Dr. Khalid A. Al- Khazraji
Lec. 8
PANCREATITIS
Mon. & Tues. 7 & 8 / 3 / 2016
Done By: Ibraheem Kais
2015 – 2016
ﻣﻜﺘﺐ ﺁ
ﺷﻮﺭ ﻟﻼﺳﺘﻨﺴﺎﺥ
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
1
Pancreatitis
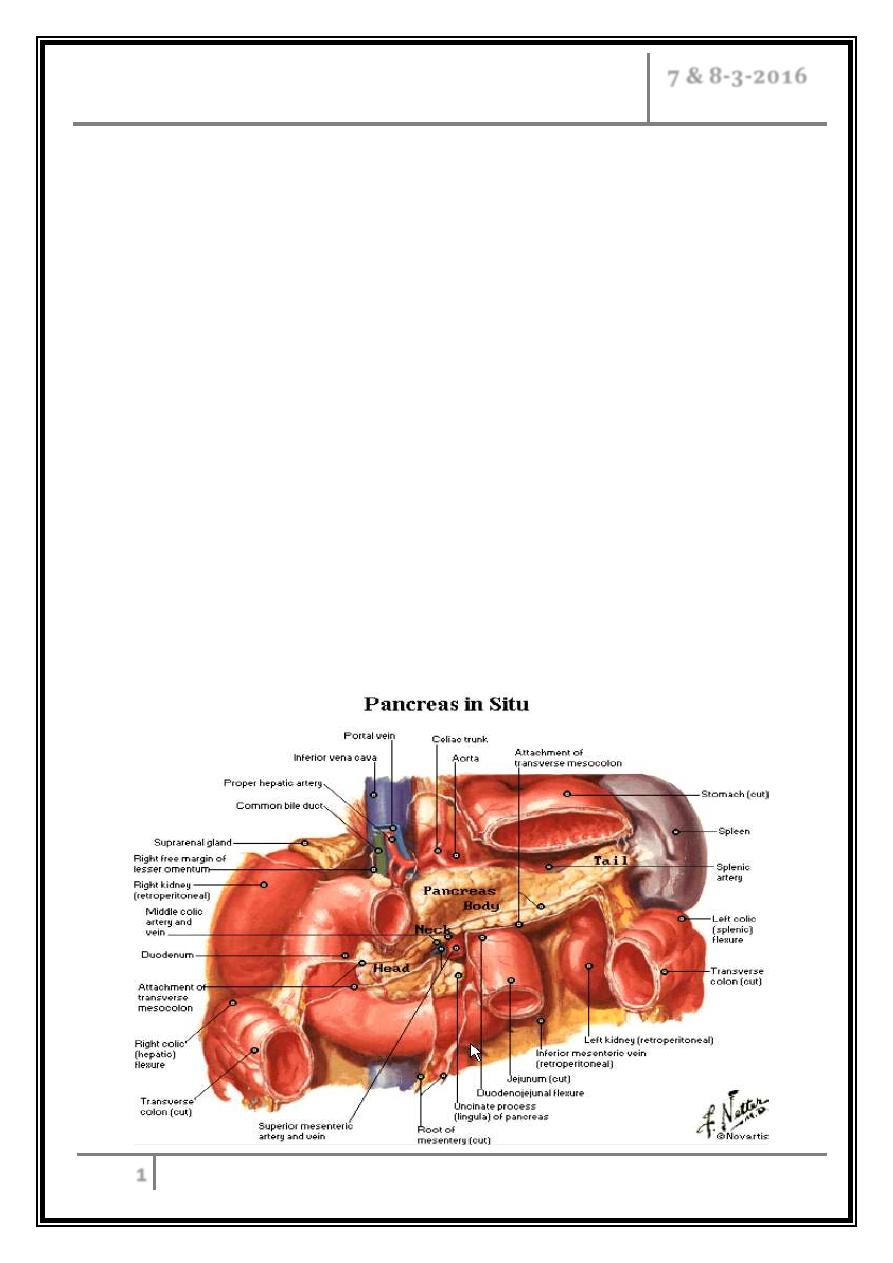
The pancreatic STRUCTURE AND FUNCTION
Extends retroperitoneally across the posterior abdominal wall from the second
part of the duodenum to the spleen.
The head is encircled by the duodenum; the body, which forms the main bulk of
the organ, ends in a tail that lies in contact with the spleen.
The pancreas consists of exocrine and endocrine cells making up 98% of the
human pancreas.
The pancreatic acinar cells are grouped into lobules forming the ductal system
which eventually joins into the main pancreatic duct.
The main pancreatic duct has many tributary ductules and gradually tapers
towards the tail of the pancreas.
The main pancreatic duct itself usually joins the common bile duct to enter the
duodenum as a short single duct at the ampulla of Vater.
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
2
Pancreatic Digestive Enzymes
Pancreatic secretion contains multiple enzymes for digesting all of the three
major types of food: proteins, carbohydrates, and fats.
It also contains large quantities of bicarbonate ions, which play an important
role in neutralizing the acidity of the chyme emptied from the stomach into the
duodenum.
The most important of the pancreatic enzymes for digesting proteins are trypsin,
chymotrypsin, and carboxypolypeptidase. By far the most abundant of these is
trypsin.
Trypsin and chymotrypsin split whole and partially digested proteins into
peptides of various sizes but do not cause release of individual amino acids.
However, carboxypolypeptidase does split some peptides into individual amino
acids, thus completing digestion of some proteins all the way to the amino acid
state.
The pancreatic enzyme for digesting carbohydrates is pancreatic amylase,
which hydrolyzes starches, glycogen, and most other carbohydrates (except
cellulose) to form mostly disaccharides and a few trisaccharides.
The main enzymes for fat digestion are (1) pancreatic lipase, which is capable
of hydrolyzing neutral fat into fatty acids and monoglycerides; (2) cholesterol
esterase, which causes hydrolysis of cholesterol esters; and (3) phospholipase,
which splits fatty acids from phospholipids.
