Placenta & Fetal
membranes
Prof. Dr. Malak A. Al-yawer
Department of Anatomy/ Embryology Section

Objectives
The 1
st
medical student will be able to answer the following
questions after reading this lecture
Define the different components of placenta
Define spiral arteries and mention their significance during
pregnancy
State the Changes that occur in spiral arteries in preclampsia
Mention the placental changes at the end of pregnancy
Define some placental abnormalities
Describe in a few sentences the surfaces of delivered placenta
State the significance of examination of placenta
Mention the structures passing through primitive umblical ring,
primitive umbilical cord and umbilical cord
Define umbilical cord & mention their abnormalities
Enumerate the fetal membranes
Compare between arrangement of fetal membranes in
monozygotic and dizygotic twins
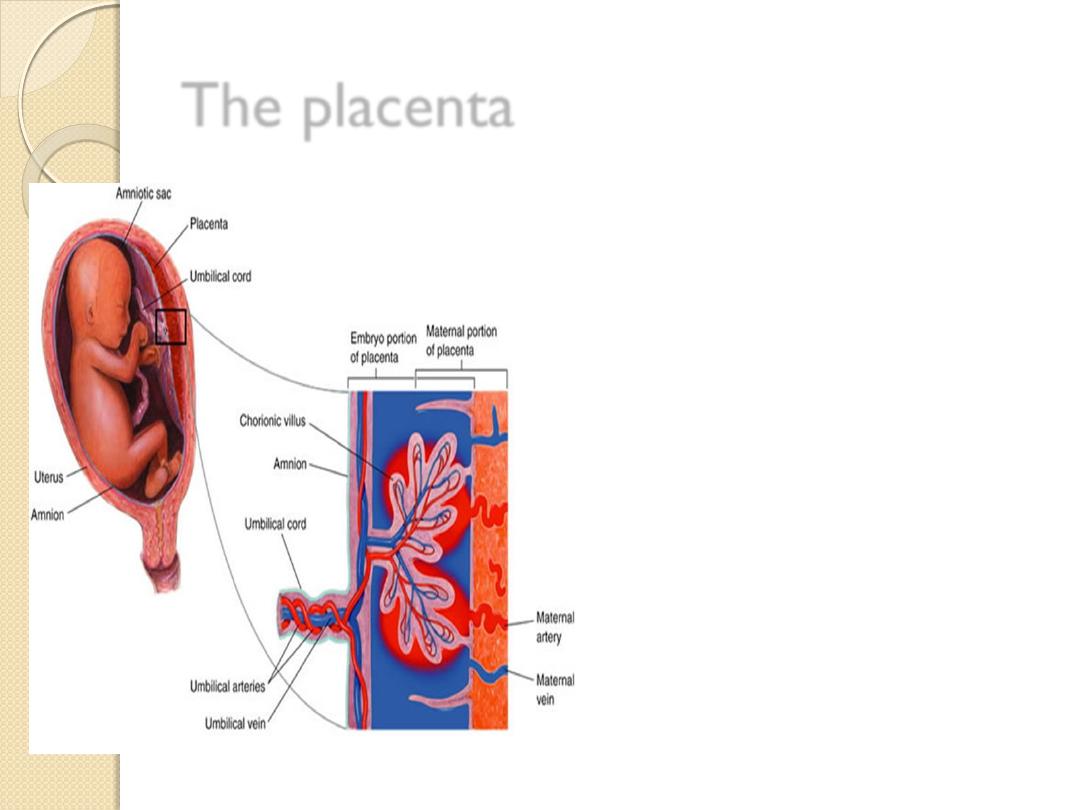
The placenta
is a fetomaternal organ
that has two
components :
A fetal part that
develops from the
chorionic sac
A maternal part that is
derived from the
endometrium

The three regions of the decidua are named according
to their relation to the implantation site
The
decidua basalis
is
the part of the decidua
deep to the conceptus that
forms the maternal part of
the placenta.
The
decidua capsularis
is the superficial part of
the decidua overlying the
conceptus.
The
decidua parietalis
is
all the remaining parts of
the decidua.

