
Diseases of the appendix

• Anatomy: the vermiform appendix is present
only in humans, certain anthropoid apes and
wombat. It is blind muscular tube with
mucosal, submucosal , muscular and serosal
layers. Morphologically , it is underdeveloped
distal end of the large cecum found in many
lower animals.

• At birth, the appendix is short and broad at
its junction with the cecum, but differential
growth of the cecum produces the typical
tubular structure by about the age of two
years.

• During childhood , continued growth of the
cecum commonly rotates the appendix into
a retrocecal but intraperitonial position, in
approximately one quarter of cases rotation
of the appendix does not occur resulting in
pelvic, subcecal, or paracecal position.
Occasionally the or tip of the appendix
becomes extraperitoneal lying behind the
cecum or ascending colon . rarely the cecum
does not migrate during development to its
normal position in the right lower quadrant
of the abdomen.
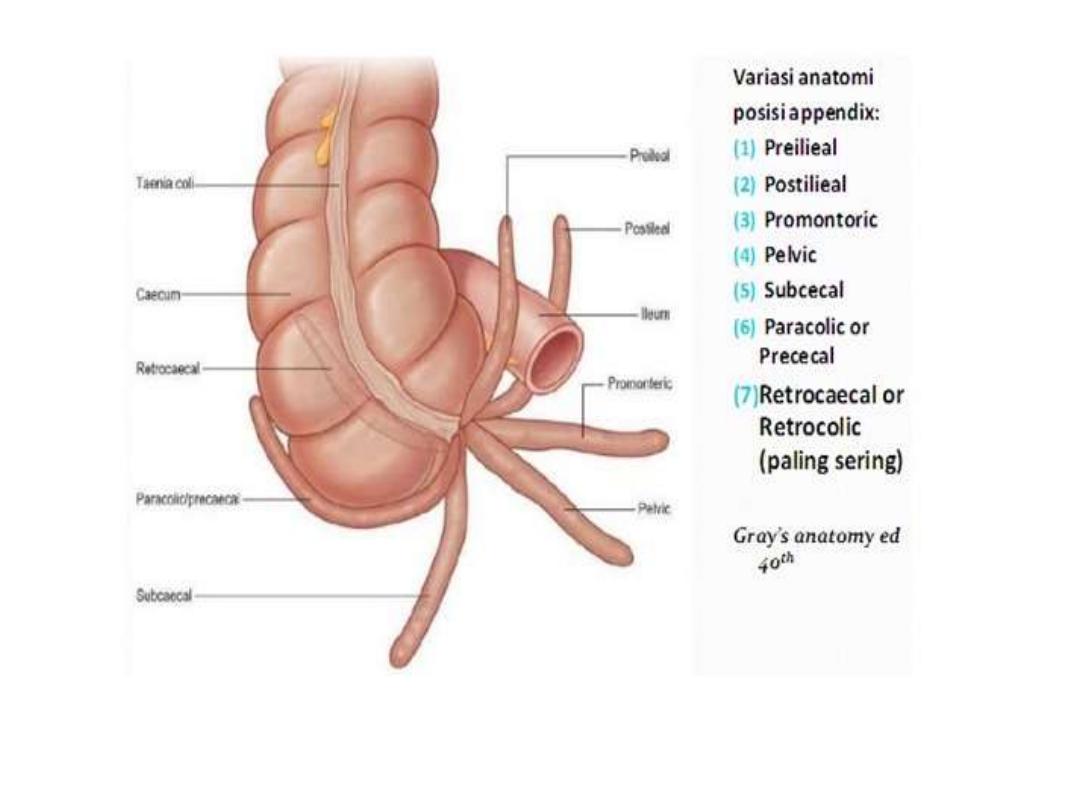
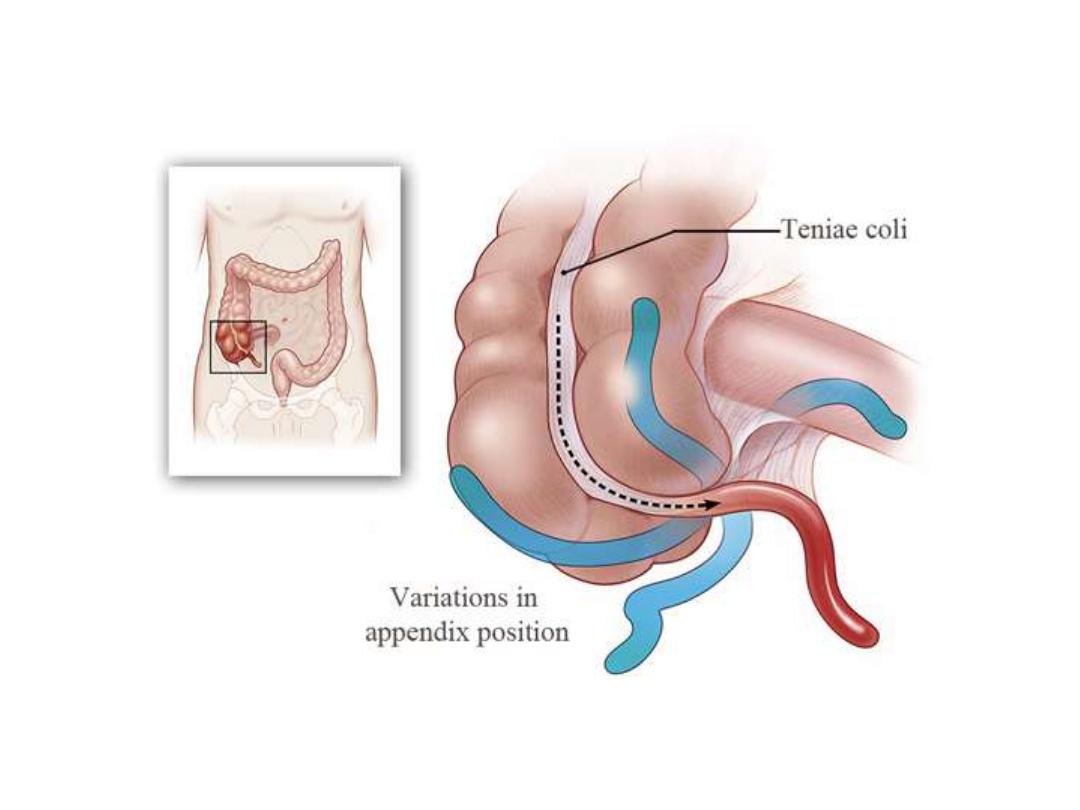

• In these circumstances the appendix can be
found near the gall bladder (subhepatic) or in
the case of intestinal rotation , in the left iliac
fossa, causing diagnostic difficulty if appendicitis
develops. the position of the base of the
appendix is constant, being found at the
confluence of the three taeniae coli of the
cecum, which fuse to form the outer
longitudinal muscle coat of the appendix. at
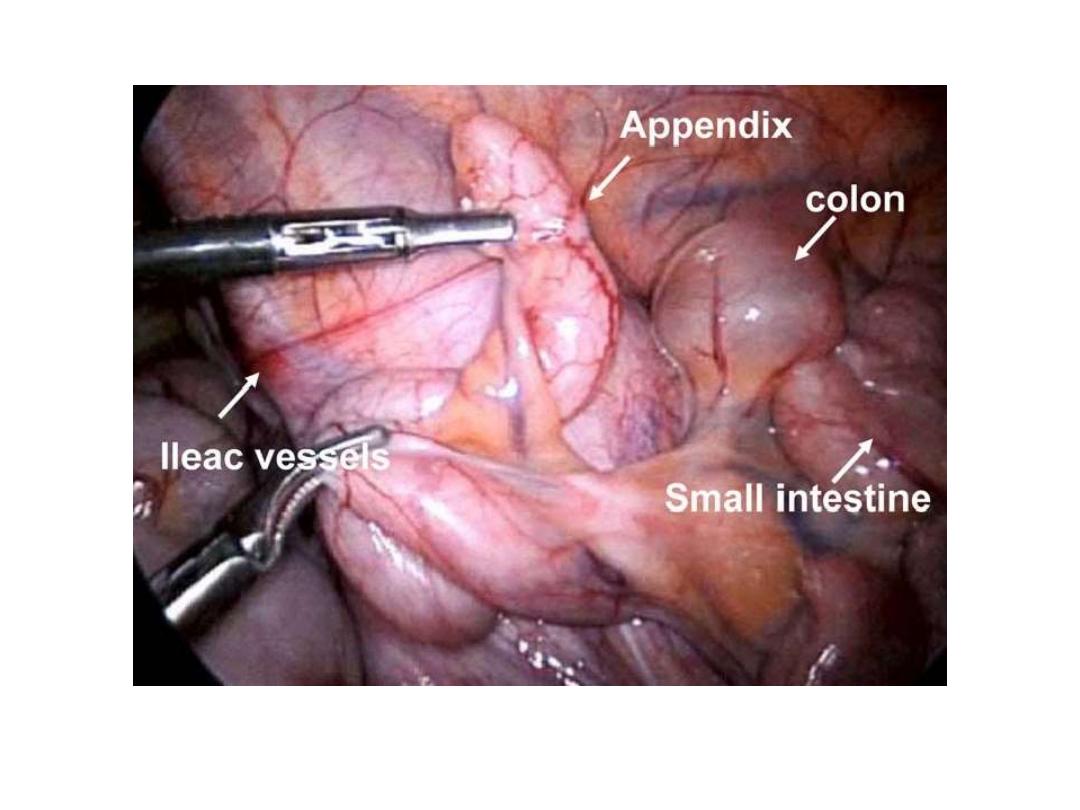
operation, use can be made of this to find an
elusive appendix, as gentle traction on the
taeniae coli, particularly the anterior taenia, will
lead the operator to the base of the appendix.