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
3
The endocrine pancreas
This consists of hormone-producing cells arranged in nests or islets (islets of
Langerhans).
The hormones produced are secreted directly into the circulation and there is no
access to the pancreatic ductular system.
There are five main types of islet cells corresponding to different secretory
components.
- The beta-cells for insulin production.
- The alpha-cells produce glucagon.
- The D cells produce somatostatin.
- PP-cells produce pancreatic polypeptide.
- Enterochromaffin cells produce serotonin.
A number of other hormones have been identified within the endocrine pancreas
including gastrin-releasing peptide, neuropeptide Y, and galanin. These are
believed to be neurotransmitters active in the neuro-gastrointestinal axis
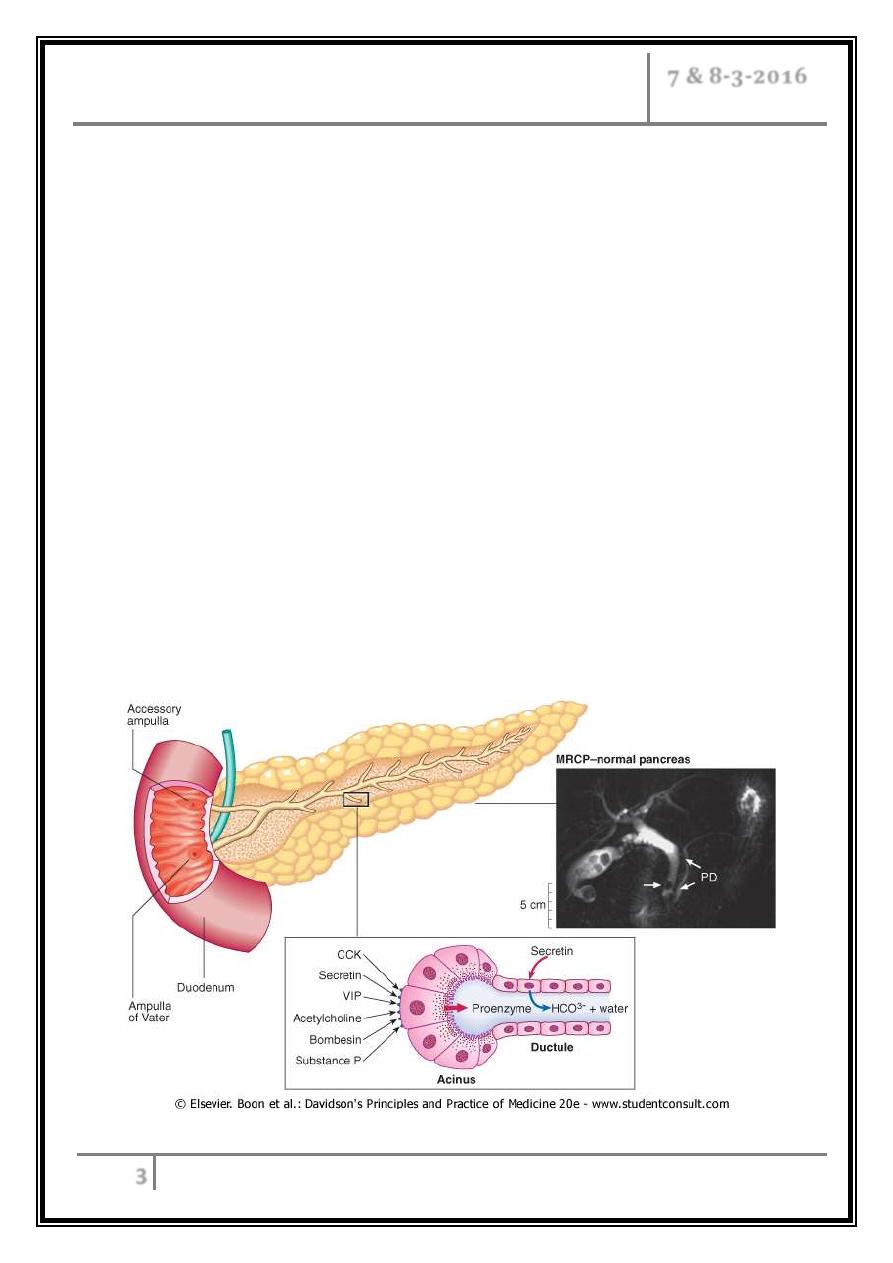
Pancreatic structure and function
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
4
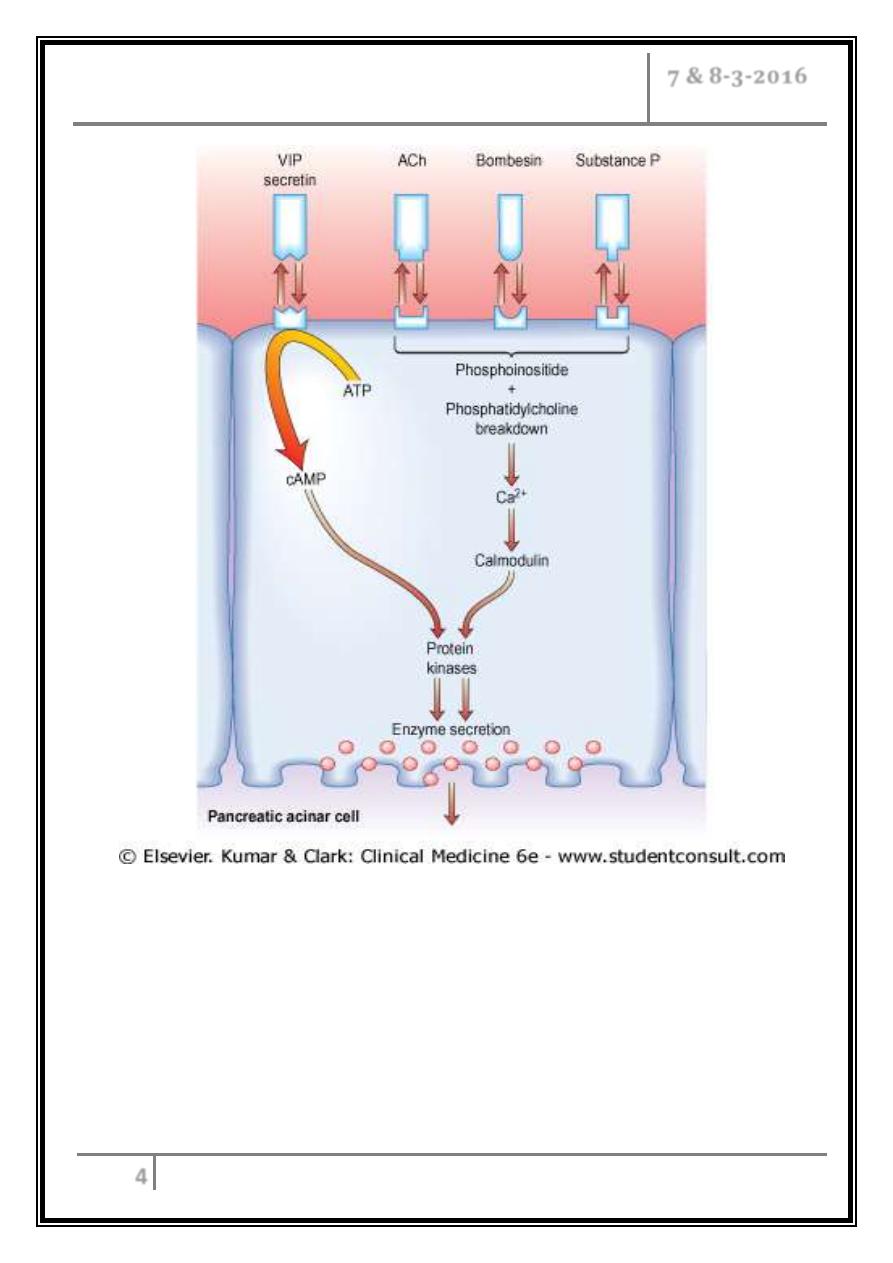
Diagram showing stimulus-secretion coupling of pancreatic cell protein
secretion. There is no CCK receptor in humans; stimulation is probably
via neural fibres. VIP, vasoactive intestinal polypeptide; CCK,
