Epidemiology, prevention & control ofMeningococcal meningitis
Dr. Nadia AzizF.A.B.C.M , Lecturer
community medicine department
1-Define what is meningitis
2-Types of meningitis3-Identification of meningococcal meningitis, the diagnosis, its occurrence & ways of controlling this disease.
OBJECTIVES
Is an inflammatory process of liptomeninges and the CSFMeningitis
1- Acute pyogenic (bacterial) meningitis
2-Acute aseptic (viral) meningitis3-Acute focal suppurative infection (brain abscess, subdural and extradural empyema)
4- Chronic bacterial infection (tuberculosis)
Classification
1- Neisseria meningitidis
2- Streptococcus pneumoniae and3- Haemophilus influenzae type b (Hib)
Constitute more than 75% of all cases of bacterial meningitis in most studies, and 90% of bacterial meningitis occur in children.
MENINGOCOCCAL MENINGITIS ICD-10 A39.0
An acute bacterial disease, characterized by:Sudden onset of fever
intense headache
nausea and vomiting
stiff neck and photophobia
A petechial rash with pink macules may be observed.
Identification
With antibiotics, intensive care units and improved supportive measures have decreased but it remains high at 8%–15%.
long-term sequelae :
10 –20% of survivors will suffer mental retardation, hearing loss and loss of limb use.
Case fatality rate
• 1- Meningitis (the most common presentation)• 2- Bacteremia and
• 3- Sepsis
Clinical syndromes
Meningococcaemia is the most severe form of infection with petechial rash, hypotension, disseminated intravascular coagulation and multiorgan failure.Other forms of meningococcal disease such as pneumonia, purulent arthritis, and
pericarditis are less common.
Clinical syndromes
• 1-CSF or blood culture: Isolation of meningococci from a sterile site CSF or blood (gold standard). The sensitivity of culture, especially in patients who have received antibiotics, is low.2-Latex agglutination test: Identification of group-specific meningococcal polysaccharides in CSF by latex agglutination in culture-negative cases
Diagnosis
• 3-Polymerase chain reaction: detecting meningococcal DNA in CSF or plasma and not requiring live organisms is of help but false-negative results are common.
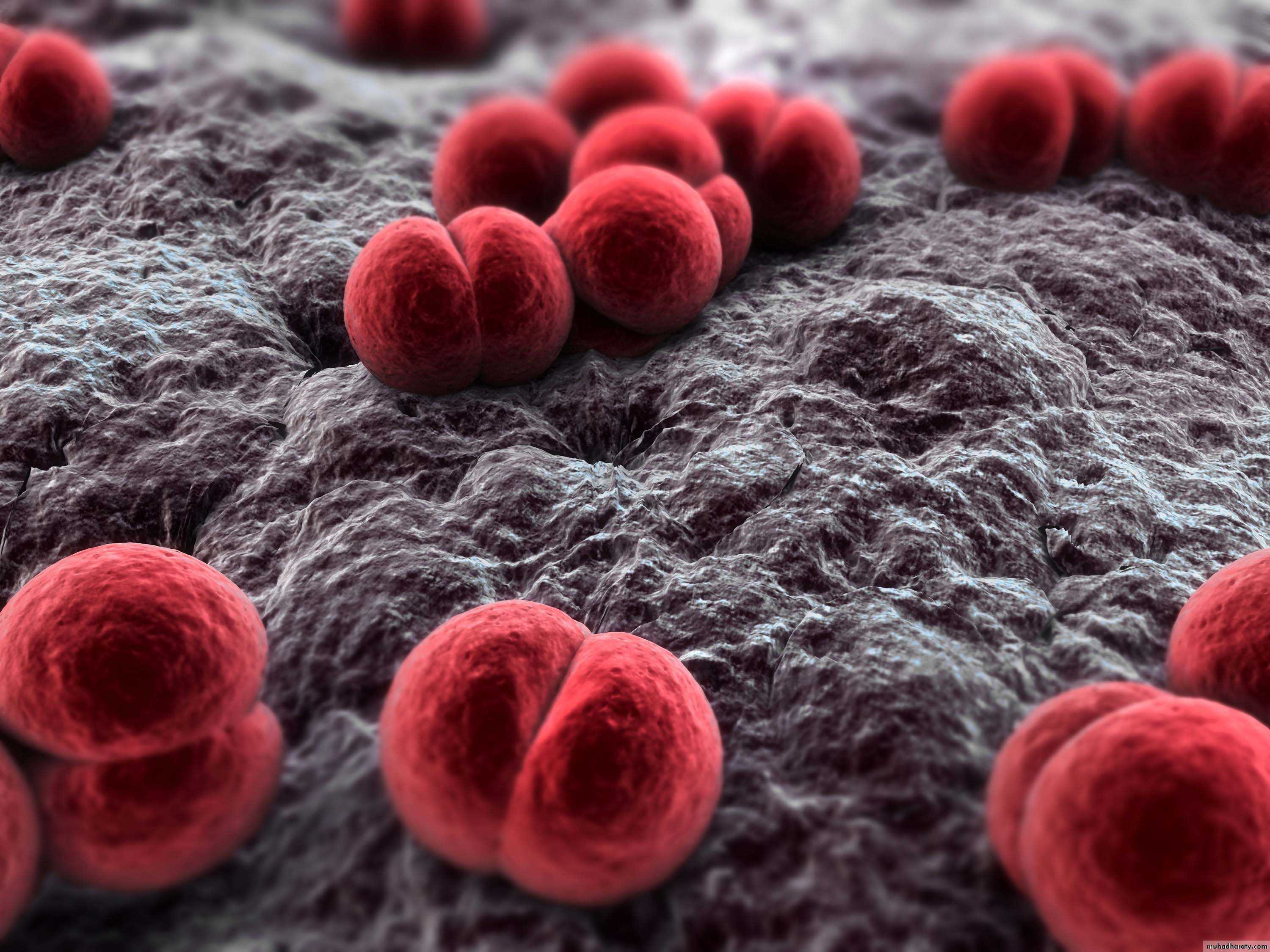
• 4-Gram-stained smears from petechiae: may show Neisseria.