• The mesentery of the appendix or
mesoappendix arise from the lower surface
of the mesentery or the terminal ileum and
is itself subject to great variation. Sometimes
as much as the distal one third ofb the
appendix is bereft of mesoappendix.
Especially
in
the
childhood,
the
mesoappendix is so transparent that the
contained blood vessels can be seen . in
many adults, it becomes laden with fat,
which obscures these vessels.
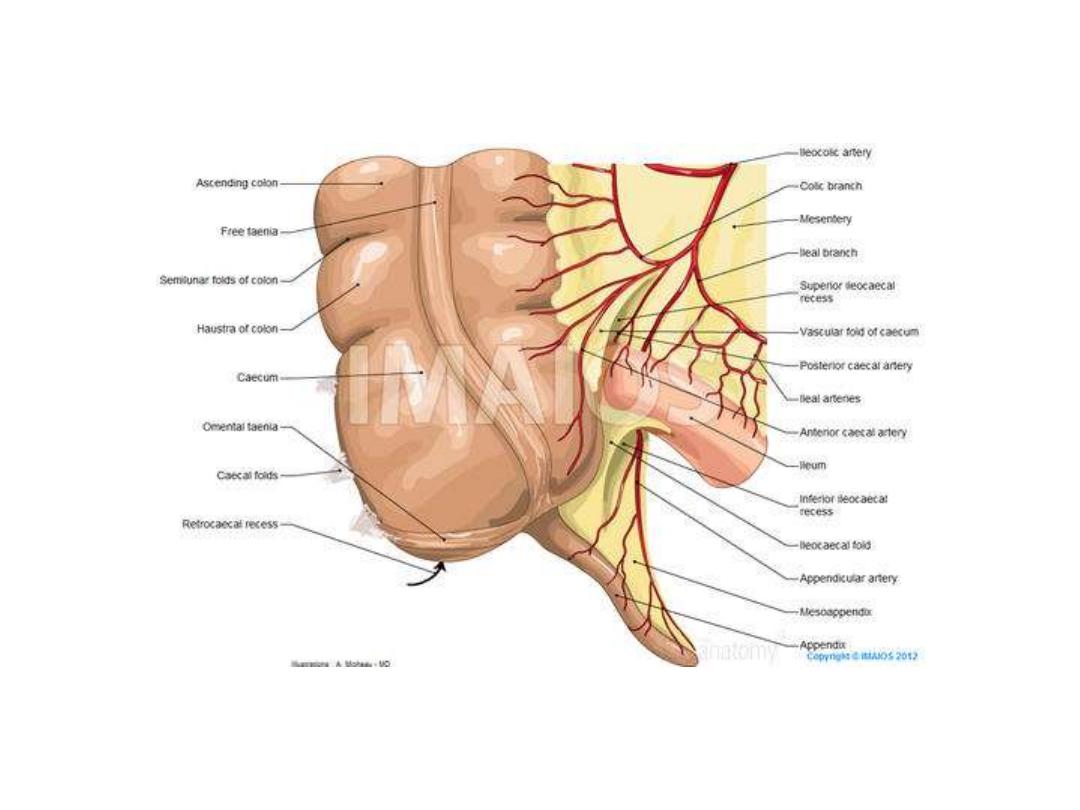

• The appendicular artery , a branch of the lower
division of the ileocolic artery , passes behind
the terminal ileum to enter the mesoappendix a
short distance from the base of the appendix. It
then comes to lie in the free border of the
mesoappendix. An accessory appendicular
artery may be present but in most people the
appendicular artery is an end artery, thrombosis
of which results in necrosis of the appendix as in
gangreneous appendicitis. Four, six of more
lymphatic channels traverse the mesoappendix
to empty into the ileocecal lymph nodes.

• Microscopic anatomy: the length of appendix
vary between average 7.5 cm and 10 cm. the
lumen is irregular folded of mucus membrane
lined by columnar cell intestinal mucosa of
colonic type. Crypts are present but are not
numerous. In the base of the crypts lies
argentaffin cells (kulchitsky cells), which may
give rise to carcinoid tumor. The submucosa
contains numerous lymphatic aggregation or
follicle but of no change in immune system
following appendicectomy, and it explain the
frequency of acute appendicitis in young adults.

• Acute appendicitis: it is the most common
surgical emergency in the world, and its
incidence is increased in the first half of this
century specially in Europe , America and
Australia with up to 16% of the population
undergoing appendicectomy. It is relatively
rare in infants and becomes increasingly
common in childhood and early adult life
reaching peak incidence in the teens and
early 20s.

• after middle age the risk of developing the
disease is quite small. The incidence is equal
in male and female before puberty. In
teenagers and young adults the ratio male to
female is increase to 3:2 at age of 25,
thereafter the incidence in male declines.

• Aetiology: no specific cause for acute
appendicitis but there are a lot of factors are
responsible, as low fiber diet and high
refined carbohydrates may share in etiology.
The incidence is decreased in western
countries due to good hygiene and change in
the pattern of gastrointestinal infection in
childhood related to increase in use of
antibiotics may be responsible.

• Appendicitis is usually associated with
bacterial proliferation with in the appendix ,
no single organism is responsible , mixed
growth of aerobic and anaerobic organisms is
usual.

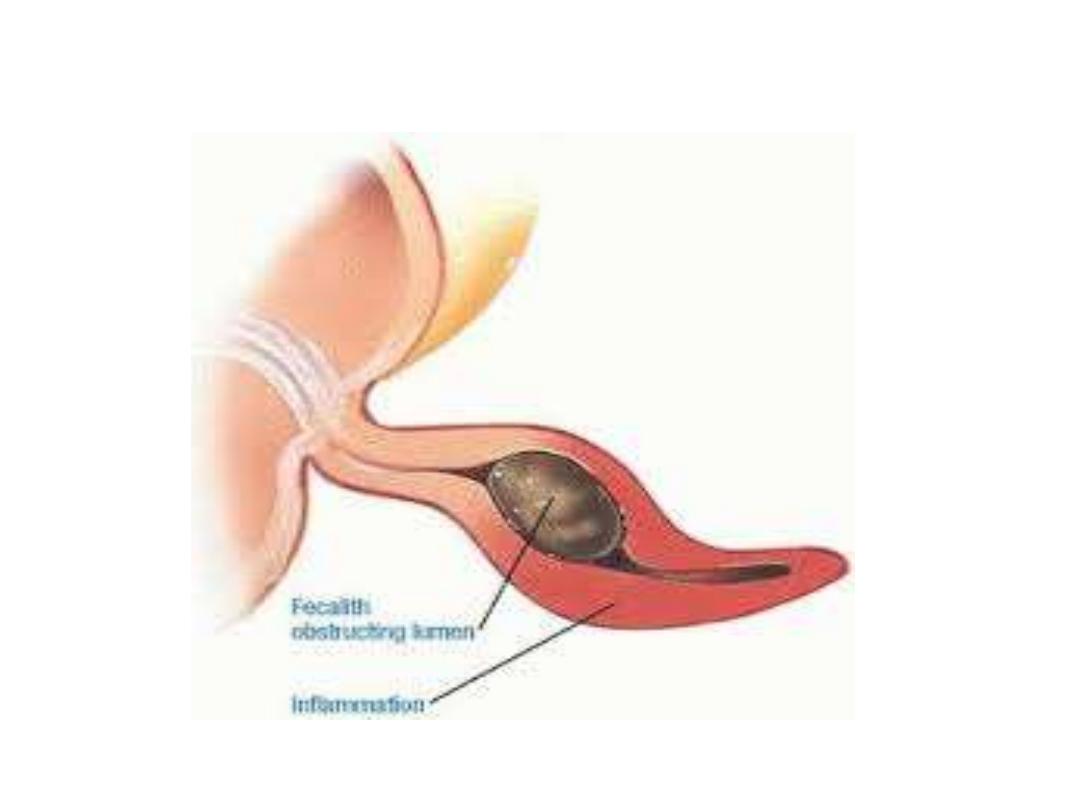
• The initiating point for proliferation of
bacteria is controversial. Obstruction of the
appendix lumen has been widely held to be
important, and some form of luminal
obstruction either by fecolith or stricture is
found in majority of cases. A fecolith is
composed of inspissated fecal material ,
calcium phosphate, bacteria and epithelial
debris, rarely foreign body is incorporated
into the mass. A presence of a fecolith is a
relative
indication
for
prophylactic
appendicectomy

• . A fibrotic stricture of the appendix is usually
indicate previous appendicitis that resolved
without surgical intervention. Obstruction of
appendicular orifice by tumors particularly
carcinoma of cecum is an occasional cause of
appendicitis in middle age or elderly patients.
Intestinal parasites particularly Oxyuris
vermicularis pin worm can proliferate in the
appendix and occlude the lumen


