Prenatal Diagnosis of Congenital and Genetic Diseases
Dr. Najmah MahmoodAim of Prenatal Diagnosis
The aim of prenatal diagnosis relate to the identification of fetal abnormality in order to:Reassure parents by reducing the likelihood of undiagnosed fetal abnormality.
Assist parents in decision making if by maximizing information about the underlying diagnosed fetal abnormality.
Allow parents of affected pregnancies to prepare to birth of an affected child.
Allow appropriate perinatal management and intrauterine treatment.
Prenatal screening and diagnostic tests
* Screening tests :- are tests performed on all women in order to identify a subset of pt who are at high risk for a disorder.* Diagnostic tests:- are tests carried out on pregnancies that have been identified as
high risk by prior screening test they are usually invasive & carry a risk for miscarriage.Invasive diagnostic tests are # Amniocentesis.# Chorionic Villous Sampling CVS. # Cordocentesis.Non invasive test as USS
Screening tests
Diagnostic tests1) population tested.
All women
Women at high risk
2) purpose of the test.
To select a high- risk group
To diagnose abnormality
3) usual method of testing
-Maternal history-USS-Maternal biochem.
-Maternal virology
-USS
-Amniocentesis.-CVS. -Cordocentesis
4) pre requisite to test
Diagnostic test available
Patient aware of potential risks
5) risk of test.
Anxiety of a screen positive result
Small risk of miscarriage from invasive test
Diagnosis of Structural Abnormalities
Neural Tube Defects (NTDs)
NTDs are among the most common major abnormalities.they occur due to defects in the formation of the neural tube during embryogenesis.
These either affect the cranial vault present in ultrasound as anencephaly (which is universally lethal) or encephalocele (its prognosis is related to the size of defect) or hydrocephaly.
or affecting the spinal cord the caudal end which is termed as spina bifida (the local effects of spina bifida like paralysis of the legs, urinary and fecal incontinence depends on the spinal level and the number of spinal segments affected).
Etiology
multi-factorial, with well-definedenvironmental
Genetic
pharmacological
geographic factors.
Prenatal screening and diagnosis of NTDs
when a parent or a previous sibling has had NTD, the risk of recurrence is 5-10%.
* Mid trimester maternal serum alpha-fetoprotein (AFP) levels are increased in pregnancies affected by open NTDs. These were once used as the established screening tests for NTDs, with screen-positive women being referred for amniocentesis. The presence of acetylcholinesterase (a CNS neurotransmitter) in amniotic fluid was taken as diagnostic for open NTD.
*The need for a two-step screening/diagnosis process was quickly superseded by the development of high resolution u/s. Anencephaly and encephaloceles are detectable on first trimester u/s. spina bifida can be detected at a routine 20-week anomaly scan. The diagnosis may be suspected from the visualization of the 'lemon"(shape of skull) and "banana"(absent cerebellum) signs in the fetal brain at this examination. The sensitivity of u/s for both open and closed NTDs is greater than 95%.
*Other CNS abnormalities such as hydrocephalus can also be detected at the 20-week scan.
PreventionFolate deficiency and drugs that interfere with folate metabolism (like anti-epileptics) are implicated in about 10% of NTDs.
Periconceptual folate supplementation of the maternal diet reduces the risk of developing these defects by about half.
Folic acid should be given for at least 3 months prior to conception and for the first trimester of pregnancy.
The dose of folic acid is 400mcg for primary prevention and 4-5 mg for prevention of recurrence of a NTD or for those of high risk like type 1 diabetes mellitus.
Congenital Heart Defects (CHDs)
These are also common congenital abnormalities.Etiology:
genetic factors, environmental factors and viral infections could be implicated. Gene mutations and chromosomal abnormalities account for less than 5% of cases.
Prenatal diagnosis of CHDs: A 4 chamber view at 20-week anomaly scan is indicated in high risk patients (like those with previous CHD, diabetes mellitus); provides information about the position and size of the fetal heart, the cardiac chambers, and the atrio-ventricular connection.
CHDs associated with abnormal 4-chamber view include hypoplastic left heart, hypoplastic right heart, atrio-ventricular canal defects, large atrial and ventricular septal defects, and others. Although 90% of such anomalies can be detected in a specialist centers, unfortunately only 30% can be detected at routine 20-week anomaly scan
Gastrointestinal Abnormalities
Bowel obstruction above ileum like duodenal and esophageal atresia, usually results in polyhydramnios and easily visualized with u/s.Doudenal atresia is characteristically associated with a "double bubble' appearance on u/s. One third of cases will be associated with Down's syndrome, and karyotyping should be considered.