cholecystokinin; ACh, acetylcholine
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
5
Pancreatits definition and classification
Pancreatitis is divided into:-
1- Acute pancreatitis.
2- Chronic pancreatitis.
Acute pancreatitis: an acute inflammatory process of the pancreas that may also
involve peripancreatic tissues and remote organ systems.
Pathologically, two morphologic classifications of acute pancreatitis are
recognized:-
1- Acute interstitial pancreatitis.
2- Acute hemorrhagic necrotizing pancreatitis.
Epidemiology
2-28/100,000 of population.
79.8/100,000 per year in US.
5.4/100,000 per year in England.
3% of all cases of abdominal pain admitted to hospital.
80% of cases are mild with mortality less than 5%.
98% of deaths occur in the 20% of severe cases:
- One third occurs within first week
multi-organ failure.
- After that
sepsis.
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
6
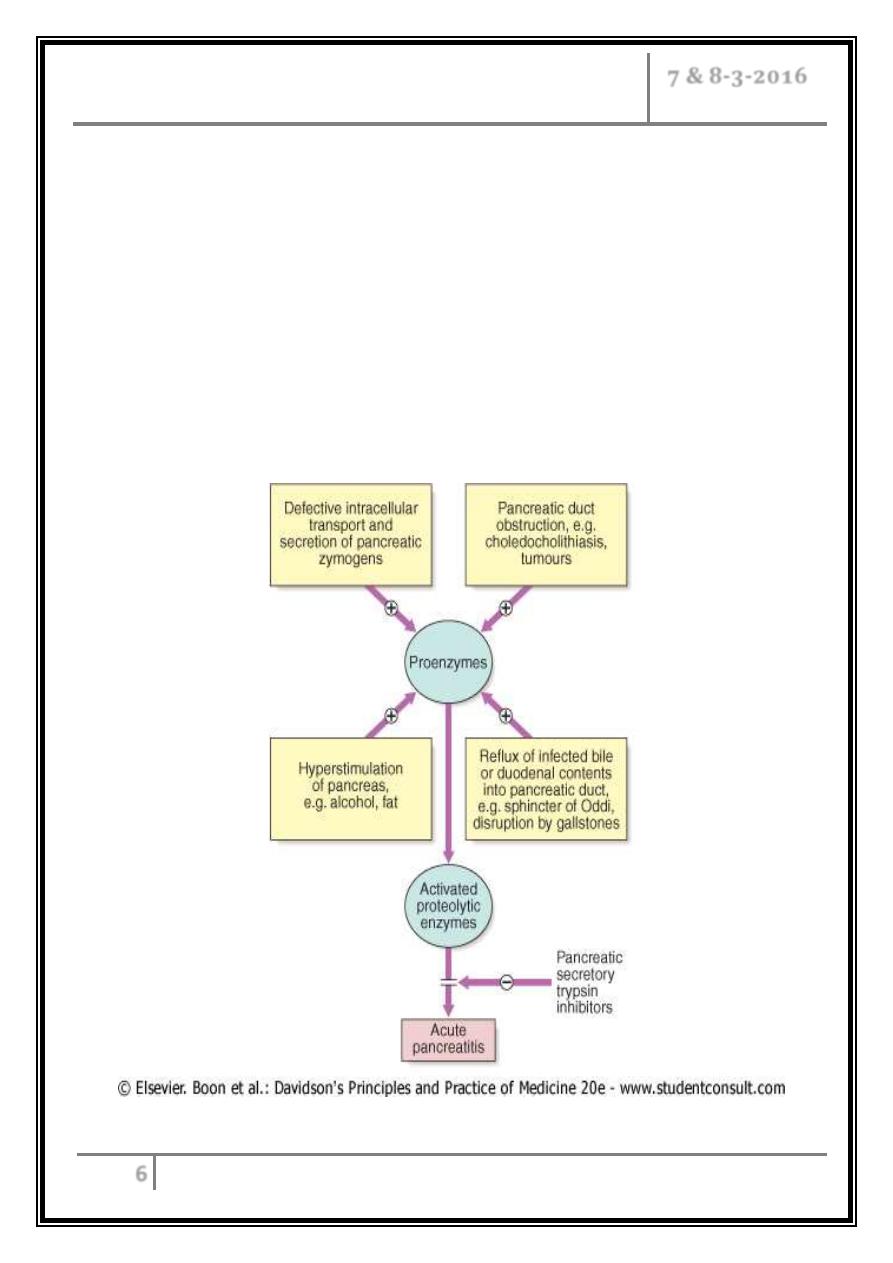
Pathophysiology
o Acute pancreatitis occurs as a consequence of premature activation of zymogen
granules, releasing proteases which digest the pancreas and surrounding tissue.