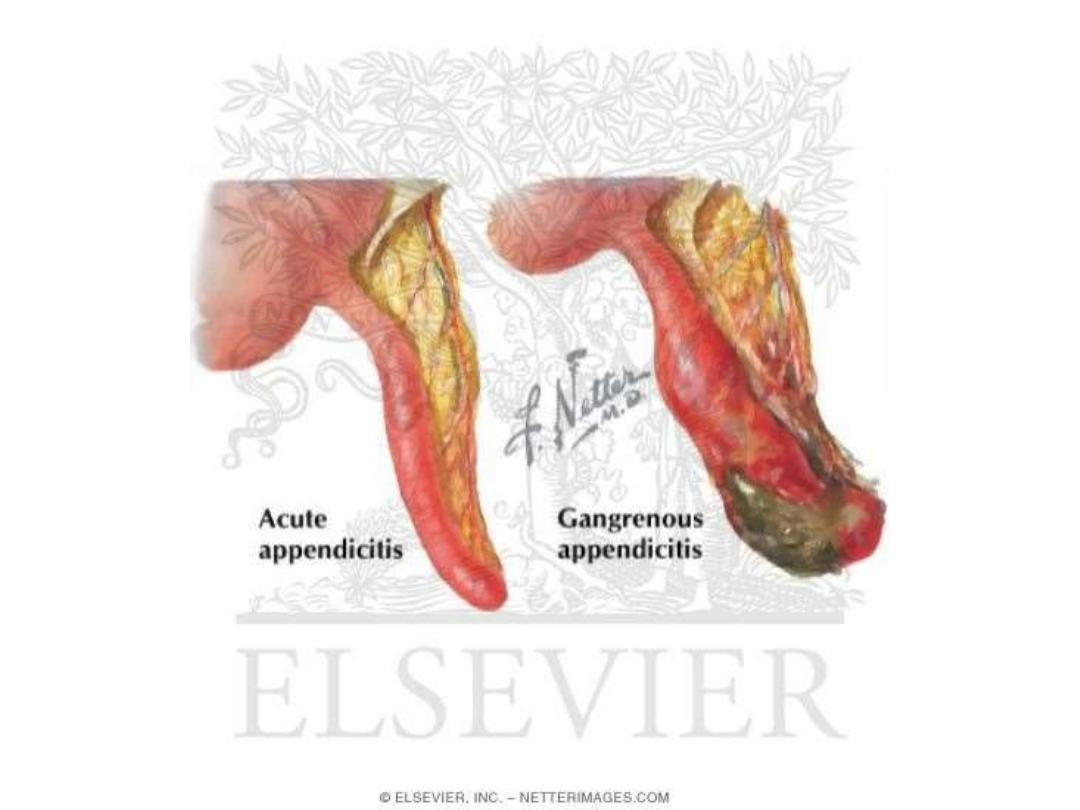
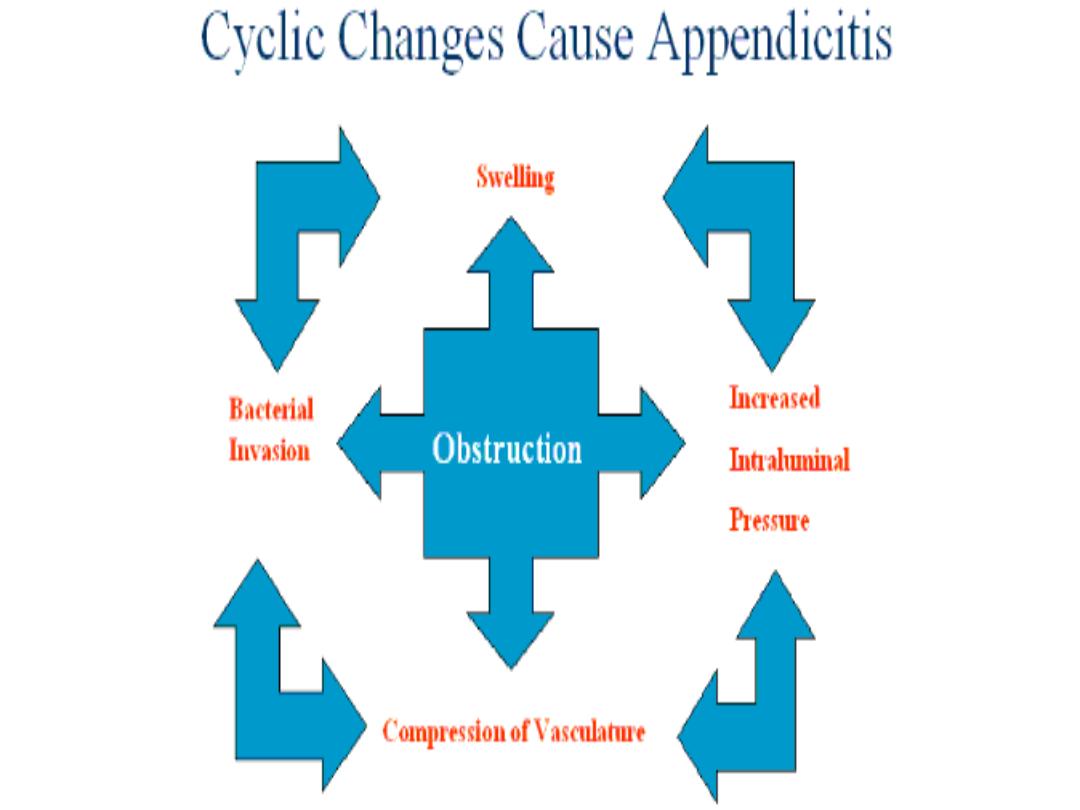
• Pathology: obstruction of the lumen seems to
be essential for development of appendicecal
gangrene and perforation . yet, in many cases
of early appendicitis, the appendix lumen is
patent despite the presence of mucosal
inflammation and lymphoid hyperplasia.
Viral infection can occurs in children with
seasonal variation more cases between May
and August in north Europe than other times
of the year.

• Lymphoid hyperplasia narrows the lumen of
the appendix leading to luminal obstruction ,
once obstruction occurs continued mucus
secretion and inflammatory exudate increase
intraluminal pressure obstructing lymphatic
drainage . edema and mucosal ulceration
develop with bacteria translocation to
submucosa. Resolution at this point may
occur either spontaneously or in response to
antibiotics therapy.

• . If the condition progresses further
distension of the appendix may cause venous
obstruction and ischemia of the appendicular
wall. With ischemia, bacterial invasion occurs
through the muscularis properia and
submucosa producing acute appendicitis,
with free contamination to peritoneal cavity..
• Alternatively, the greater omentum and loops
of small bowels becomes adherent to the
inflamed appendix , walling off the spread of
peritoneal contamination and resulting in a
phlegmonous mass or paracecal abscess.
Rarely appendicecal inflammation resolves ,
leaving a distended mucus-filled organ
termed a mucocele of the appendix

• Peritonitis is a bad complication of acute
appendicitis and to be as result of free
migration of bacteria through an ischemic
appendicular wall or from frank perforation
or gangrenous appendix or from delayed
perforation of appendicular abscess.

• Factors that may play a role in perforation
and peritonitis are extremes of age,
immunosuppression, diabetes and fecolith
obstruction of the appendix lumen, a free-
lying pelvic appendix and previous abdominal
surgery that limits the ability of the greater
omentum to wall off the spread of peritoneal
contamination. At this case a rapid
deteriorating clinical course is accompanied
by signs of diffuse peritonitis and systemic
sepsis syndrome called septic shock.

• clinical diagnosis:
• history: the classic features of acute
appendicitis begin with poorly localized
colicky abdominal pain. This is due to mid gut
visceral
discomfort
in
response
to
appendicecal inflammation and obstruction.
The pain is frequently first noticed in the
periumbilical region and is similar to, but less
intense than, the colic of small intestine
obstruction.
• Central abdominal pain is associated with
anorexia, nausea and usually one or two
episodes of vomiting that follow the onset of
pain. Anorexia is a useful a d constant clinical
feature , particularly in children. The patient
often gives a history of similar discomfort
that settled spontaneously.



• A family history is also useful as up to one
third of children with appendicitis have a first
degree relative with a similar history. With
the
progressive
inflammation
of
the
appendix , the parietal peritoneum in the
right iliac fossa becomes irritated, producing
more intense , constant and localized somatic
pain that begins to predominate. Patients
often report this as an abdominal pain that
has shifted and changed in character.

• Typically, coughing or sudden movement
exacerbates the right iliac fossa pain. The
classic visceral-somatic sequence of pain is
present in only about half of those patients
subsequently
proven
to
have
acute
appendicitis

• Atypical presentations include pain that is
predominately somatic or visceral and poorly
localized. Atypical pain is more common in
the elderly , in whom localization to the right
iliac fossa is unusual. An inflamed appendix
in the pelvis may never produce somatic pain
involving the anterior abdominal wall , but
may instead cause suprapubic discomfort and
tenesmus.

• In this circumstances, tenderness may be
elicited only on rectal examination and is the
basis for the recommendation that a rectal
examination should be performed on every
patient who presents with acute lower
abdominal pain.

• During the first 6 hours , there is rarely any
alteration in temperature or pulse rate. After
that time, slight pyrexia (37.2-37.7) with a
corresponding increase in the pulse rate to 80
or 90 is usual. However, in 20% of patients,
there is no pyrexia or tachycardia in the early
stages.

• In children, a temperature greater than 38.5c
suggests other causes, e.g. mesenteric
adenitis. Typically, two clinical syndromes of
acute appendicitis can be discerned, acute
catarrhal (non obstructive) appendicitis and
acute obstructive appendicitis.

• The latter is characterized by a much more
acute course. The onset of symptoms is
abrupt, and there may be generalized
abdominal pain from the start. The
temperature may be normal and vomiting is
common, so that the clinical picture may
mimic acute intestinal obstruction. Once
recognized, urgent surgical intervention is
required because of the more rapid
progression to perforation.