CHORION
Chorion laeve
:
•
is the greater part of
the chorion
•
is in contact with
decidua capsularis
•
becomes smooth.
Chorion frondosum
:
•
is in contact with
decidua basalis
•
the villi over this part
increase greatly in size
and complexity

Spiral arteries
Maternal blood is delivered
to the placenta by spiral
arteries in the uterus.
Erosion of these maternal
vessels to release blood
into intervillous spaces is
accomplished by
endovascular invasion by
cytotrophoblast cells.

Cytotrophoblast cells invade the
terminal ends of spiral arteries
creating hybrid vessels
cytotrophoblast cells undergo an
epithelial to endothelial
transition.
Invasion of the spiral arteries by
cytotrophoblast cells transforms
these vessels from small-
diameter, high-resistance vessels
to larger-diameter, low-
resistance vessels

Preeclampsia
is a condition characterized by
maternal hypertension,
proteinuria, and edema.
It may begin suddenly anytime
from about 20 weeks’ gestation
to term and
The condition appears to be a
trophoblastic disorder related
to:
failed or incomplete
differentiation of
cytotrophoblast cells,
many of which do not undergo
their normal epithelial to
endothelial transformation

Structure of the Placenta
By the beginning of the
fourth month, the
placenta has two
components:
(a) a fetal portion,
formed by the chorion
frondosum and
(b) a maternal portion,
formed by the decidua
basalis
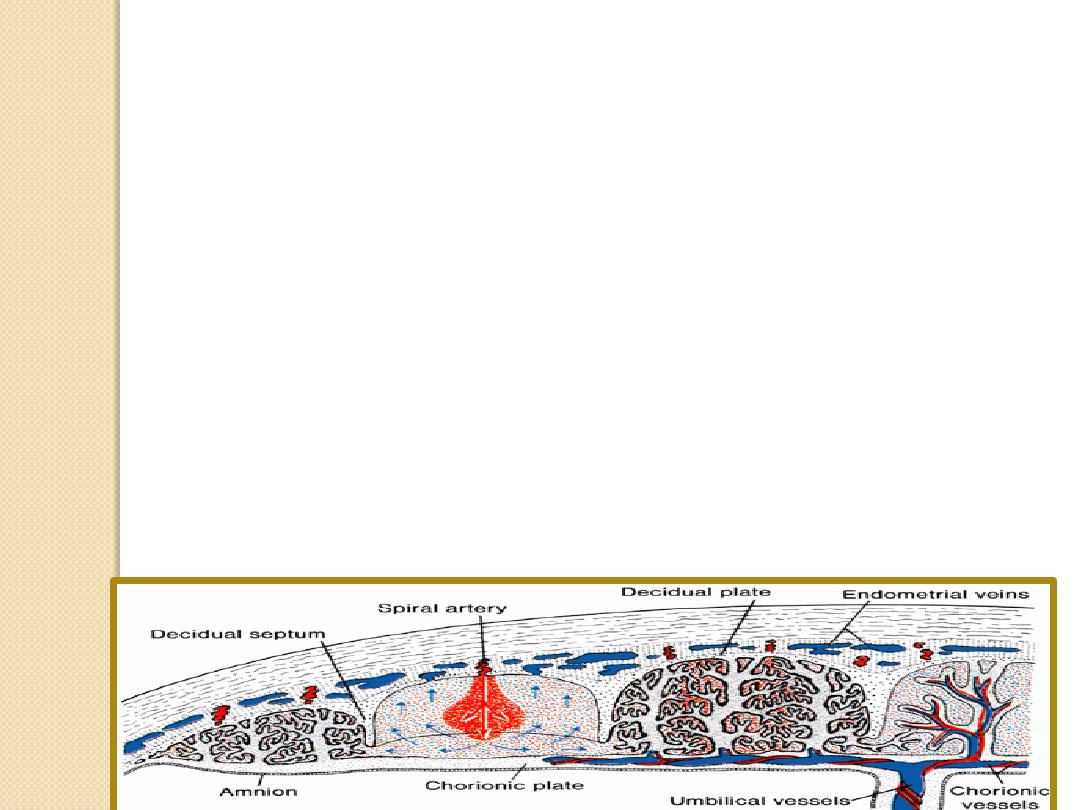
On the fetal side, the placenta is bordered by the
chorionic plate
On the maternal side, the placenta is bordered the
decidual plate
junctional zone: trophoblast and decidual cells
intermingle. This zone
During 4
th
& 5
th
months, the decidua forms a number of
decidual septa, which project into intervillous spaces
The placenta is divided into a number of compartments, or
cotyledons
These septa do not reach the chorionic plate (contact
between intervillous spaces in the various cotyledons is
maintained).