o The severity of acute pancreatitis is dependent upon the balance between
activity of released proteolytic enzymes and antiproteolytic factors.
o Acute pancreatitis is usually mild and self-limiting, with minimal organ
dysfunction and uneventful recovery. In some patients, however, it is severe,
with local complications such as necrosis, pseudocyst or abscess, and systemic
complications leading to multi-organ failure.
Pathophysiology of acute pancreatitis
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
7
Etiology
Obstructive causes
1- Gallstones (including microlithiasis).
2- Tumors: ampullary or pancreatic tumors.
3- Development anomalies: pancreas divisum, choledochocele, annular
pancreas.
4- Periampullary duodenal diverticula.
5- Hypertensive sphincter of Oddi.
6- Afferent duodenal loop obstruction.
Toxins
1- Ethyl alcohol.
2- Methyl alcohol.
3- Scorpion venom.
4- Organophosphorus insecticides.
Drugs
Azathioprine, 6-mercaptopurine, sulfonamides, estrogens, tetracycline,
valproic acid, metronidazole, furosemide, methyldopa, cimetidine.
Metabolic causes
Hypertriglyceridemia, hypercalcemia, end stage renal disease.
Trauma
1- Accidental: (especially blunt abdominal trauma).
2- Iatrogenic: postoperative, ERCP.
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
8
Infectious
1- Parasitic: ascariasis, clonorchiasis.
2- Viral: mumps, coxsackievirus B, cytomegalovirus, echovirus.
3- Bacterial: mycoplasma, tuberculosis, legionella species.
Vascular
1- Ischemic: hypoperfusion (such as post cardiac surgery).
2- Vasculitis: SLE, polyarteritis nodosa.
Idiopathic
Miscellaneous
1- Penetrating PU.
2- Crohn disease of the duodenum.
3- Pregnancy associated.
4- Pediatric association: Reye syndrome , cystic fibrosis.
Clinical features
1- Severe, constant upper abdominal pain (usually begins in the epigastrium),
involvement of the retroperitoneum lead to radiation of pain to the midback in
65% of cases, builds up over 15-60 minutes. The pain typically last for hours to
days and not relieved by vomiting.
2- Nausea and vomiting are common.
3- Marked epigastric tenderness, but in early stages guarding and rebound
tenderness are absent.
4- Bowel sounds become quiet or absent (paralytic ileus).
5- Hypoxic, hypovolemia shock, oliguria in severe cases.
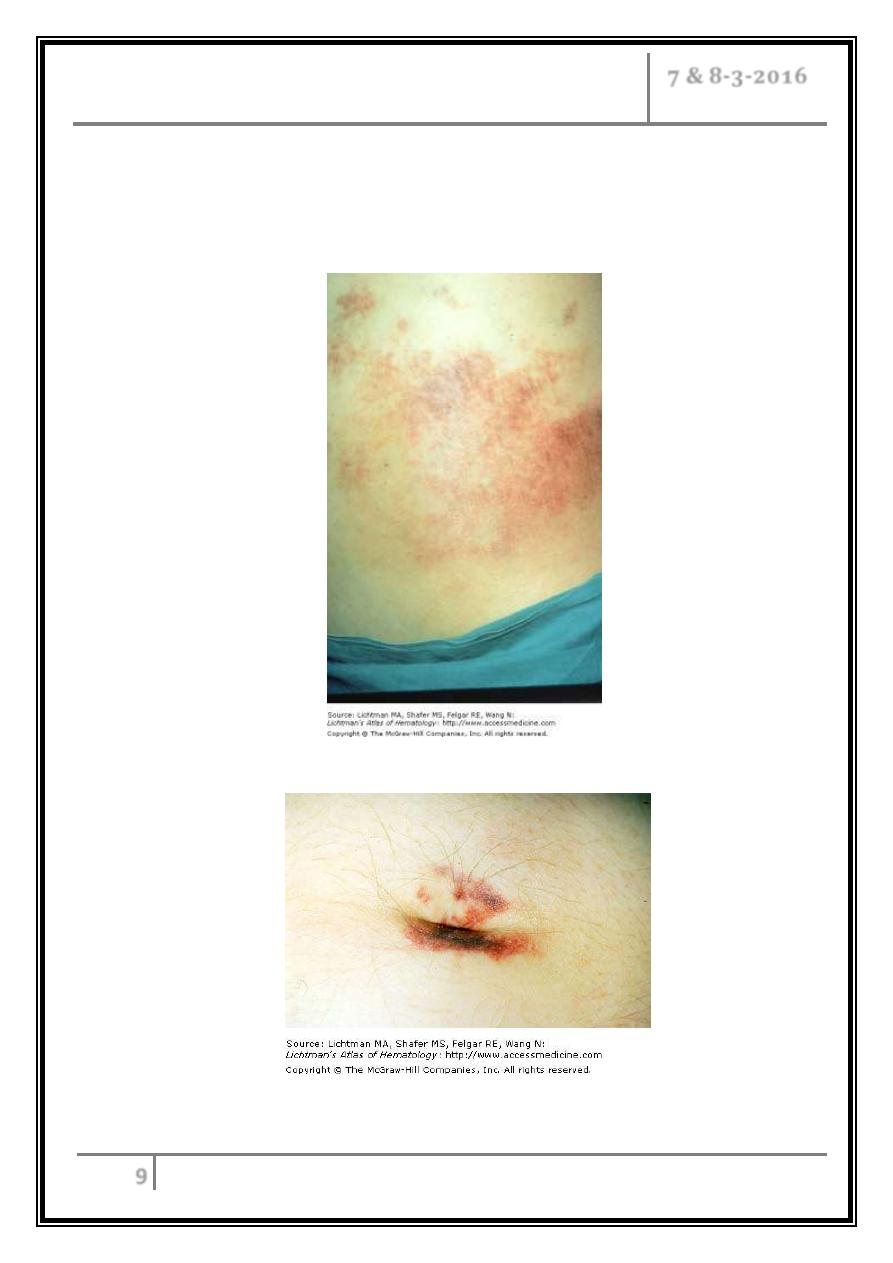
6- Discoloration of the flanks (Grey Turner’s sign) ,or periumbilical region
(Cullen’s sign) is a feature of severe pancreatitis with haemorrhage.
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
9
7- In patients with a gallstone aetiology the clinical picture may also include the
features of jaundice or cholangitis.
