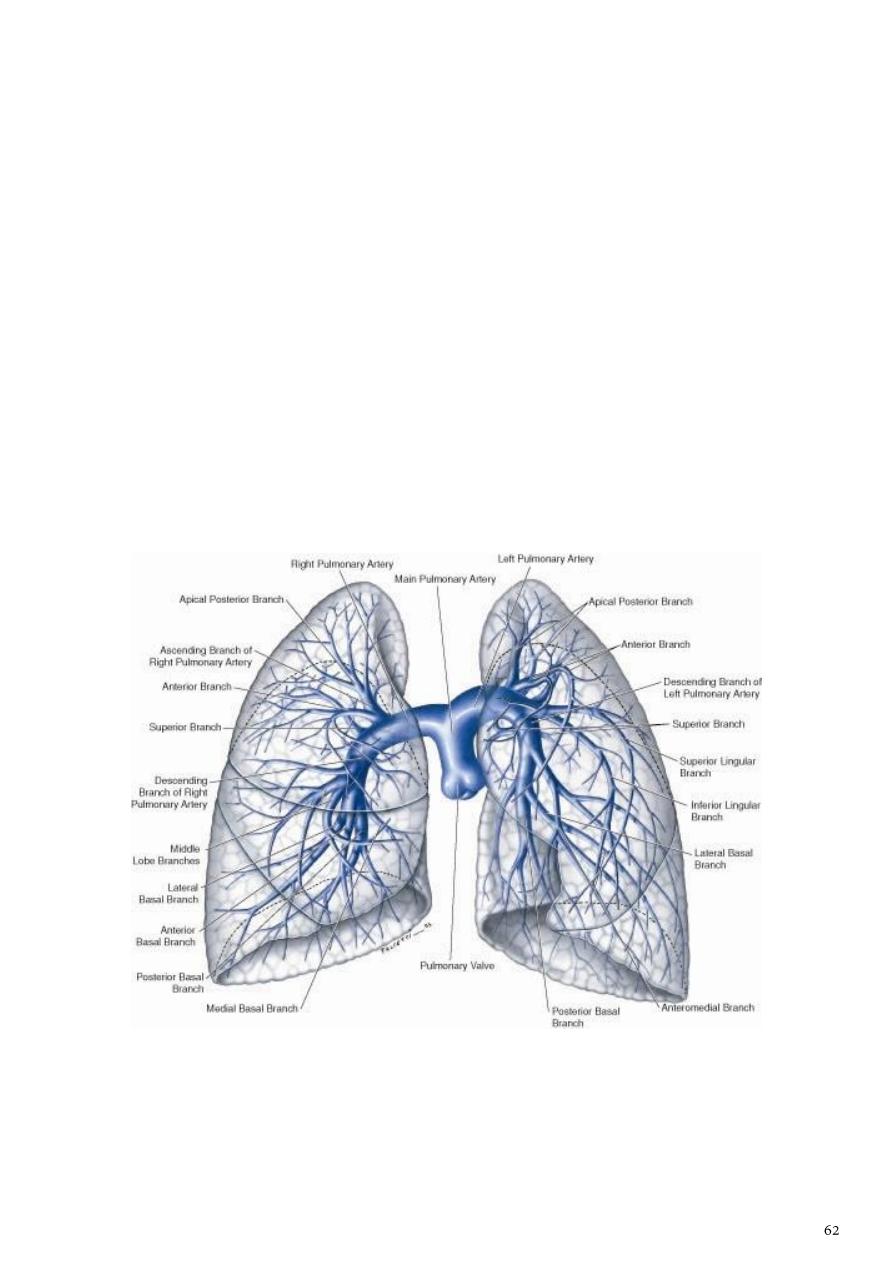
Pulmonary Trunk
1- The pulmonary trunk conveys deoxygenated blood from the right ventricle of the heart
to the lungs.
2- It leaves the upper part of the right ventricle and runs upward, backward, and to the
left.
3- It is about (5 cm) long and terminates in the concavity of the aortic arch by dividing into
right and left pulmonary arteries.
4- it is enclosed in the fibrous pericardium and a sheath of serous pericardium together
with the ascending aorta.
Branches :
1-
The right pulmonary artery runs to the right behind the ascending aorta and superior
vena cava to enter the root of the right lung.
2-
The left pulmonary artery runs to the left in front of the descending aorta to enter
the root of the left lung
The ligamentum arteriosum
1- A fibrous band that connects the bifurcation of the pulmonary trunk to the lower
concave surface of the aortic arch.
2- It is the remains of the ductus arteriosus, which in the fetus conducts blood from the
pulmonary trunk to the aorta, thus bypassing the lungs.