Structure of villi at various stages of development
placental membrane
4
th
week 4
th
m
onth

Placental Abnormalities
Placenta Accreta :
Abnormal adherence, with
absence of decidua basalis.
Placenta Increta :
Occurs when the placenta
penetrates into the uterine
muscle, but does not
penetrate the uterine
serosa.
Placenta Percreta :
Placental villi penetrate
myometrium and through
to uterine serosa
.


Placental Abnormalities
When the blastocyst
implants close to or
overlying the internal
os of the uterus, the
abnormality is called
placenta previa.

Separation of the placenta
The placenta is torn from the uterine wall approximately 30 minutes
after birth of the child, is expelled from the uterine cavity.
The expelled placenta
is discoid with a diameter of 15 to 25 cm,
is approximately 3 cm thick, and
weighs about 500 to 600 g.

The fetal surface of the placenta
( facing the fetus )
Has a shiny ,smooth surface provided by the amniotic membrane that
covers it .
A number of large arteries and veins, the chorionic vessels, converge
toward the umbilical cord .
The attachment of the umblical cord is usually eccentric.

maternal side of the placenta
Is textured and spongy looking
Is divided by a series of fissures into lobules or
cotyledons
The fissures contain the remains of septae which
extended between the maternal and fetal portions

Examination of the placenta
prenatally by
ultrasonography or
magnetic resonance
imaging. or
postnatally by gross
and microscopic study
may provide clinical
information about the
causes of
1.
IUGR,
2.
placental dysfunction,
3.
fetal distress and
death, and
4.
neonatal illness .

Placental studies
can also determine whether the placenta
is complete. Retention of a cotyledon or
an accessory placenta in the uterus may
cause severe uterine hemorrhage .

Placental Changes at the end of
Pregnancy
(a) an increase in fibrous tissue in the core
of the villus,
(b) thickening of basement membranes in
fetal capillaries,
(c) obliterative changes in small capillaries of
the villi, and
(d) deposition of fibrinoid on the surface of
the villi in the junctional zone and in the
chorionic plate. Excessive fibrinoid
formation frequently causes infarction of an
intervillous lake or sometimes of an entire
cotyledon.