8- Fever usually less than 38.5 C.
Grey-Turner
’s sign
Cullen
’s sign
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
10
Diagnosis
Blood tests
1- S.Amylase: extremely sensitive test if it’s 3 times the upper limit of normal when
measured within 24 hours of the onset of pain. It falls back gradually towards
normal over the next 3-5 days.
Elevation of serum amylase unrelated to pancreatitis:
I. Leakage of upper gastrointestinal contents into the peritoneum:
- Upper gastrointestinal perforation.
- Biliary peritonitis.
- Intestinal infarction.
II. Inherited abnormalities of amylase:
- Macroamylasaemia.
2- Urinary amylase: may be diagnostic as remain elevated over a longer period of
time.
3- Serum lipase: remains elevated for a longer period of time than those of
amylase but accuracy is not greater than amylase and technically difficult.
4- C reactive protein: useful in assessment and prognosis.
5- Full blood count, urea, electrolytes, blood glucose, liver biochemistry, plasma
calcium, and arterial blood gases, used for assessment.
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
11
Radiology
1. An erect chest X-ray is mandatory to exclude gastroduodenal perforation,
which also raises the serum amylase. A supine abdominal film may show
gallstones or pancreatic calcification.
2. An abdominal ultrasound scan is used as a screening test to identify a
possible biliary (gallstone) cause of pancreatitis. Gallstones are difficult to
detect in the distal common bile duct but dilated intrahepatic ducts may be
present in the presence of bile duct obstruction. Stones within the gall bladder
are not sufficient to justify a diagnosis of gallstone-related pancreatitis. The
ultrasound may also demonstrate pancreatic swelling and necrosis as well as
peripancreatic fluid collections if present. In severe pancreatitis the pancreas
may be difficult to visualize because of gas-filled loops of bowel.
3. Contrast-enhanced spiral CT scanning is essential in all but the mildest
attacks of pancreatitis. Carried out within 2-3 days of presentation, it allows
the extent of pancreatic necrosis to be assessed. This provides very valuable
prognostic information. Later in the course of the disease, repeated CT scans
may be used to detect other complications including fluid collections, abscess
formation, and pseudocyst development.
4. MRI (MRCP) can assess the degree of pancreatic damage and identify
gallstones within the biliary tree. MRI is particularly useful to differentiate
between fluid and solid inflammatory masses.
5. ERCP is used as a treatment measure to remove bile duct stones in the
presence of gallstone-related pancreatitis.