• Signs: the diagnosis of appendicitis rests
more on thorough clinical examination of the
abdomen than on any aspect of the history or
laboratory
investigations,
the
cardinal
features are those of an unwell patient with
low grade pyrexia, localized abdominal
tenderness, muscle guarding and rebound
tenderness.
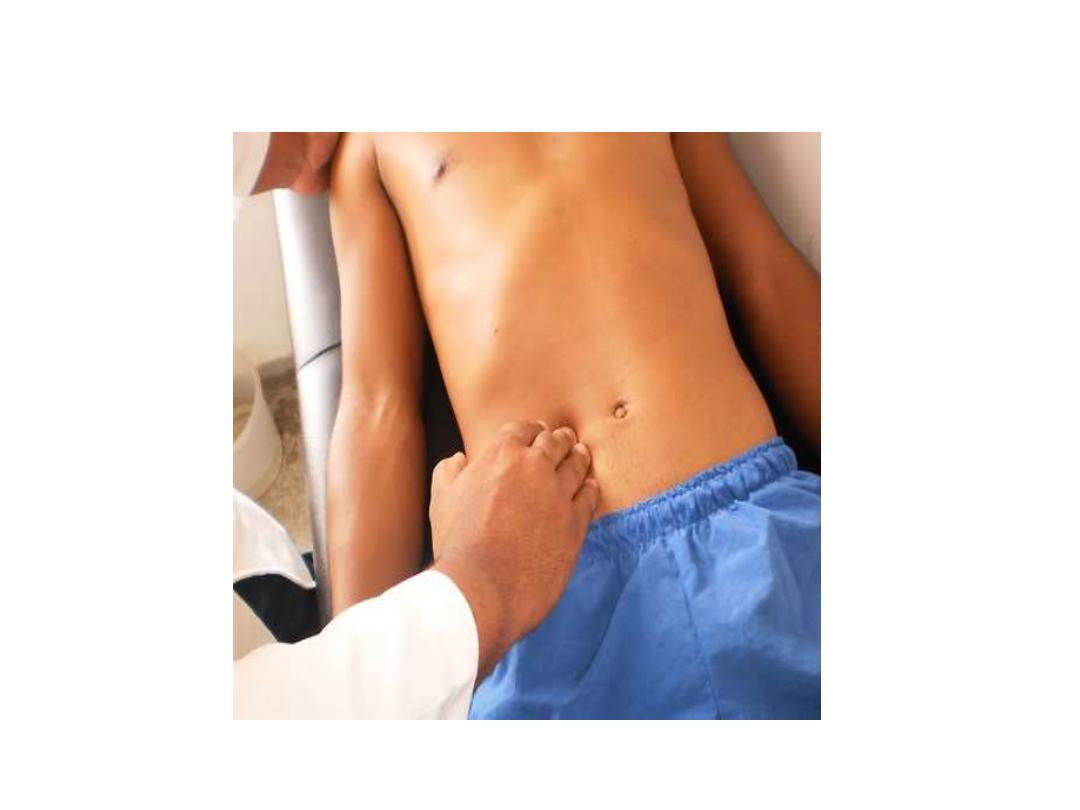

• Inspection of the abdomen may show
limitation of respiratory movement in the
lower abdomen. The patient is then asked to
where the pain began and where it moved
(pointing sign). Gentle superficial palpation
of the abdomen , beginning in the left iliac
fossa moving anticlockwise to right iliac fossa
will detect muscle guarding over the point of
maximum tenderness, classically Mc Burney's
point. Asking the patient to cough or gentle
percussion over the site of maximum
tenderness will elicit rebound tenderness.

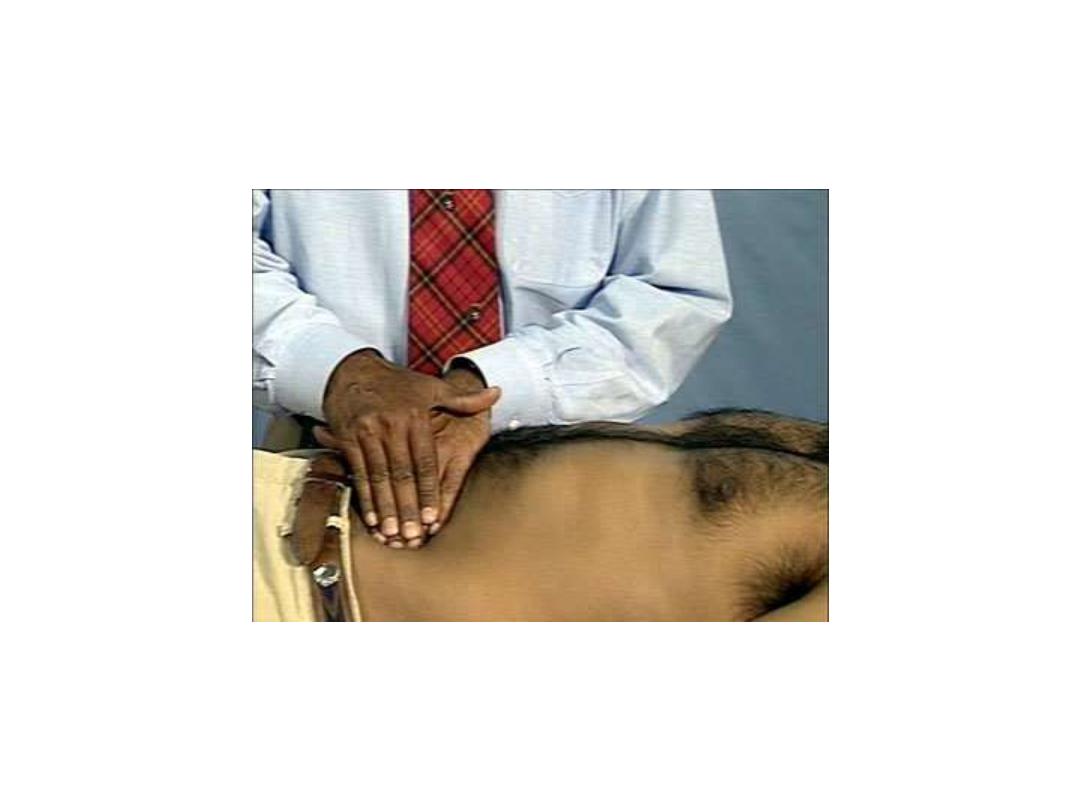
• Deep palpation in the left iliac fossa may
cause pain in the right iliac fossa called
Rovsing's sign which helpful in supporting a
clinical
diagnosis
of
appendicitis.
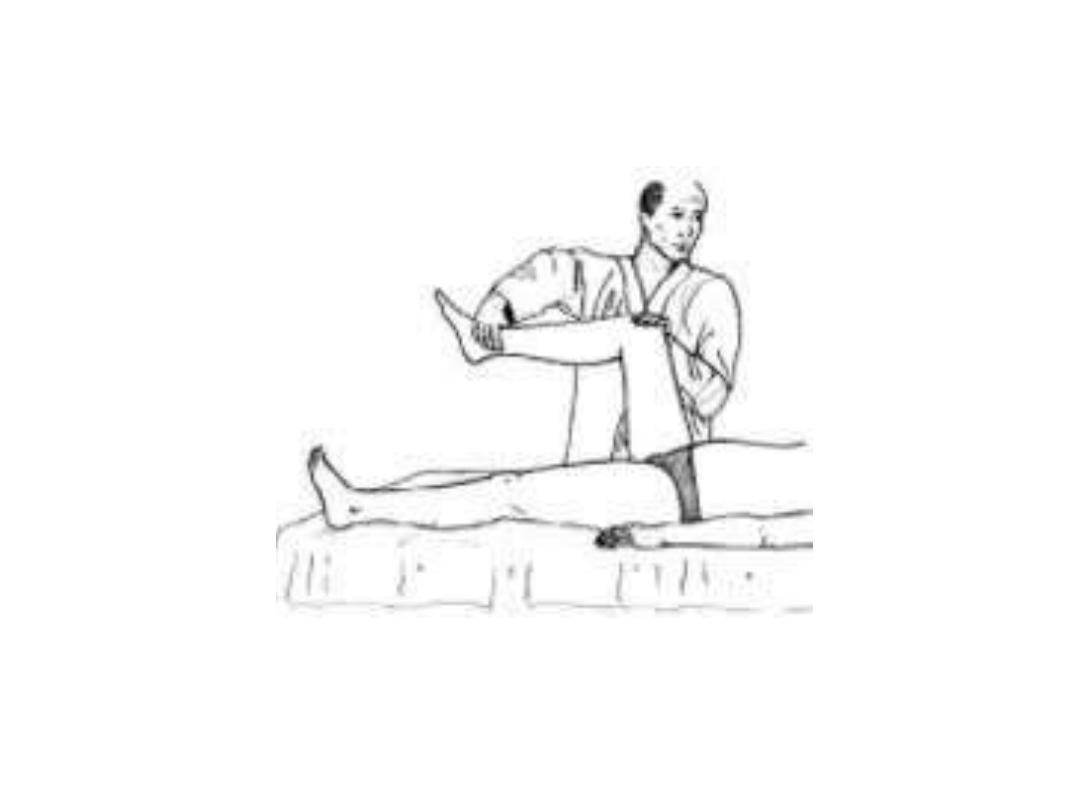
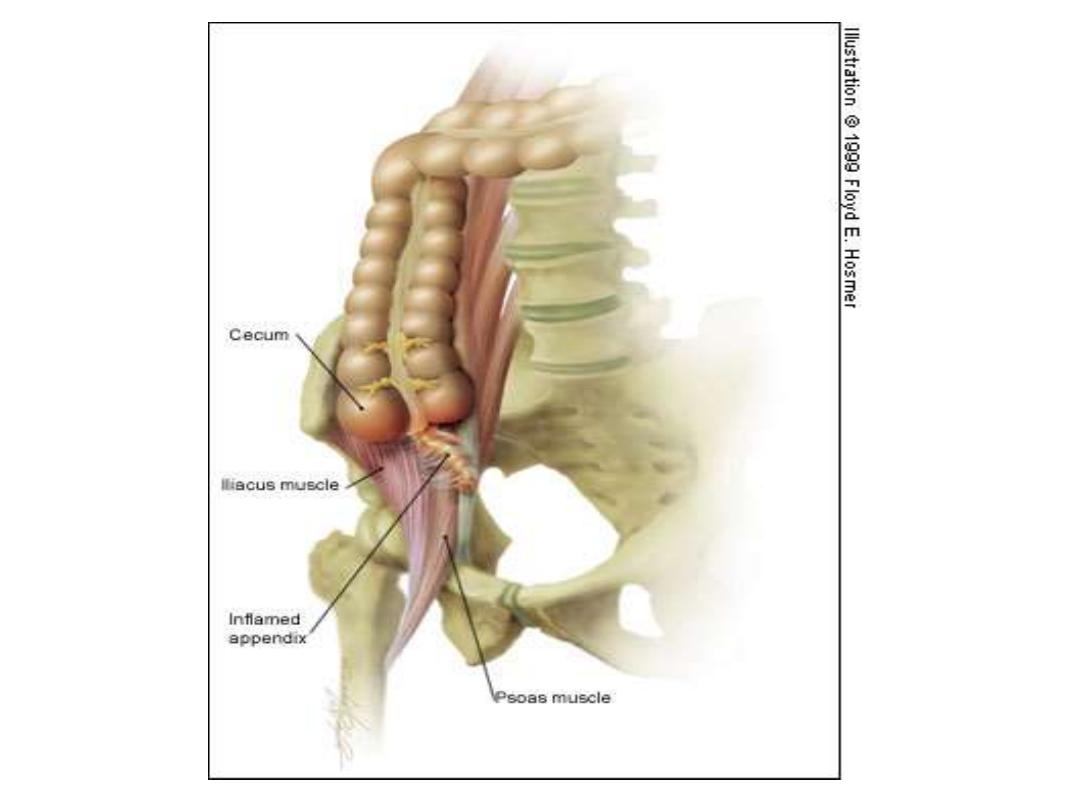
Occasionally, an inflamed appendix lies on
the psoas muscle, and the patient, often a
young adult will lie with the right hip flexed
for pain relief called psoas sign.