3- The left recurrent laryngeal nerve hooks around the lower border of this structure. After
birth, the ductus closes.
4- If it remains patent, aortic blood will enter the pulmonary circulation, producing
pulmonary hypertension and hypertrophy of the right ventricle.

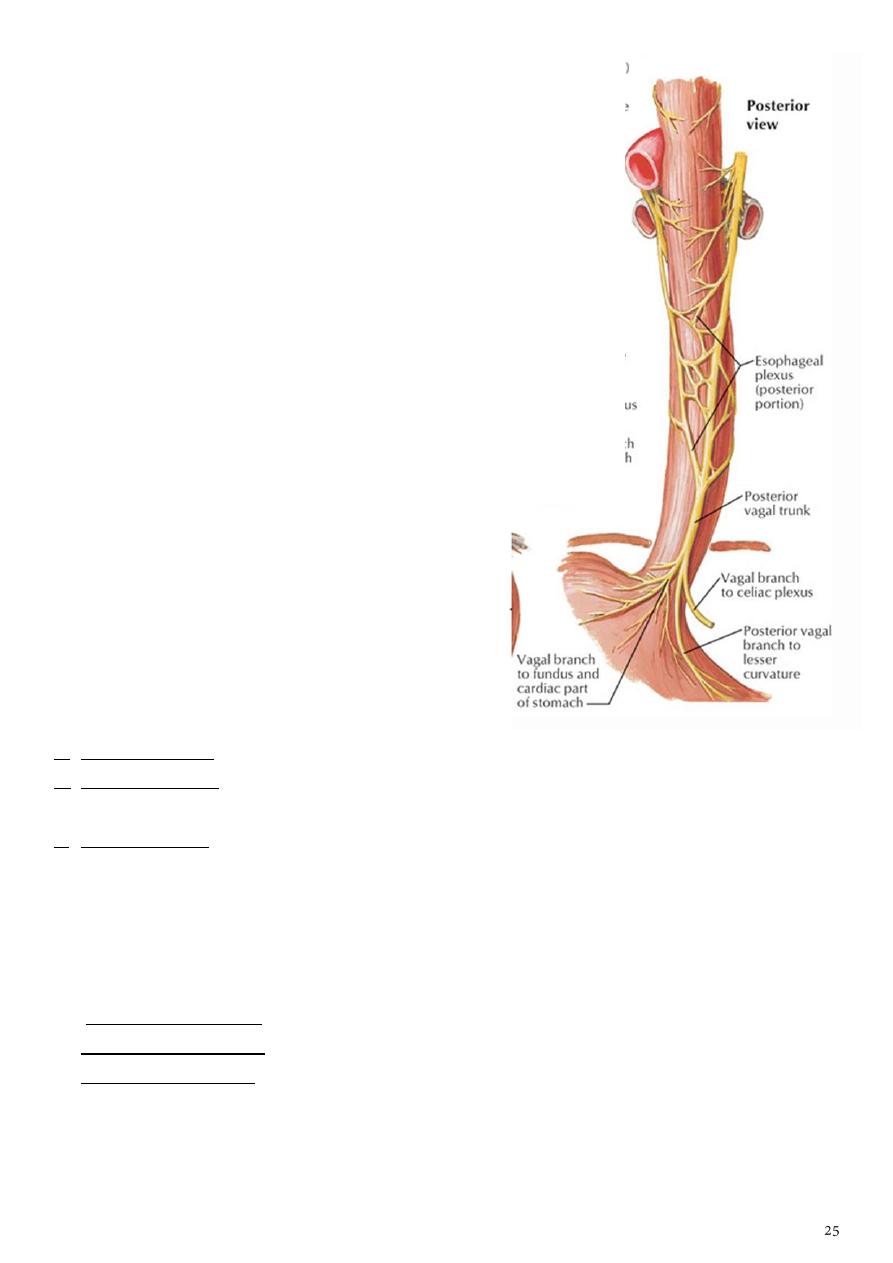
Vagus Nerves
1- The right vagus nerve
a- descends in the thora
b- first lying posterolateral to the brachiocephalic artery.
c- It passes behind the root of the right lung and assists in the formation of the
pulmonary plexus.
d- On leaving the plexus, the vagus passes to the posterior surface of the esophagus
and takes part in the formation of the esophageal plexus.
e- It then passes through the esophageal opening of the diaphragm behind the
esophagus to reach the posterior surface of the stomach.