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
12
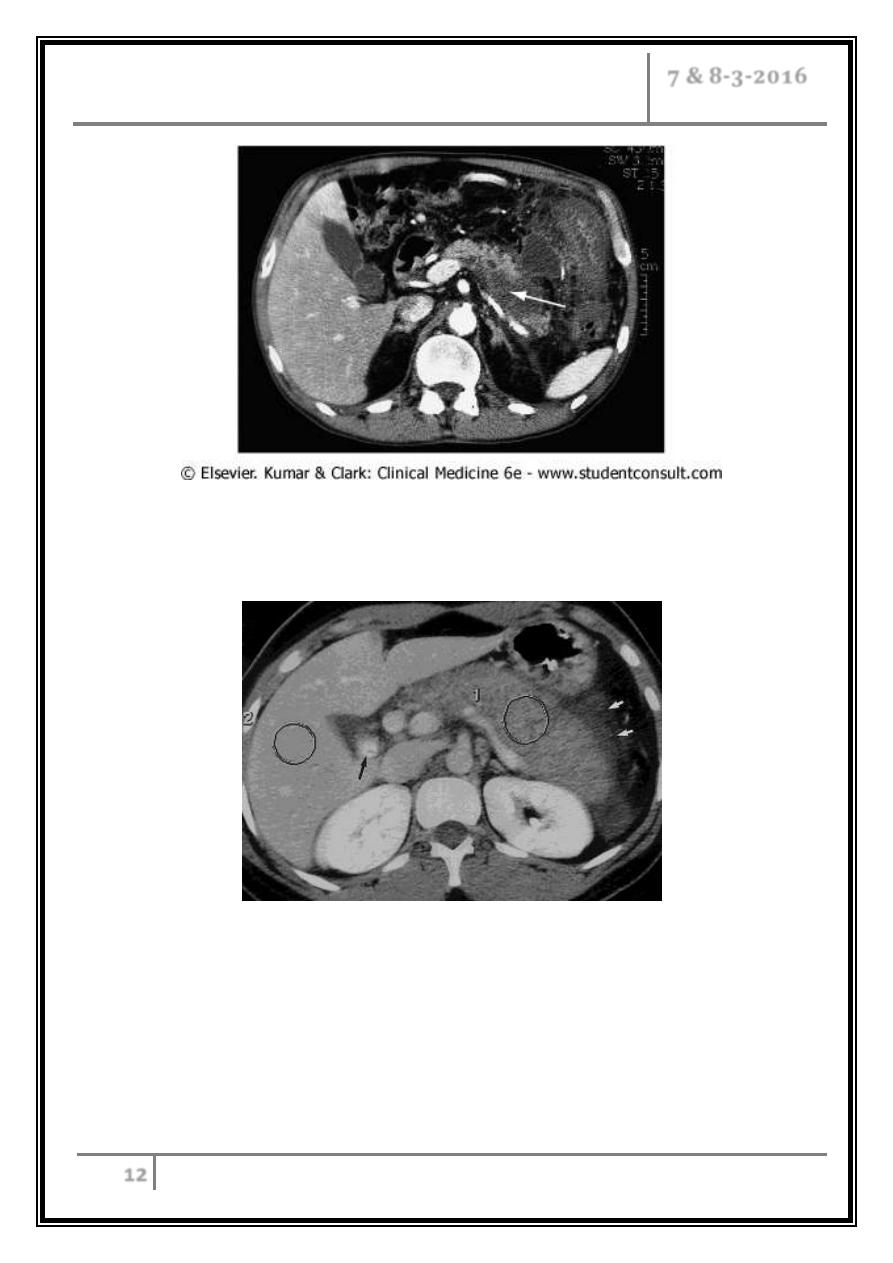
CT scan in patient with acute pancreatitis showing necrosis of the
pancreatic parenchyma (arrow) and a fluid collection extending outside the
gland with inflammatory thickening of the colon.
Gallstone-induced pancreatitis in 27 year-old woman
Transverse CT scan obtained with intravenous and oral contrast material
reveals a large, edematous, homogeneously attenuating (73-HU) pancreas (1)
and peripancreatic inflammatory changes (white arrows). Although the
attenuation values are low, there is no pancreatic necrosis. Calcified gallstones
are seen in gallbladder (black arrow). 2 = liver (140 HU).
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
13
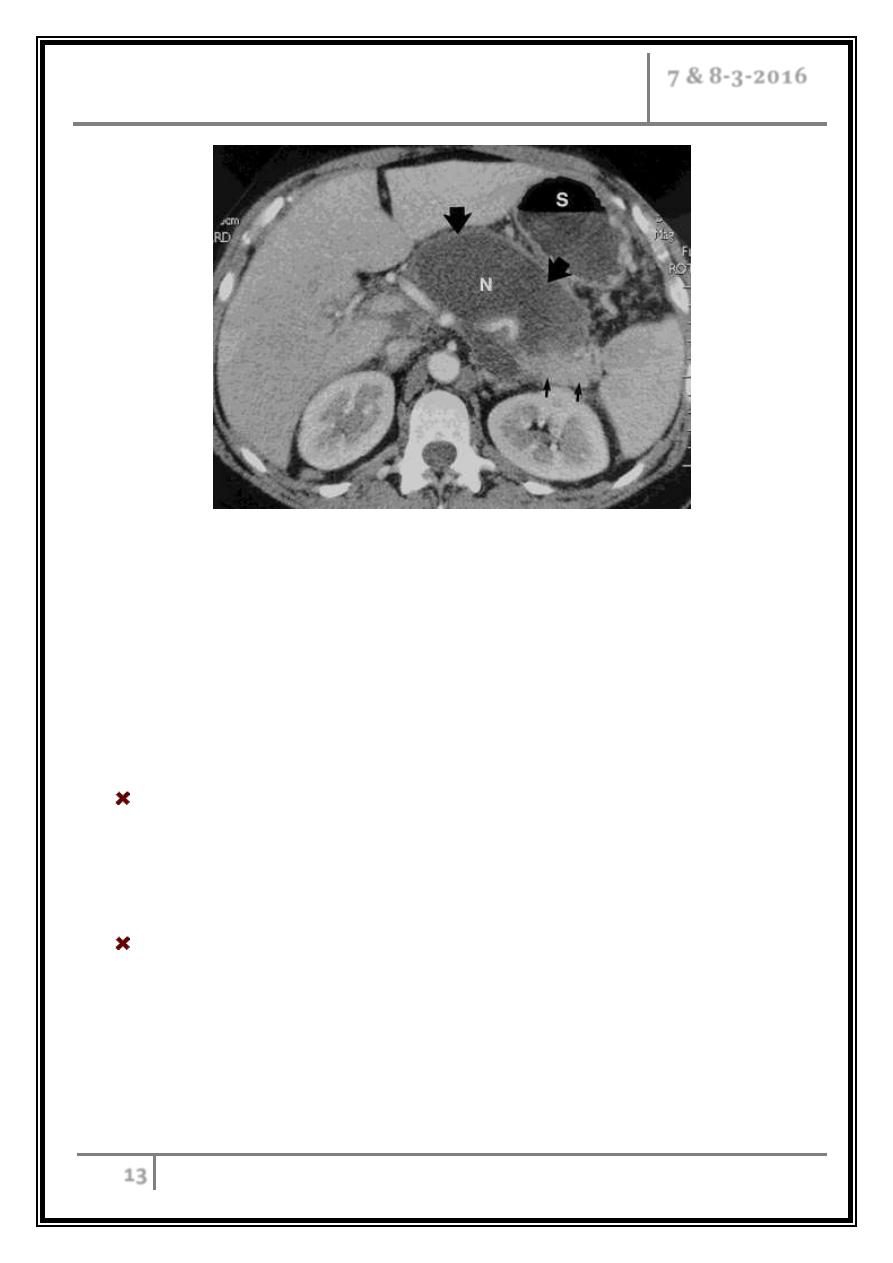
50 year-old woman with acute pancreatitis (1st view)
(a, b) Transverse CT scans obtained with intravenous and oral contrast
material reveal an encapsulated fluid collection associated with liquefied
necrosis (large straight arrows) in the body of the pancreas. The head, part of
the body, and the tail of the pancreas are still enhancing (small straight
arrows). N = liquefied gland necrosis, S = stomach.