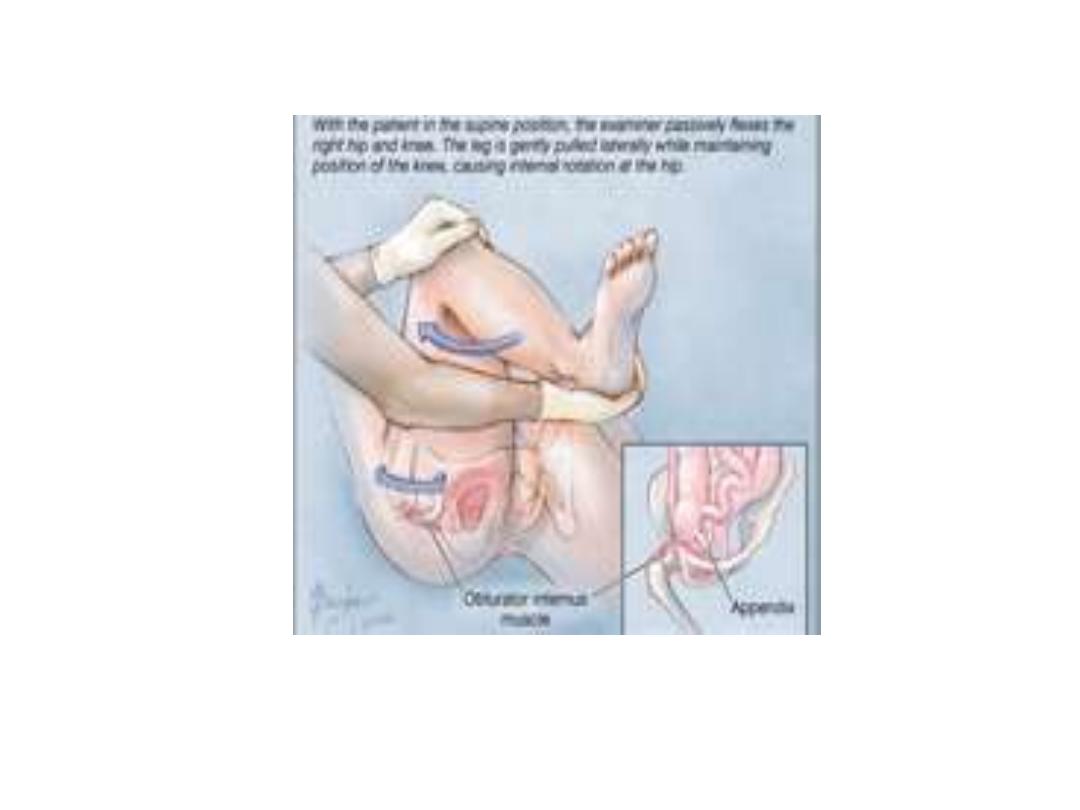
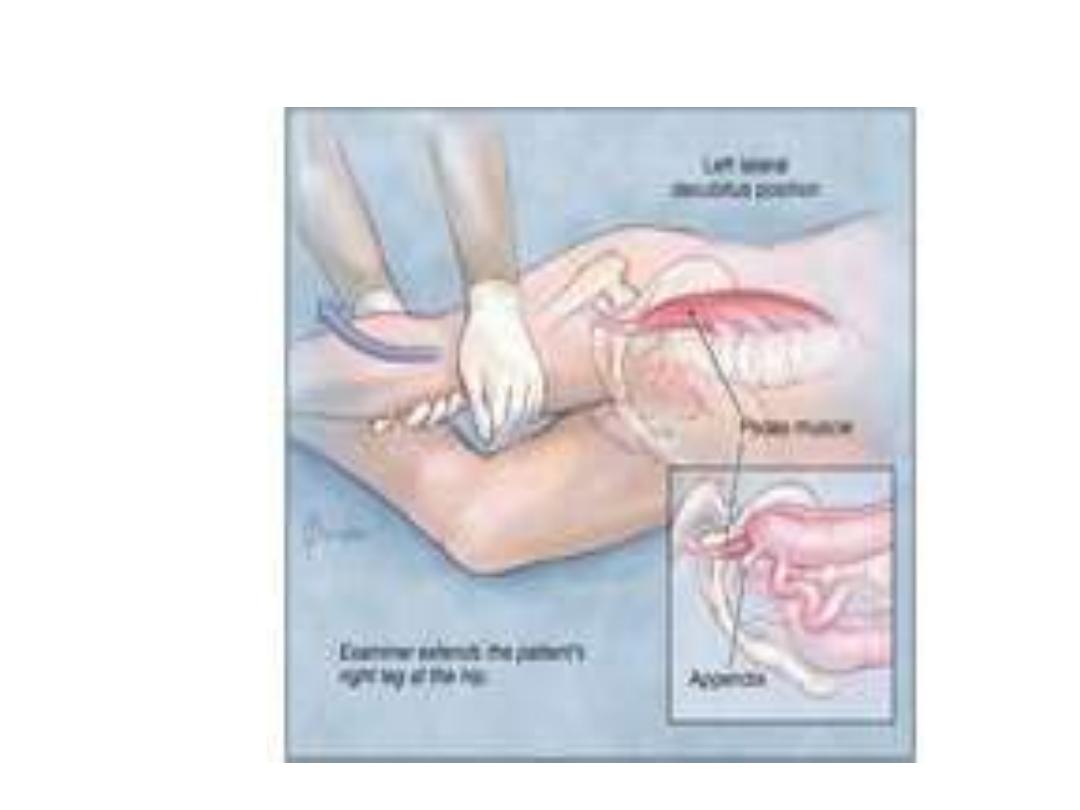
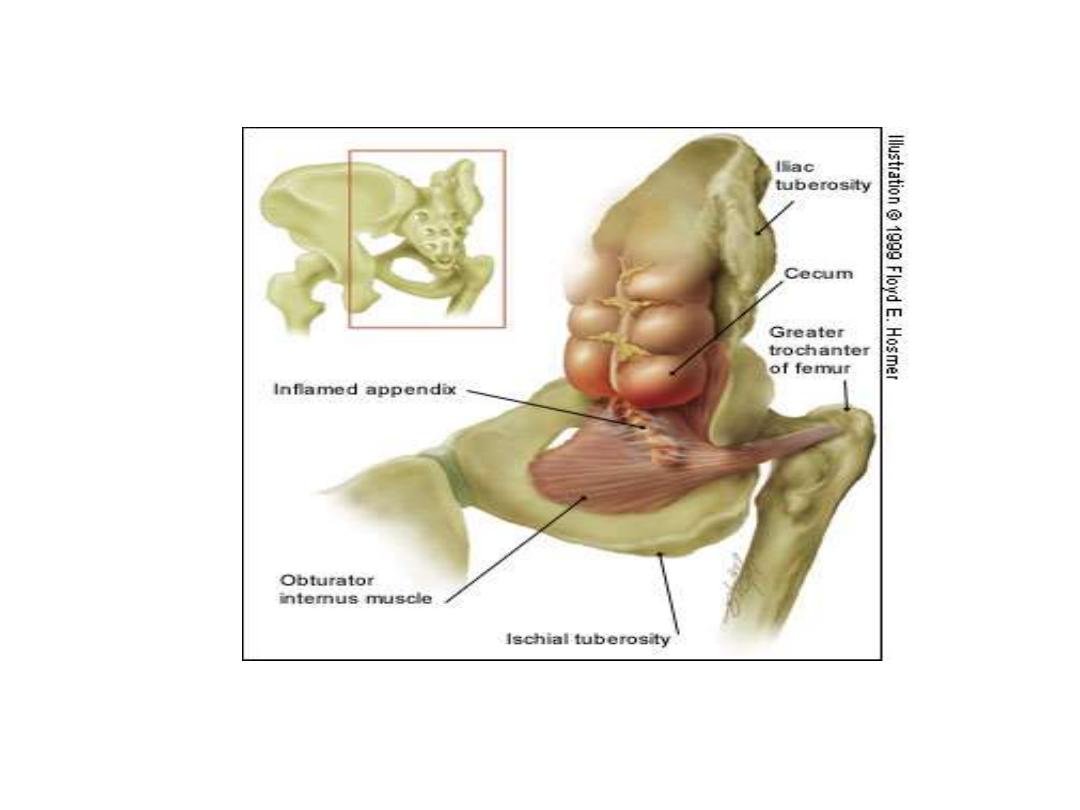
• Spasm of the obturator internus is sometimes
demonstrable when the hip is flexed and
internally rotated. If an inflamed appendix is in
contact
with
obturator
internus
,
the
manoveoure will cause pain in the hypogastrium
called obturator sign or Zachary Cope.
Cutaneous hyperesthesia may be demonstrable
in the right iliac fossa, but is rarely of diagnostic
value.
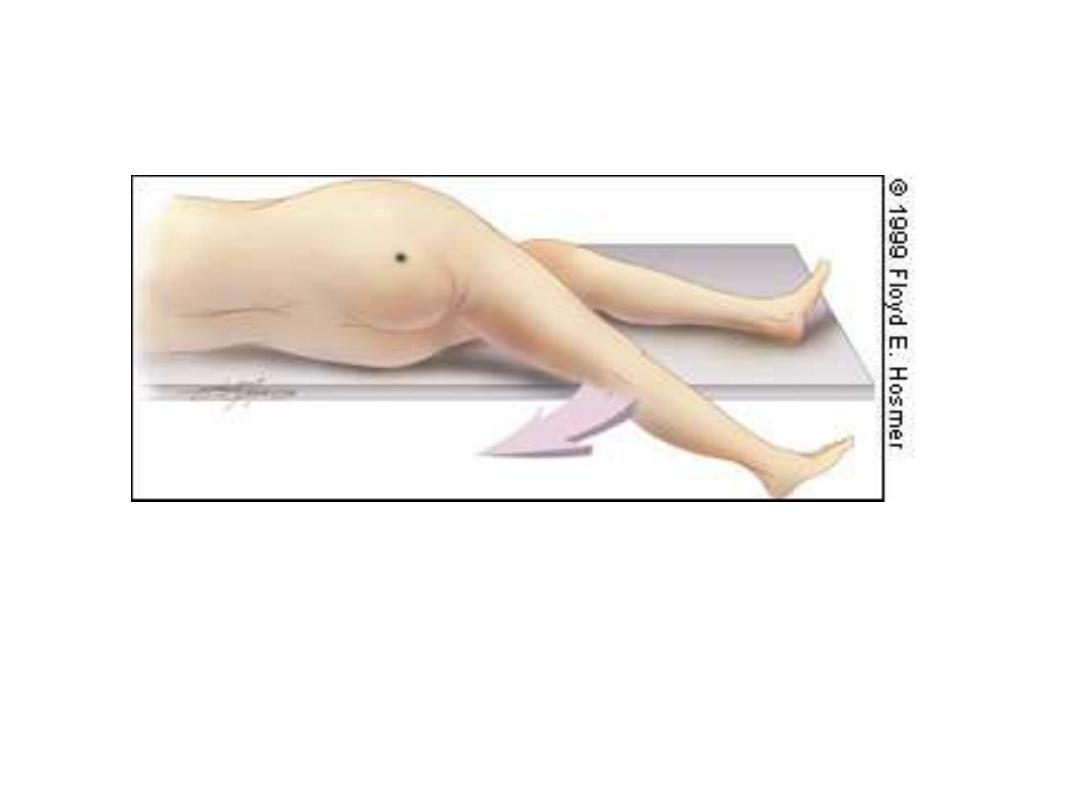
• Straight leg raising sign (digital pressure over
tender spot , elevation of right leg may cause
increase in pain)