Abdominal wall defects: 50% of omphaloceles (due to midline abdominal wall defect through which peritoneal sac herniates) have associated cardiac or chromosomal abnormalities.
Renal Tract Abnormalities
Major abnormalities of the renal tract such as renal agenesis will normally be detected by 20-weeks because of the associated oligohydramnios.Diagnosis of Chromosomal Abnormalities:
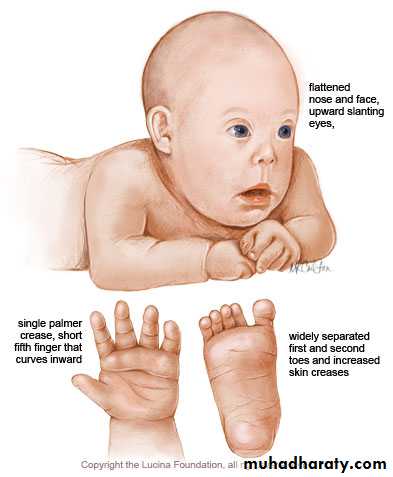
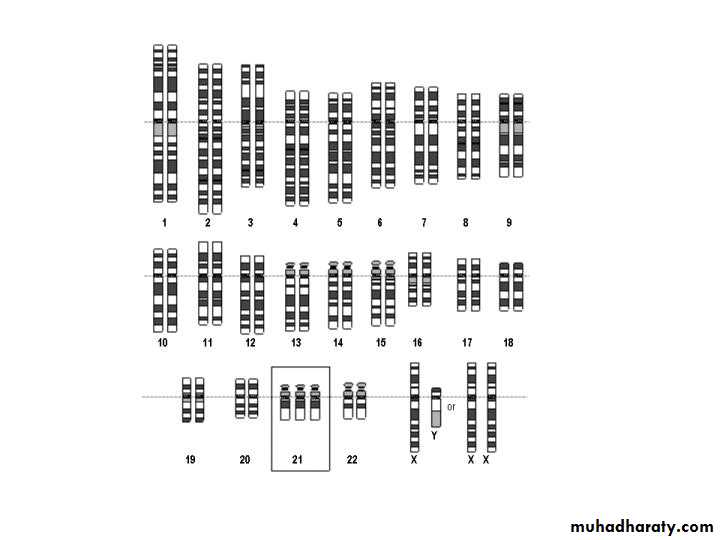
Chromosomal abnormalities**** aneuploidies**** sex chromosomal abnormality** Down syndrome:- the commonest chromosomal abn at birth characterized by IU lethalityof 40%at 12-40 wk , with MR, defness,short sightedness, flat facies , macroglossia, cardiac septal defect, intestinal atresia ,premature ageing reduced immunity, leukemia, reduced life span
Screening tests for down syndrome:-1) maternal Hx:the prevalence of Down syndrome increase with advancing maternal age, therefore women above 35y are routinely screened, & women with previous Hx of Down baby.2) maternal serum biochemistry : by estimating the maternal serum level of alpha-feto protien (decreased) ,hCG (increased) & estriol at 15-22 week (triple test).when we add S.inhibin to them then called quadriple test.
3) nuchal translucency :By sonographic measurement of the translucent space on the neck of the fetus at 10-13 week gestation this NT is increased in majority of aneuoploidy, sensitivity of this test is 75-80% .
4) second trimester USS : identify the soft tissue marker as Echogenic intracardiac focus ,Echogenic bowel,Mild renal pelvis dilatation ,Widened gap between first and second toes ,Clinodactyly, hypoplastic mid-phalanx of fifth digit ,Single transverse palmer crease, Short femur ,Short humerusDiagnostic tests by amniocentesis & CVS.
Invasive Diagnostic Tests
A number of different tests exist to sample material of fetal origin.The sample obtained can be used for
cytogenetic
biochemical
enzymatic
DNA analysis
to give a prenatal diagnosis.