PRODUCTION OF
HORMONES
•
The placenta (
syncytiotrophoblast )
is classified as an
endocrine organ .
•
It produces both
protein and steroid
hormones
1. human Chorionic
Gonadotropin ( hCG)
2. estrogen
3. Progestrone
4. human Chorionic
Somatomammotropin (hCS )
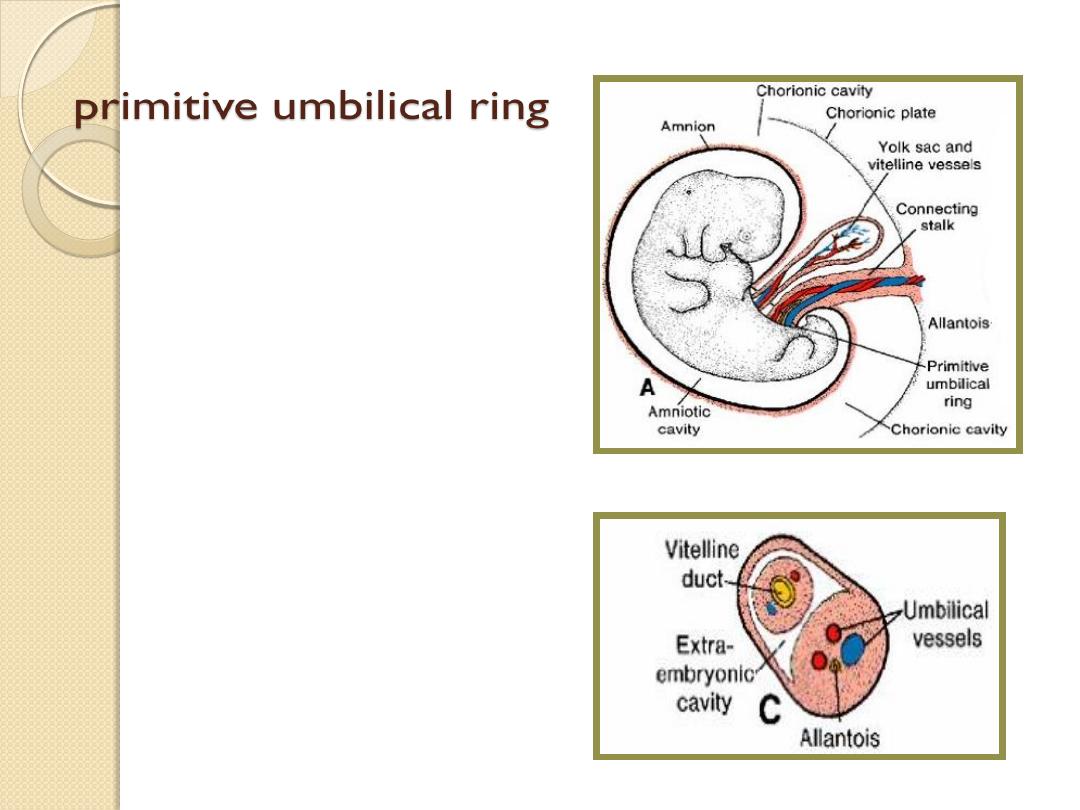
amnio–ectodermal junction
At the fifth week of
development, the following
structures pass through the
ring
(a) the connecting stalk, containing
the allantois and the umbilical
vessels, consisting of two arteries
and one vein;
(b) the yolk stalk (Vitelline duct),
accompanied by the vitelline
vessels
(c) the canal connecting the
intraembryonic and
extraembryonic cavities

The primitive umbilical cord
The amniotic cavity
enlarges rapidly at the
expense of the chorionic
cavity, and the amnion
begins to envelop the
connecting and yolk sac
stalks, crowding them
together and giving rise
to the primitive umbilical
cord .

The primitive umbilical cord
It contains
1.
the yolk sac stalk
2.
umbilical vessels.
3.
some intestinal loops
4.
the remnant of the allantois
When the allantosis and
vitelline duct and its vessels are
also obliterated , all that
remains in the cord are the
umblical vessels surrounded by
a jelly of wharton which
function as a protective layer
for the blood vessels

The Umbilical Cord
The attachment of the
umbilical cord to the
placenta is usually near
the center of the fetal
surface of this organ, but
it may attach at any point.