Assessment of disease severity
The majority of cases of acute pancreatitis are mild, but approximately 25% run
a more complicated course which may result in haemodynamic instability and
multiple organ failure. The early prediction of such a severe attack allows
appropriate monitoring and intensive care to be in place.
Factors during the first 48 hours that indicate severe pancreatitis & a poor
prognosis (three or more factors present predict a severe episode): -
- Age> 55 years, WBC> 15 ×109/L, Blood glucose> 10 mmol/L, Serum
urea> 16 mmol/L, Serum albumin< 30 g/L, Serum aminotransferase>
200 U/L, Serum calcium< 2 mmol/L, Serum LDH> 600 U/L, Pao2< 8.0
kPa (60 mmHg).
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
14
The Ranson and Glasgow scoring systems are based on such parameters and
have been shown to have an 80% sensitivity for predicting a severe attack .
The APACHE II scoring system parameters
Physiological
- Temperature.
- Heart rate.
- Respiratory rate.
- Mean arterial pressure.
- Glasgow Coma Scale.
Laboratory
- Oxygenation (Pao2).
- Arterial pH.
- Serum: sodium, potassium,
creatinin levels.
- Haematocrit.
- White blood cells count.
Ranson’s CRiteRia
Ranson's criteria on admission:
- Age greater than 55 years.
- A white blood cell count of > 16,000/µL.
- Blood glucose > 11 mmol/L (>200 mg/dL).
- Serum LDH > 350 IU/L.
- Serum AST >250 IU/L.
Ranson's criteria after 48 hours of admission:
- Fall in hematocrit by more than 10 percent.
- Fluid sequestration of > 6 L.
- Hypocalcemia (serum calcium < 2.0 mmol/L (<8.0 mg/dL)).
- Hypoxemia (PO2 < 60 mmHg).
- Increase in BUN to >1.98 mmol/L (>5 mg/dL) after IV fluid hydration.
- Base deficit of >4 mmol/L.
Score 0-2: 2% mortality
Score 3-4: 15% mortality
Score 5-6: 40% mortality
Score 7-8: 100% mortality
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
15
Complications
Local complications:
1. Fluid collections.
2. Pancreatic necrosis.
3. Acute pseudocyst.
4. Pancreatic abscess.
Systemic complications:
1. Systemic inflammatory response syndrome (SIRS).
2. Respiratory complications: most frequent systemic complications. Hypoxemia
occurs within first 48 hr.
3. Hyperglycemia.
4. Hypocalcaemia.
5. Reduced serum albumin concentration.
6. GI bleeding (gastric or duodenal erosions).
7. Renal failure.
8. Pancreatic encephalopathy.
9. Subcutaneous fat necrosis and bone abnormalities.
Differential diagnosis
1. Biliary colic.
2. Perforated hollow viscus.
3. Mesenteric ischemia.
4. Closed-loop intestinal obstruction.
5. Inferior wall MI.
6. Dissecting aneurysm.
7. Ectopic pregnancy.
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
16
Treatment
The initial management of acute pancreatitis is similar, whatever the cause.
A multiple factor scoring system (ideally APACHE II with a modification for
obesity) should be carried out at the end of the first 24 hours after presentation
to allow identification of the 25% of patients with a predicted severe attack. This
should be repeated at 48 hours to identify a further subgroup who appear to be
moving into the severe category.
Early fluid losses in acute pancreatitis may be large, requiring well-maintained
intravenous access as well as a central line and urinary catheter to monitor
circulating volume and renal function.
Naso-gastric suction: prevents abdominal distension and vomitus and hence the
risk of aspiration pneumonia.
Baseline arterial blood gases determine the need for continuous oxygen
administration.
Prophylactic antibiotics are not indicated unless there are infective
complications (broad-spectrum antibiotics).
Analgesia requirements: pethidine and tramadol are the drugs of choice. The
morphine derivatives should be avoided because they can cause sphincter of
Oddi contraction.
Feeding: nn patients with a severe episode there is a little likelihood of oral
nutrition for a number of weeks. Total parenteral nutrition has been associated
with a high risk of infection and has been replaced by enteral nutrition. This is
administered via a naso-jejunal tube, which is well tolerated and can maintain
adequate nutritional input.
In a small proportion of patients, multiorgan failure will develop in the first few
days after presentation reflecting the extent of pancreatic necrosis. Such
patients will require positive-pressure ventilation and often renal support.
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
17
Prophylaxis of thromboembolism with low-dose subcutaneous heparin is
advisable.
Gallstone-related pancreatitis and associated cholangitis, endoscopic
intervention with sphincterotomy and stone extraction is of proven benefit and is
the treatment of choice.
Chronic pancreatitis
It is a chronic inflammatory condition characterized by fibrosis, destruction of
exocrine tissue and eventually destruction of exocrine and endocrine tissue.
Chronic pancreatitis predominantly affects middle-aged alcoholic men.