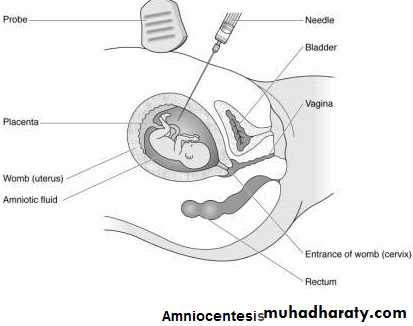
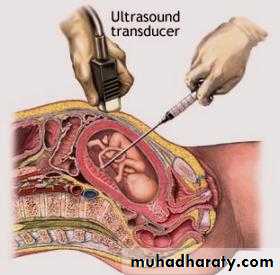
Amniocentesis
A thin needle is passed transabdominally under ultrasound guidance into the amniotic cavity. A small amount of amniotic fluid is removed which contains fetal fibroblasts. This test is usually performed at or after 15 weeks' gestation.
Amniocentesis
Indication;1. Women with positive screening for Down's syndrome.
2. Women with advanced maternal age (traditionally >35 years).
3. U/S detection of abnormality or soft markers.
4. Parental balanced translocation.
5. Previous history of chromosomal abnormality.
Complication:
1. Miscarriage rate of 1%.
2. Cell culture may fail in 0.5% necessitating further invasive tests.
3. Early amniocentesis (<10 weeks) has higher risk of fetal loss rate, fetal talipes, reduced amniocyte culture rate.
4. Cell culture for karyotyping takes 2-3 weeks
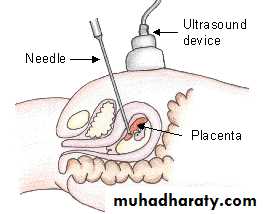
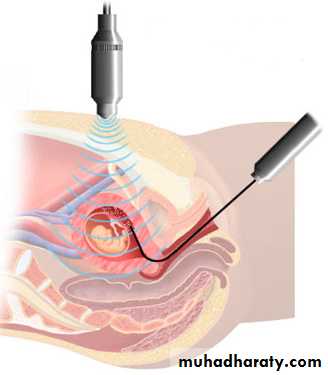
Chorionic Villus Sampling
A thin needle is passed transabdominally or trascervically under u/s guidance into the placenta.
Chorionic villi are feto-placental in origin. This test is usually performed at or after 10 weeks.
Although, it is technically possible to do CVS at earlier gestation, this is generally avoided as it is associated with a higher rate of cleft lip/palate and digital amputation abnormalities.
Transabdominal CVS transcervical CVS
Chorionic Villus Sampling
Indication: CVS has the advantage of yielding a large amount of tissue and is therefore is the method of choice in when large amount of DNA are required as in:Diagnosis in monogenetic disorders.
Early diagnosis of Down syndrome.
Rapid karyotyping within 24-48 hrs.
Complication:
Miscarriage and fetal loss in 1%.
Placental mosaicism in about 2%.
There is association between CVS and limb defect when the procedure is performed at earlier gestational ages.
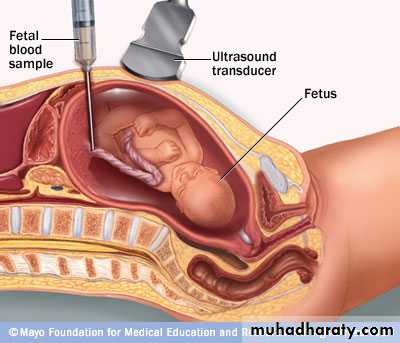
Cordocentesis
a thin needle is inserted transabdominally under u/s guidance into the umbilical cord to sample fetal blood. This test usually performed at or after 20 weeks' gestation.
Indication:
Rapid high-quality karyotyping within 48-72 hrs.
Diagnosis of haematological problems such as anemia, thrombocytopenia.
Assessment of acid- base status of fetus with growth restriction.
Complication:
Bleeding at the site of needle.
Fetal bradycardia.
Fetal loss is 1-2%.
Introduction of infection, more importantly if mother is carrying (HIV )virus transmission to the fetus may occur.
Fetoscopy
with improvement of fiberoptic technology, direct in-utero visualization of the fetus can now be achieved. It is useful in identifying small structural abnormalities and facilitating direct organ biopsy such as skin and muscle biopsy.New Developments in Prenatal Diagnosis:
1. Analysis of fetal cells in the maternal circulation.2. Pre-implantation genetic diagnosis.
3. Three-dimensional ultrasound.
4. Fetal magnetic resonance imaging.