• Special features according to position of the
appendix
• Retrocecal: called silent appendicitis , rigidity
is often absent and even application of deep
pressure may fail to elicit tenderness, the
reason being that the cecum ,distended with
gas, prevents the pressure exerted by the
hand from reaching the inflamed structure.
psoas sign is positive.

• Pelvic: diarrhea can be result when the
inflamed appendix be in contact with the
rectum, when the appendix is entirely within
the pelvis there is complete absence of
abdominal rigidity and also absence of
tenderness over Mc Burney's point. In some
cases there is tenderness above and to the
right of pubic symphysis.

• Rectal examination should be done reveals
tenderness at rectovesical pouch in male or
pouch of Douglas (rectouterine pouch) .
psoas and obturator signs are positive. If the
inflamed appendix is present in contact with
bladder, patient may has frequency of
micturition due to irritation of the bladder.

• Postilial: when the inflamed appendix lies
behind the terminal ileum, pain may not shift
and patient develop diarrhea.
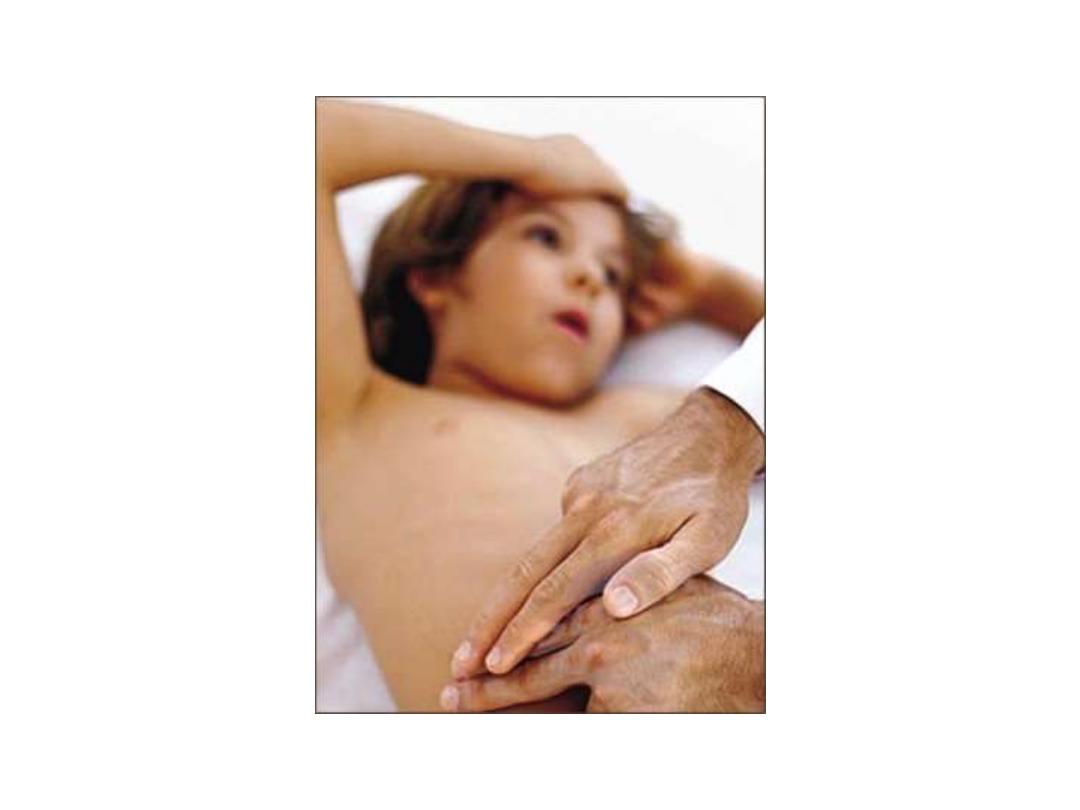
• Special features according to age: in infant
acute appendicitis is rarely before 36 months
of age so it is difficult to diagnose and will be
delayed so perforation might occurs and
diffuse peritonitis will soon be present
because of the underdeveloped greater
omentum which is unable to give much
assistance in localizing the infection.

• The elderly: gangrene and perforation occur
more frequently in elderly patients. Elderly
patients with lax abdominal wall or obesity
may harbor a gangrenous appendix with little
evidence of it and the picture may simulate
sub acute intestinal obstruction. These
features coupled with coincident medical
conditions produce a much higher mortality
for acute appendicitis in the elderly.