Diagnosis
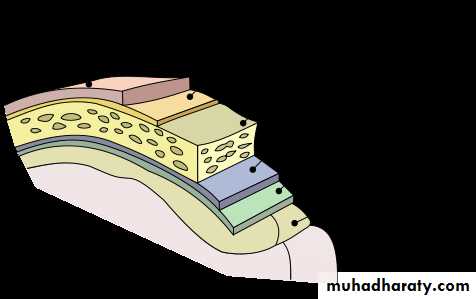
Neisseria meningitidis, the meningococcus, is a Gram-negative, aerobic diplococcus. Neisseria are divided into serogroups according to their capsular polysaccharide. Group A, B, and C organisms account for at least 90% of cases, although the proportion of groups Y and W135 and X is increasing in several regions.Infectious agent
In Europe and North America the incidence of meningococcal disease is higher during winter and spring
In Sub-Saharan Africa (African meningitis belt) the disease classically peaks during the dry season
Occurrence
Infants have the highest risk of meningococcal disease.
Rates of disease decrease after infancy and then increase in adolescence and young adulthood.Occurrence
In addition to age, other risk factors include underlying immune deficiencies, such as asplenia, properdin deficiency.
Crowding, low socioeconomic status, active or passive exposure to tobacco smoke and concurrent upper respiratory tract infections In some countries males are at higher risk than females
Occurrence
Reservoir: Humans.Mode of transmission
Direct contact, including respiratory droplets from nose and throat of infected people
Up to 5%–10% of people may be asymptomatic carriers with nasopharyngeal colonization by N. meningitidis.
MENINGOCOCCAL MENINGITIS
2 to 10 days, commonly 3–4 days.Incubation period
Until live meningococci are no longer present in discharges from nose and mouth. Meningococci usually disappear from the nasopharynx within 24 hours after institution of antimicrobial treatment to which the organisms are sensitive.Period of communicability
Susceptibility to the clinical disease is low and decreases with age; this induces a high ratio of carriers to cases.Persons deficient in certain complement components are especially prone to recurrent disease; splenectomized persons are susceptible to bacteraemic illness.
Susceptibility
A. Preventive measures
1) Educate the public on the need to reduce direct contact and exposure to droplet infection.2) Reduce overcrowding in living quarters and workplaces, barracks, schools and ships.
3) Vaccines containing groups A, C, Y and W-135 meningococcal polysaccharides are been available
Methods of control
Two polysaccharide vaccines:1- Quadrivalent ACYW-135 vaccine
2- Bivalent AC Polysaccharide meningococcal vaccines against serogroups A and C are safe and effective in adults and children over 2, but do not elicit long-term protection.
Vaccines
Vaccines are effective for:1- outbreak control
2- prevention among high-risk groups, such as travellers to countries where disease is epidemic, Hajj pilgrims, military groups, and individuals with underlying immune dysfunctions.
Vaccines
Because these vaccines are often poorly immunogenic in young children and have limited duration of efficacy, they are not
generally used in routine childhood immunization programs.
Vaccines
1) Isolation: Respiratory isolation for 24 hours after start of treatment.
2) Protection of contacts: Close surveillance of household, daycare, and other intimate contacts for early signs of illness, to initiate appropriate therapy without delayprophylactic administration of chemotherapeutic agent to intimate contacts
B. Control of patient, contacts and the immediate environment
Younger children in day care centers, even if not close friends, should all be given prophylaxis after an index case is identified
Prophylaxis
1- Rifampicin
Twice daily for 2 days: adults 600 mg per dose; children over 1month old, 10 mg/kg2- Ceftriaxone
For adults, 250 mg IM, given in a single dose, 125 mg IM for children under 15.
3- Ciprofloxacin
500 mg PO, a single dose to adults.
Prophylaxis
Penicillin given parenterally in adequate doses is the drug of choice
Ampicillin and chloramphenicol are also effective.Ceftriaxone
Ciprofloxacin
Treatment
Penicillin-resistant strains have been reported in many countries,strains resistant to chloramphenicol also have been reported.
Treatment should start as soon as the presumptive clinical diagnosis is made, even before menin-gococci have been identified.
Treatment
In children, until the specific agent has been identified, the drug chosen must be effective against Haemophilus influenzae type b (Hib) as well as Streptococcus pneumoniae.Treatment
1) When an outbreak occurs, major emphasis must be placed on:Careful surveillance, early diagnosis and immediate treatment of suspected cases.
Thresholds (alert and epidemic)
When thresholds are passed, immunization campaigns must be implemented.
C. Epidemic measures
1) setting up an epidemic management committee,
enhancing surveillance, undertaking field epidemiology andbacteriological investigations, ensuring supplies of drugs and laboratory material
mass vaccination
Specific actions at the epidemic
2) Reduce overcrowding and ventilate living and sleeping quarters3) Intimate contacts should all be considered for prophylaxis
Specific actions at the epidemic4) The use of vaccine in all age groups affected is strongly recommended if an outbreak occurs in a large institutional
or community setting
Specific actions at the epidemic
Thank you&
Good luck