Marginal insertion
produces a battledore
placenta,

velamentous insertion
attachment of
umblical cord to the
fetal membranes

The umbilical cord is usually 1 to 2 cm in
diameter and 30 to 90 cm in length (average,
55 cm).
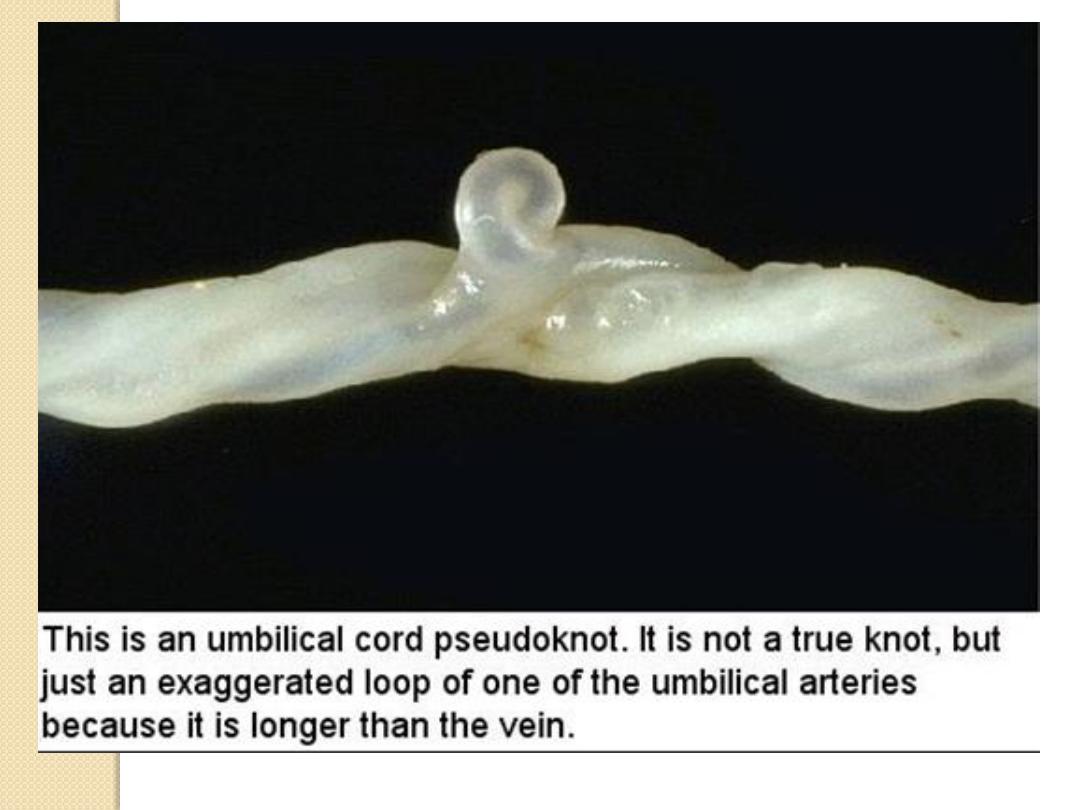
Because the umbilical vessels are longer
than the cord, twisting and bending of the
vessels(false knots) are common.
Excessively long or short cords are
uncommon. Long cords have a tendency to
prolapse and/or to coil around the fetus. A
very short cord may cause premature
separation of the placenta from the wall of
the uterus during delivery.



The umbilical cord usually has two arteries and one vein
that are surrounded by mucoid connective tissue (Wharton
jelly).

However a single
umblical artery is
present and these
babies have
approximately a
20%chance of having
cardiac and other
vascular defects

Fetal membranes
Thin layers or tissues which surround
the embryo or foetus and provide for its
nutrition, excretion and protection
They are :
A. amnion
B. yolk sac;
C. allantosis ;
D. chorion

Amniotic fluid (liquor amni)
Nature
Composition
Circulation of amniotic fluid
Function
During pregnancy
During labour

Clinical Correlates
Amniotic Fluid
Hydramnios or polyhydramnios
oligohydramnios
is the term used to
describe an excess of
amniotic fluid (1,500 to
2,000 mL).
Primary causes of
hydramnios include
1.
idiopathic causes
2.
maternal diabetes
3.
congenital malformations,
that prevent the infant
from swallowing the fluid
refers to a decreased
amount (less than 400 mL).
may result from renal
agenesis.
May cause
1.
club foot
2.
lung hypoplasia

Amniotic Bands
Occasionally,
tears in the amnion
result in amniotic bands that may encircle
part of the fetus, particularly the limbs and digits.
May result in
1.
Amputations
2.
ring constrictions ,and other abnormalities, including
3.
Craniofacial deformations
Origin of the bands is unknown

Premature rupture of the
membranes (PROM)
is the most common cause of preterm labor
occurs in 10% of pregnancies.
Unknown causes but risk factors include
1.
Previous pregnancies affected by
prematurity
2.
Black race
3.
Smoking
4.
Infections
5.
Severe polyhydramnios