2- The left vagus nerve
a- descends in the thorax between the left common carotid and the left subclavian
arteries.
b- It then crosses the left side of the aortic arch and is itself crossed by the left phrenic
nerve.
c- The vagus then turns backward behind the root of the left lung and assists in the
formation of the pulmonary plexus.
d- On leaving the plexus, the vagus passes onto the anterior surface of the esophagus
and takes part in the formation of the esophageal plexus.
e- It then passes through the esophageal opening in the diaphragm in front of the
esophagus to reach the anterior surface of the stomach.
Branches
-
Both vagi supply the lungs and esophagus.
-
The right vagus gives off cardiac branches. The right recurrent laryngeal nerve arises
from the right vagus in the neck and hooks around the subclavian artery and ascends
between the trachea and esophagus.
-
The left vagus gives origin to the left recurrent laryngeal nerve which arises from the
left vagus trunk as the nerve crosses the arch of the aorta. It hooks around the
ligamentum arteriosum and ascends in the groove between the trachea and the
esophagus on the left side . It supplies all the muscles acting on the left vocal cord
(except the cricothyroid muscle, a tensor of the cord, which is supplied by the
external laryngeal branch of the vagus).
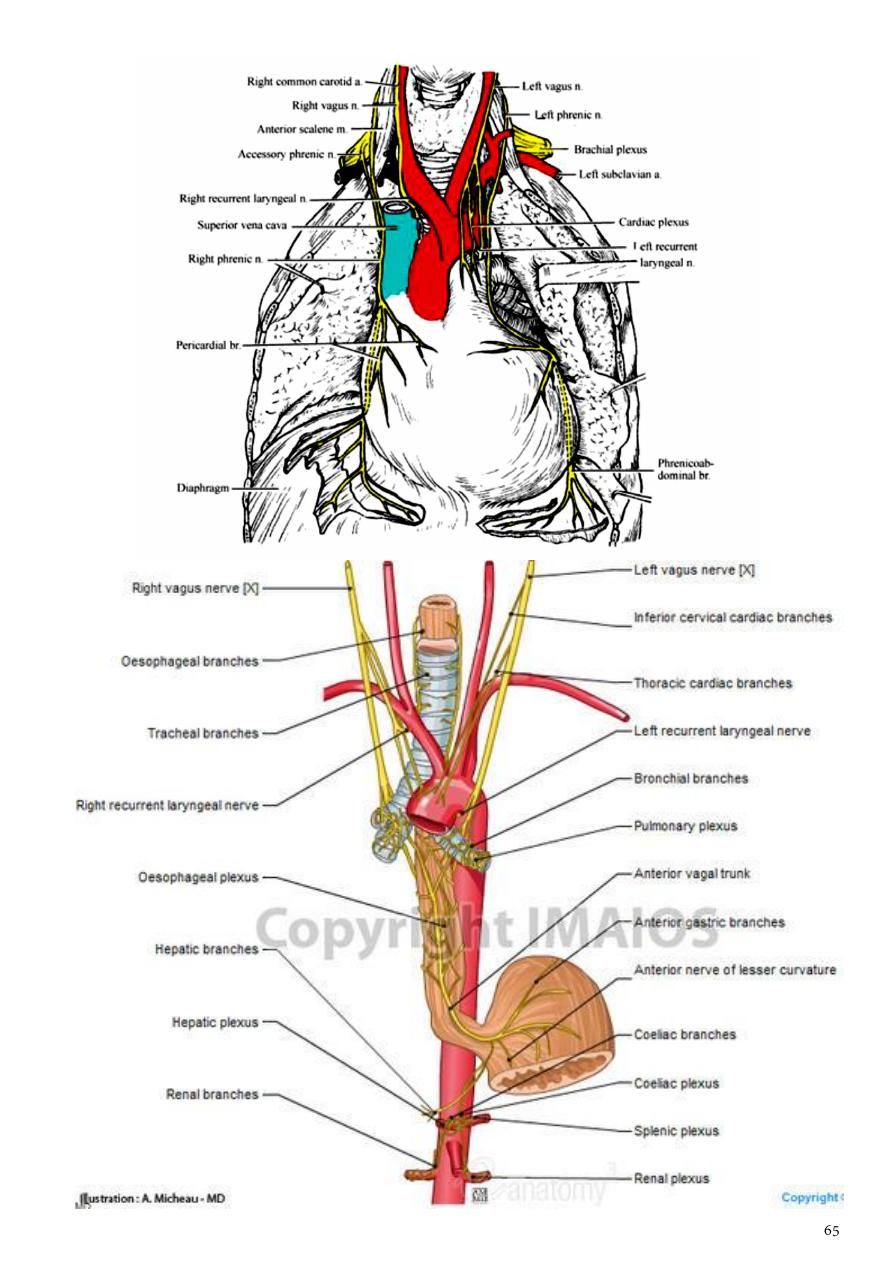
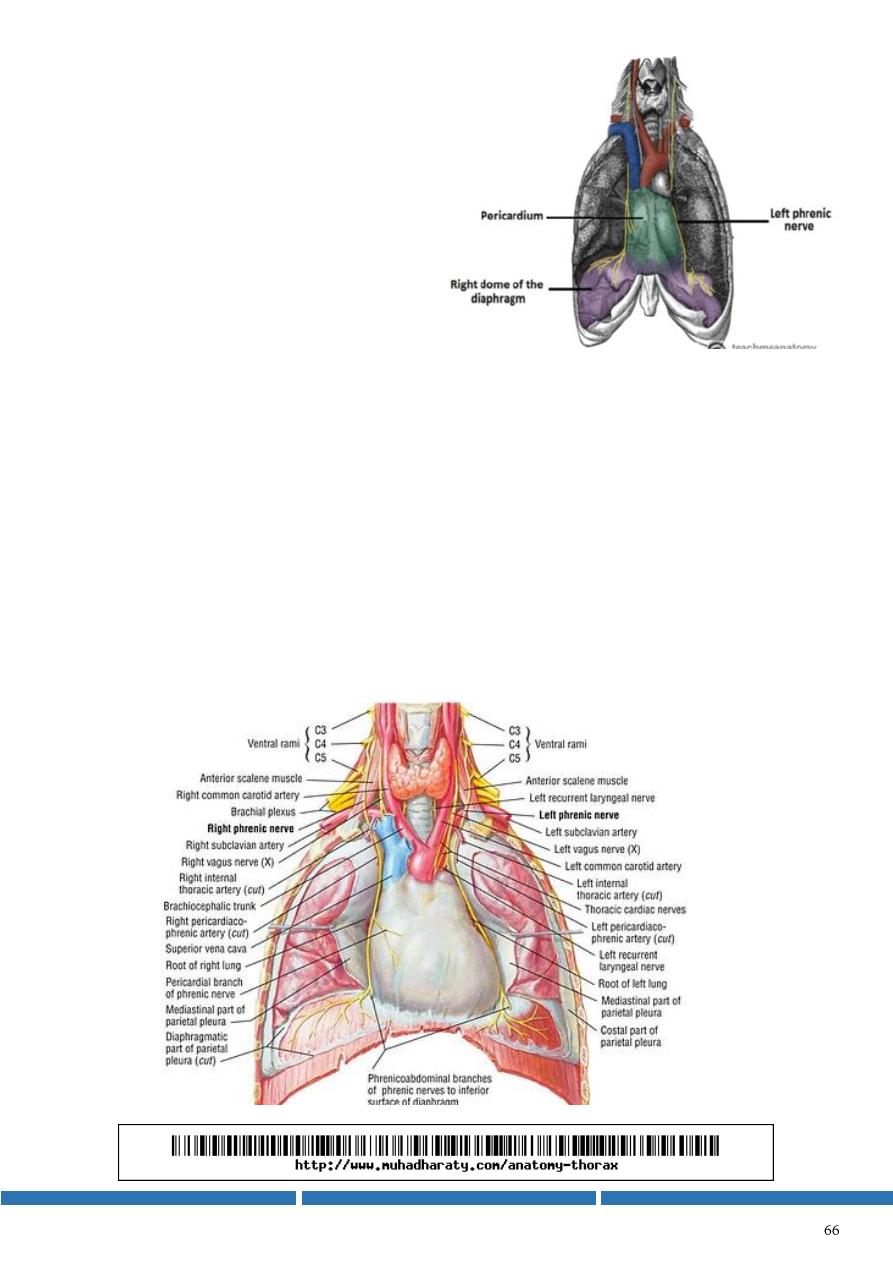
Phrenic Nerves
The phrenic nerves arise from the neck from
the anterior rami of the C3, C4, and C5
cervical nerves.
The right phrenic nerve
1- descends in the thorax along the right
side of the right brachiocephalic vein
and the superior vena cava.
2- It passes in front of the root of the
right lung and runs along the right side of the pericardium.
3- It then descends on the right side of the inferior vena cava to the diaphragm.
4- Its terminal branches pass through the caval opening in the diaphragm to supply the
central part of the peritoneum on its underaspect.
The left phrenic nerve
1- descends in the thorax along the left side of the left subclavian artery.
2- It crosses the aortic arch and here crosses the left vagus nerve.
3- It passes in front of the root of the left lung and then descends over the left surface
of the pericardium, which separates the nerve from the left ventricle.
4- On reaching the diaphragm, the terminal branches pierce the muscle and supply the
central part of the peritoneum on its underaspect.