• The obese: obesity can obscure and diminish
all the local signs of acute appendicitis. Delay
in diagnosis coupled with technical
difficulties of operating in obese makes it
wiser to operate through a midline
abdominal
incision.
Laparoscopy
is
particularly useful in the obese as it may
obviate the need for a large abdominal
incision.

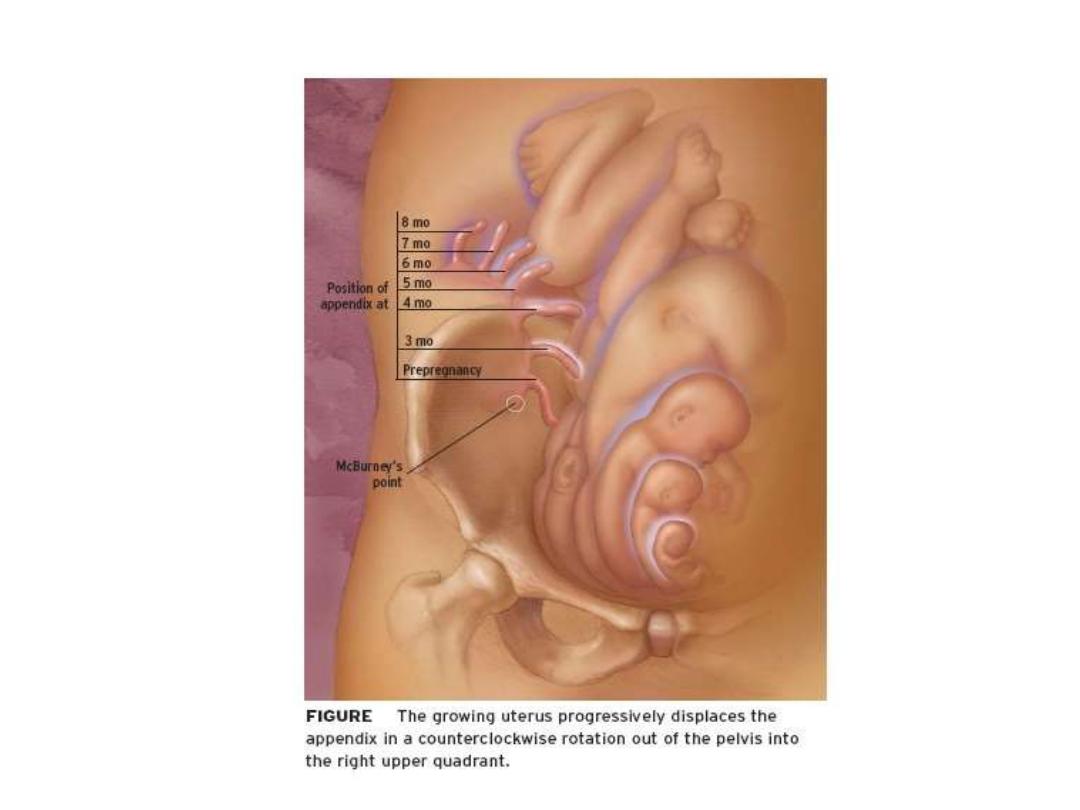
• Pregnancy: appendicitis is the commonest
extra uterine acute abdominal condition in
pregnancy with a frequency of 1:1500-2000
pregnancies. Diagnosis is complicated by
delay in presentation as early non specific
symptoms are often attributed to the
pregnancy. Usually the cecum and appendix
are progressively pushed to the right upper
quadrants the pregnancy develops during the
second or third trimesters.

• However pain at right lower quadrant of
abdomen remains the cardinal feature of
appendicitis in pregnancy. Fetal loss occurs in
3-5% of cases, increasing to 20% if
perforation Is found at operation.

• Differential diagnosis:
• In children: gastroenteritis, mesenteric adenitis,
Meckle's diverticulitis, intussusception, Henoch-
Scholen purpura, lobar pneumonia.
• In adult: regional enteritis, ureteric colic,
perforated peptic ulcer, torsion of the testis,
pancreatitis, rectus sheath hematoma.
• Adult
female:
Mittelsschmerz,
pelvic
inflammatory disease, pyelonephritis, ectopic
pregnancy, torsion or rupture of ovarian cyst,
endometeritis.
• Elderly: diverticulitis, intestinal obstruction,
colonic carcinoma, torsion appendix epiploicae,
mesenteric infarction, leaking aortic aneurysm.

• Investigations:
the
diagnosis
of
acute
appendicitis is essentially clinical. However a
decision to operate based on clinical suspicion
alone can lead to the removal of a normal
appendix in 15-30% of cases. To say it is better
to remove a normal appendix than to delay
diagnosis is not always fit specially in elderly
patient. A number of clinical and laboratory
based scoring systems have been devised to
assist diagnosis. The most widely used is the
Alvarado score . a score of 7 or more is strongly
predictive of acute appendicitis.

• Symptoms score
• Migratory right iliac fossa 1
• Anorexia 1
• Nausea and vomiting 1
• Signs
• Tenderness 2
• Rebound tenderness 1
• Elevated temperature 1
• Laboratory
• Leukocytosis 2
• Shift to left 1
• Total 10

• In patients with an equivocal score (5-6),
abdominal ultrasound or CT scan further
reduce the rate of –ve appendicectomy.
Ultrasound is useful in cases of gynecological
problems, and CT scan useful in elderly as has
diverticulitis
,neoplasm,
or
intestinal
obstruction.
• So full blood count, general urine
examination, ultrasound, CT scan, urea,
electrolyte all might be needed.

• Treatment:
the
treatment
of
acute
appendicitis is appendicectomy. Urgent
operation is essential to prevent the
increased morbidity and mortality of
peritonitis. It should no delay to operation
and I.V fluids should be given and I.V
antibiotics. Single injection of antibiotics
reduce postoperative wound infection. The
operation is done under general anesthesia
by conventional (open) or laparoscopic.

• The patient should be examined for any
presence of mass at right iliac fossa and
operation may postponed for conservative
treatment. The incision called grid-iron
incision which is perpendicular on Mc Burney
point which is in line joining between lateral
one third with medial two third from
umbilicus and anterior superior iliac spine.





• PROBLEMS
ENCONTERED
DURING
APPENDICECTOMY
• -If normal appendix is found, this needs
careful exclusion of other causes, ex terminal
ileitis, Mickel's diverticulitis, tubo-ovarian
diseases in women. It's usual to remove
appendix
to
avoid
future
diagnostic
difficulties even although the appendix is
macroscopically normal, particularly if a skin
crease or gridiron incision has been made.

• -If appendix can't be found, caecum should be
mobilized & taenia coli should be traced to their
confluence before the DX of "absent appendix"
is made.
• -If appendix tumor is found, small tumor less
than 2 cm can be removed by appendicectomy.
Larger tumor should be treated by Right
hemicoloectomy.
• -If appendix abscess is found& appendix can't be
removed easily, local peritoneal toilet, drainage
of abscess & IV antibiotic. Rarely caecectomy or
Right hemicoloectomy is required.

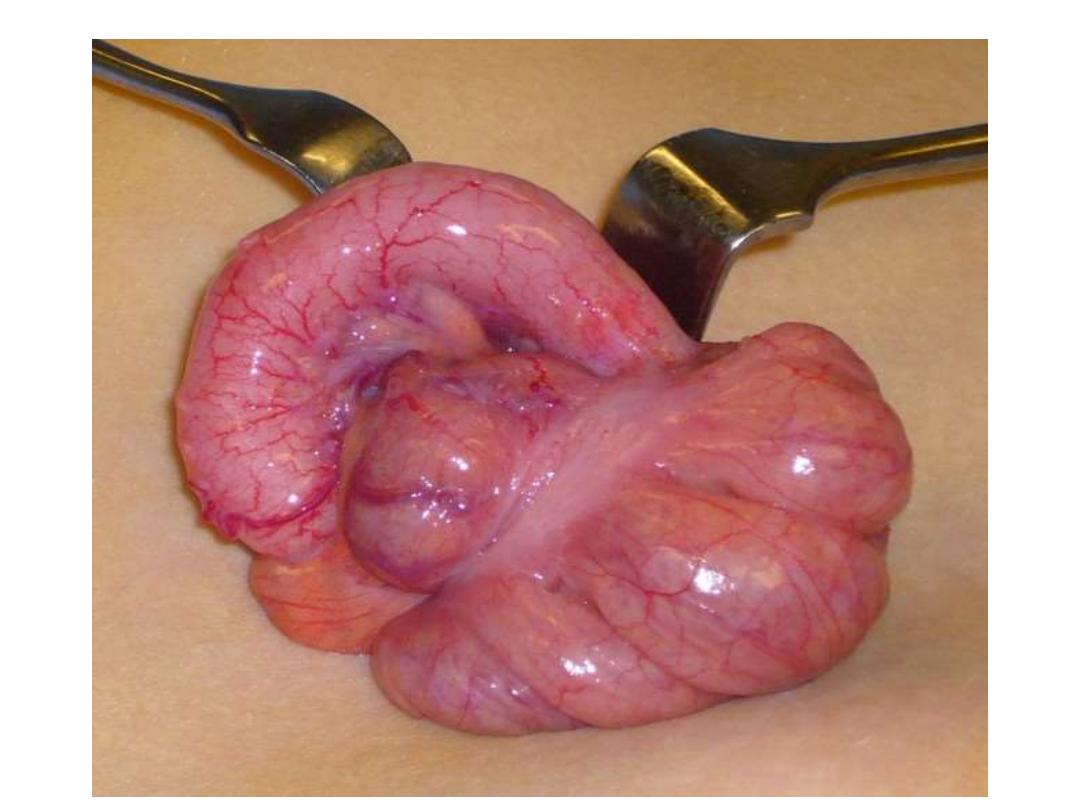
• Appendicular mass: if the operation is not
done, at fifth day appendicular mass may
appear, and can be felt in right iliac fossa
which compose of inflamed appendix.
Cecum, coils of loops bowel and greater
omentum, the standard treatment is the
conservative Ochsner-Sherren regimen. The
strategy is based on premise that the
inflammatory process is already localized and
that inadvertent surgery is difficult and may
be dangerous.

