Infectious disease 4
Hand-Foot-and-Mouth Disease( it is Common )
One of the more distinctive rash syndromes, is most frequently caused by coxsackievirus A16.
Highly infectious.
Peak incidence in late summer and in fall.
Clinical Presentation
Prodrome of fever, anorexia, sore throat.
Oval blisters in acral distribution, usually few in number.
Shallow, oral erosions on erythematous base in oral mucosa.
Vesicles resolve in about 1 wk.
HFMD
A. Oval blisters of the palms
B. Oval blisters on the feet
C. Erosion of the tongue
Herpes Simplex Virus
The 2 closely related herpes simplex viruses (HSVs), HSV type 1 (HSV-1) and HSV type 2 (HSV-2), cause a variety of illnesses, depending on the:
Anatomic site where the infection is initiated.
Immune state of the host.
whether the symptoms reflect primary or recurrent infection.
HSV is a double-stranded DNA.
The mode of transmission is direct contact between mucocutaneous surfaces.
All infected individuals harbor latent infection and experience recurrent infections, which may be symptomatic or may go unrecognized, and thus are periodically contagious.
HSV-1 and HSV-2 are equally capable of causing initial infection at any anatomic site but differ in their capacity to cause recurrent infections.
HSV-1 has a greater propensity to cause recurrent oral infections,
HSV-2 has a greater proclivity to cause recurrent genital infections.
CLINICAL MANIFESTATIONS
The hallmarks of common HSV infections are skin vesicles and shallow ulcers. Classic infections manifest as small, 2-4 mm vesicles that may be surrounded by an erythematous base.
Acute Oropharyngeal Infections: the gums become markedly swollen, and vesicles may develop throughout the oral cavity, including the gums, lips, tongue, palate, tonsils, pharynx, and perioral skin. During the initial phase of the illness there may be tonsillar exudates suggestive of bacterial pharyngitis.
Clustered perioral vesicles and erosions in an infant with primary herpetic gingivostomatitis
Herpes Labialis: fever, blisters (cold sores) are the most common manifestation of recurrent HSV-1 infections. The most common site of herpes labialis is the lip, although lesions sometimes occur on the nose, chin, cheek, or oral mucosa.
Cutaneous Infections:
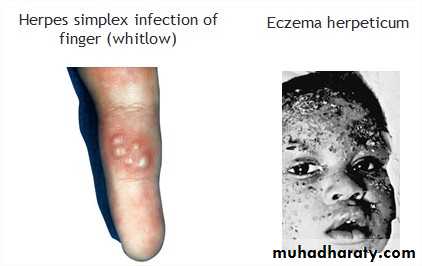
Herpes whitlow is a term generally applied to HSV infection of fingers or toes.
Eczema herpeticum: cutaneous HSV infections can be severe or life-threatening in patients with disorders of the skin such as eczema.
Genital Herpes: usually caused by HSV-2. It is common in adolescents and young adults.
Ocular Infections: HSV ocular infections may involve the conjunctiva, cornea, or retina. Vesicular lesions may be seen on the lid margins and periorbital skin.
CNS infection: It is an acute necrotizing infection generally involving the frontal and/or temporal cortex and the limbic system and, beyond the neonatal period, is almost always caused by HSV-1.
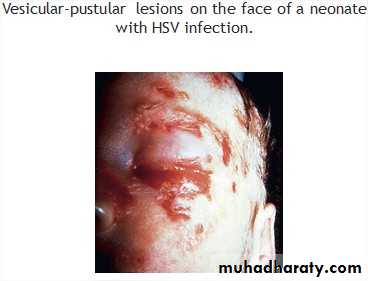
Perinatal Infections: HSV infection may be acquired in utero, during the birth process, or during the neonatal period.
IU infection typically have skin vesicles, eye findings including chorioretinitis and keratoconjunctivitis, and microcephaly or hydranencephaly.
Infection during delivery or the postpartum period present with 1 of the following 3 patterns of disease:
Disease localized to the skin, eyes, or mouth.
Encephalitis with or without skin, eye, and mouth disease.
Disseminated infection involving multiple organs, including the brain, lungs, liver, heart, adrenals, and skin.
TREATMENT
Early initiation of therapy with acyclovir, valacyclovir, or famciclovir results in the maximal therapeutic benefit.Leishmaniasis
The leishmaniases are parasites of the genus Leishmania, which are transmitted by sand flies.
Multiple species of Leishmania are known to cause human disease involving the skin and mucosal surfaces and the visceral reticuloendothelial organs.
Cutaneous disease is generally mild but may cause cosmetic disfigurement.
Mucosal and visceral leishmaniasis is associated with significant morbidity and mortality.
CLINICAL MANIFESTATIONS
Localized Cutaneous Leishmaniasis: LCL (Oriental sore) can affect individuals of any age, but children are the primary victims in many endemic regions. It may present as 1 or a few papular, nodular, plaque like, or ulcerative lesions that are usually located on exposed skin, such as the face and extremities, may ulcerate over the course of several weeks to months. It may associated with regional LAP. If lesions do not become secondarily infected, there are usually no complications aside from the residual cutaneous scar.
Diffuse Cutaneous Leishmaniasis: DCL manifests as large nonulcerating macules, papules, nodules, or plaques that often involve large areas of skin. The face and extremities are most commonly involved. It is thought that an immunologic defect underlies this severe form of cutaneous leishmaniasis.
Mucosal Leishmaniasis: ML is an uncommon but serious manifestation of leishmanial infection resulting from hematogenous metastases to the nasal or oropharyngeal mucosa from a cutaneous infection.
Visceral Leishmaniasis (kala-azar): اخطر شي
The classic clinical features is high fever, marked splenomegaly, hepatomegaly, and severe cachexia.
At the terminal stages of kala-azar the HSM is massive, there is gross wasting, the pancytopenia is profound, and jaundice, edema, and ascites may be present.
Anemia may be severe enough to precipitate heart failure. Bleeding episodes, especially epistaxis, are frequent.
The late stage of the illness is often complicated by secondary bacterial infections, which frequently are a cause of death.
A younger age at the time of infection and underlying malnutrition may be risk factors for the development and more rapid evolution of active VL.
Death occurs in more than 90% of patients without specific antileishmanial treatment.
DIAGNOSIS
Patients with cutaneous leishmaniasis or ML generally do not have abnormal laboratory results unless the lesions are secondarily infected with bacteria.
Laboratory findings associated with classic kala-azar include anemia, thrombocytopenia, leukopenia, elevated hepatic transaminase levels, and hyperglobulinemia that is mostly IGg.
Serologic testing is very useful in VL because of the very high level of antileishmanial antibodies.
In patients with VL, smears or cultures of material from splenic, bone marrow, or lymph node aspirations are usually diagnostic.
TREATMENT
The sodium stibogluconate (Pentostam), is the mainstay of antileishmanial chemotherapy .
Recommended regimen 20 mg/kg/day IV or IM for:
20 days (for severe LCL and DCL).
28 days (for ML and VL).