Fetal Membranes in Twins
Arrangement of fetal membranes in twins ,
depending on the
a. type of twins
b. the time of separation of Monozygotic
twins.
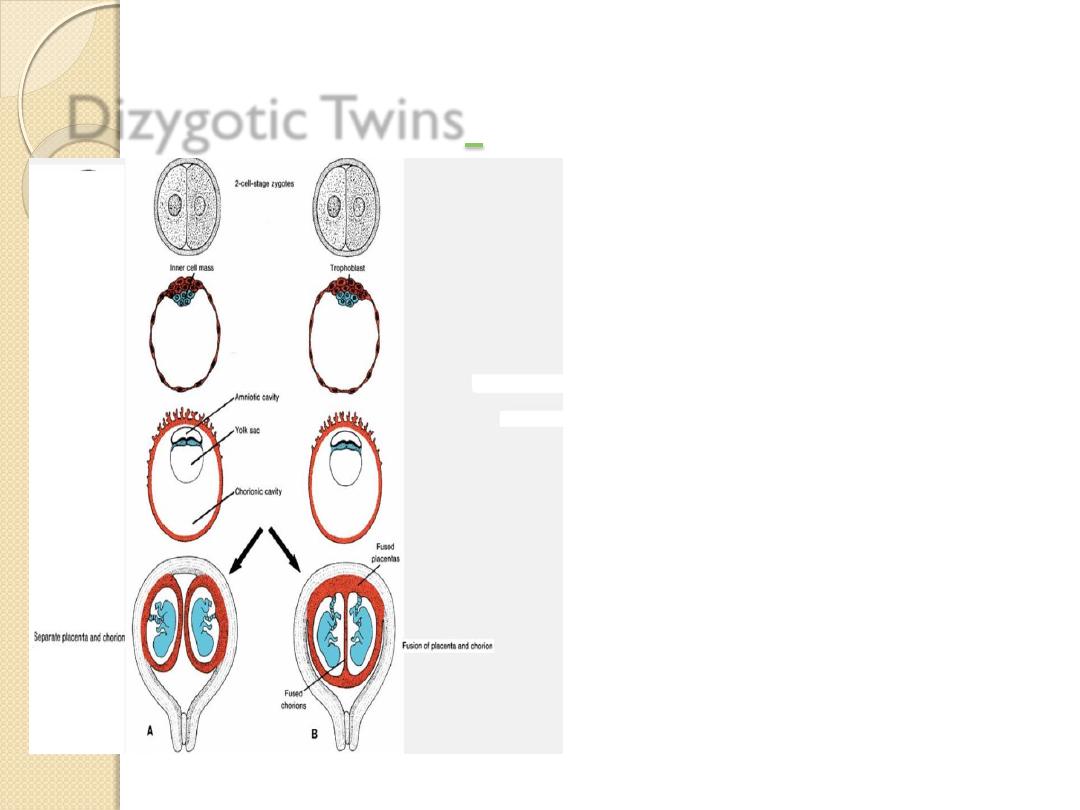
Dizygotic Twins
each embryo has its own
amnion
chorion
placenta
but sometimes the
placentas are fused.

Possible relations of fetal membranes in
monozygotic twins
A .Splitting occurs at the
two-cell stage,
each embryo has its own
placenta
amniotic cavity
chorionic cavity .

Possible relations of fetal membranes in
monozygotic twins
B .Splitting of the inner cell
mass into two completely
separated groups.
The two embryos have
a common placenta
a common chorionic sac
separate amniotic cavities

Possible relations of fetal membranes in
monozygotic twins
C .the separation occurs at the
bilaminar germ disc stage before
the appearance of the primitive
streak .
The embryos have
a common placenta
a common amniotic cavity
a common chorionic cavity .
In cases of conjoined twins, in
which the fetuses are not
entirely split from each other,
there is one amnion, one
chorion, and one placenta.

Thank you