• It may be impossible to find appendix and
occasionally a fecal fistula may form. For
these reasons it is wise to observe a non-
operative programme but to be prepared to
operate when clinical deterioration occurs.
This regimen include recording the patient
condition carefully .

• it is helpful to mark the limits of the mass on
the abdomen using a skin pencil. CT scan
abdomen is done and I.V antibiotics by
metronidazole
and
third
generation
cephalosporin. If abscess is present should be
drained radiologically. Chart 4 hourly of pulse
,blood
pressure,
respiratory
rate,
temperature fluid input and amount of urine
output all should be recorded. Clinical
deterioration and evidence of peritonitis is an
indication of laparotomy.

• Clinical improvement is usually evident
within 24-48 hours. Failure of the mass to
resolve rise suspicion of carcinoma or Crohn's
disease. Using of this regimen 90% of the
cases resolve without incident. The great
majority of the patients will not develop
recurrence and it is no longer considered
advisable to remove the appendix after an
interval of 6-8 weeks.

•
• Conservative management includes:
• Admission of the patient to the hospital
• Nothing by mouth
• I.V. fluid therapy, daily requirement according to
the weight of patient
• Antibiotics therapy against aerobic and anaerobic
organisms
• Regular measurements of temperature and pulse
rate every 4 h.
• It’s helpful to mark the mass on the abdominal
wall using skin pencil
• A contrast-enhanced CT examination of the
abdomen should be performed

•
Criteria for improvement:
• Improvement of general condition of the
patient
• Improvement of appetite
• Decrease in the abdominal pain
• Decrease in temp. and pulse rate
• The mass decreased in its size and
tenderness.
•
It’s advisable to remove the appendix after
an interval of 6-8 weeks

• Criteria for stopping conservative treatment
• 1- a rising pulse 2- vomiting or copious gastric
aspirate 3- increasing or spreading of abdominal
pain 4- increasing the size of abscess. So these
factors indicates developing of appendicular
abscess needing urgent operation for drainage.
• Contraindications to delayed conservative
treatment
• 1- diagnosis is uncertain that it can not be
differentiating between acute appendicitis and
other abdominal condition that requiring
immediate operation as perforated peptic ulcer.

• 2- the signs indicates that inflammation is
still confined to the appendix.
• 3- patient is less than 10 years of age as early
perforation of appendix may occur due to
poor development of greater omentum to
localize the inflammation.
• 4- patient is above 60 years of age because
may has peritonitis with minimum clinical
signs due laxity of abdominal wall
musculature so he will not develop rigidity or
guarding of abdominal wall that indicate
peritonitis and early operation.

• Recurrent appendicitis: usually the patient
gives a history of previous abdominal pain
treated conservatively so he develops mild
recurrent attacks of mild abdominal pain and
dyspepsia and mild tenderness on right iliac
fossa, usually diagnosed as recurrent
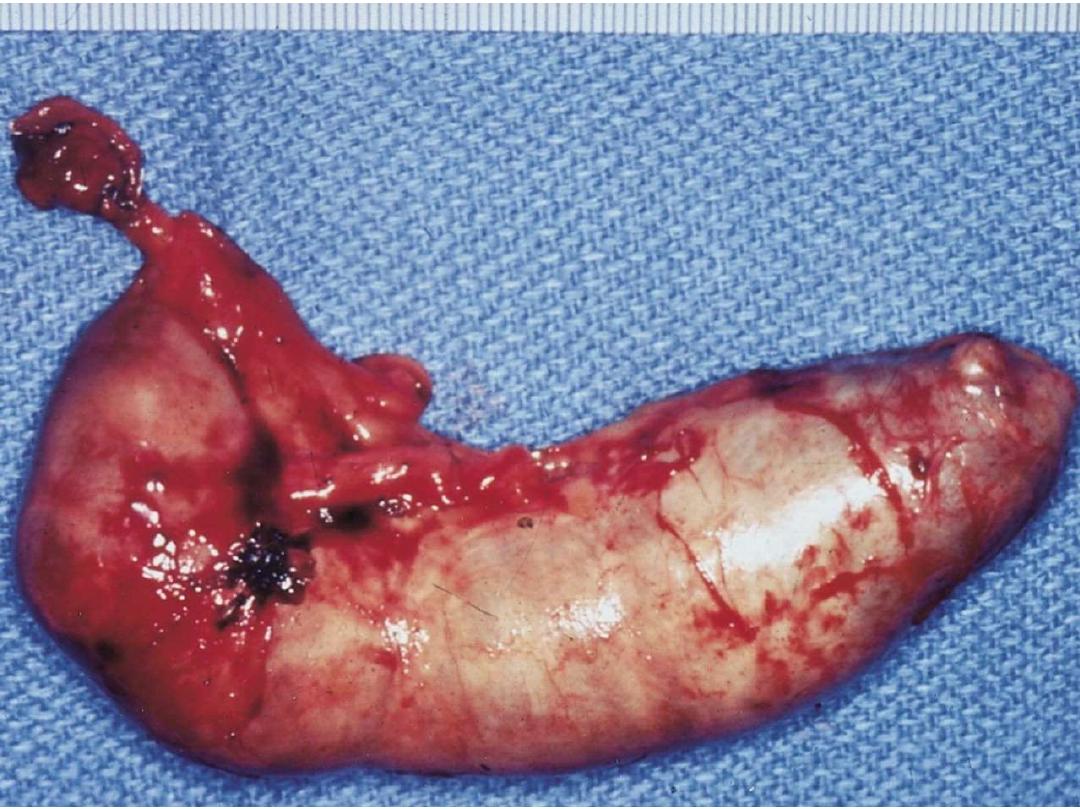
appendicitis and operation reveals that the
removed appendix has signs of chronicity as
fibrosis, short and kinking .
• Chronic appendicitis: it does not exist. Some
authors used this term, it usually example of
recurrent appendicitis.
• Post-operative complications:
• Early complications
• 1- Wound infection 2- intra-abdominal
abscess, residual abscess (local, pelvic,
paracolic, subphrenic) 3- paralytic ileus 4-
respiratory
atalactaxis
(lung
collapse),
pneumonitis 5-venous thrombosis and
embolism 6- portal pyemia (pyleophlebitis) 7-
fecal
fistula
8-
adhesive
intestinal
obstruction.

• Late complications
• 1- intestinal obstruction from fibrous
adhesion 2- incisional hernia 3- right inguinal
hernia following grid-iron incision especially
if the drain brought through the wound 4-
sterility in the female from frozen pelvis.

• Neoplasms of appendix
• Carcinoid tumor (argentaffinoma): it arise
from argentaffin tissue( Kulchitsky cells of the
crypts of Lieberkuhn)and most common in
appendix . it seen once in 300-400
appendices
sent
to
histopathological
examination and it is 10 times more common
than any other neoplasm present in
appendix. It usually present as acute
appendicitis , it felt hard and yellow in color
that it contain lipoid.

• it rarely metastases , and needs only
appendicectomy if it less than 2 cm , if it is
larger or has lymph nodes metastases or
involvement of cecal wall, a right
hemicoloctomy should be performed. The
cell of this tumor has special stain for
chromogranin. It usually occurs in female,
can appear at any age from 10-60 years. It
usually presents at distal third of the
appendix. Their metastases does not secrete
hormone to cause carcinoid syndrome as
flushness ,cyanosis and diarrhea.

• Primary adenocarcinoma: usually rare and of
colonic
type
and
treated
by
right
hemicoloectomy.
A
mucus
secreting
adenocarcinoma of the appendix may
rupture into peritoneal cavity, seeding it
inside , presentation is often delayed until
the patient develop a gross abdominal
distension as a result of pseudomyxoma
peritoneii, which may mimic ascites.
Treatment consists of radical resections of all
involved parietal peritoneal surfaces and
aggressive intraperitoneal chemotherapy.



• Less common conditions of the appendix:
• Mucocele of the appendix: may occur when e
proximal end of the lumen slowly becomes
completely occluded, usually by fibrous
stricture, and the secretions inside the lumen
remains sterile. The appendix is greatly enlarged
and contains mucin. When the mucin becomes
infected it changed to pyocele called empyema
by appendicectomy. One should be aware that
mucocele
is
not
a
mucus
secreting
adenocarcinoma as the treatment will be right
hemicoloectomy.

• Diverticulosis of the appendix: treatment is
appendicectomy.
• Endometriosis of the appendix: intensively rare and
bleeding per rectum occurs monthly with the
menstrual cycle as due to presence of endometrial
tissue in the appendix.
• Crohn's disease: fistula has been reported following
appendicectomy , usually there is Crohn's disease of
the cecum reaching to the base of the appendix , at
this situation appendicectomy should not be
performed.
• Intussusception of the appendix: usually in childhood
, as appendiculo-colic intussusception or part of ileo-
cecal intussusception , treatment by release of
intussusception with appendicectomy.