Aetiology
1. In developed countries the most common cause is alcohol in 60-80% of cases.
2. In developing countries malnutrition – induced (tropical) is the most prevalent.
3. In a small group of patients chronic pancreatitis has been shown to be
hereditary.
4. Almost all patients with cystic fibrosis have established chronic pancreatitis,
usually from birth.
5. Obstruction of the pancreatic duct because of either a benign or malignant
process may result in chronic pancreatitis.
6. Congenital abnormalities of the pancreatic duct, in particular pancreas divisum.
7. 20% of cases are idiopathic.
8. Trauma or prolonged metabolic disturbance.
9. Autoimune pancretitis – IGg4
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
18
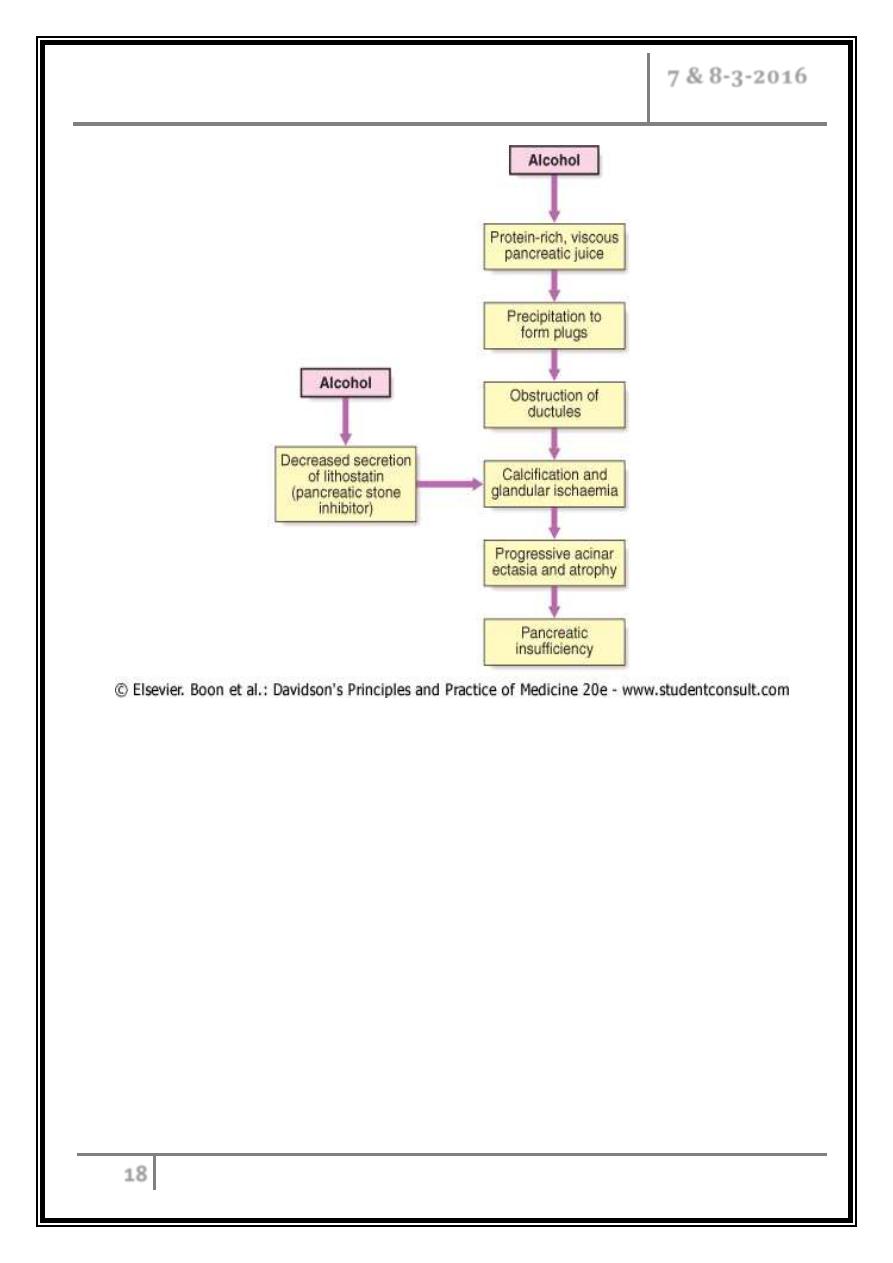
Pathophysiology of chronic pancreatitis
Clinical features
Almost all present with abdominal pain. Usually epigastric and often radiates
through into the back. Pain is due to a combination of increased pressure within
the pancreatic ducts and direct involvement of pancreatic and peripancreatic
nerves by the inflammatory process. Approximately one-fifth of patients
chronically consume opiate analgesics.
Weight loss is common and results from a combination of anorexia, avoidance
of food because of post - prandial pain, malabsorption and/or diabetes.
Steatorrhoea occurs when more than 90% of the exocrine tissue has been
destroyed; protein malabsorption only develops in the most advanced cases.
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
19
Overall, 30% of patients are diabetic, but this figure rises to 70% in those with
chronic calcific pancreatitis.
O/E: reveals a thin, malnourished patient with epigastric tenderness. Skin
pigmentation over the abdomen and back is common and results from chronic
use of a hot water bottle (erythema ab igne). Many patients have features of
other alcohol- and smoking-related diseases
Investigations
Tests to establish the diagnosis
- Ultrasound.
- CT (may show atrophy, calcification or ductal dilatation).
- Abdominal X-ray (may show calcification).
- MRCP.
- Endoscopic ultrasound.
Tests of pancreatic function
- Collection of pure pancreatic juice after secretin injection (gold standard but
invasive and seldom used).
- Faecal pancreatic chymotrypsin or elastase.
- Oral glucose tolerance test.
Tests of anatomy prior to surgery
- MRCP.
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
20
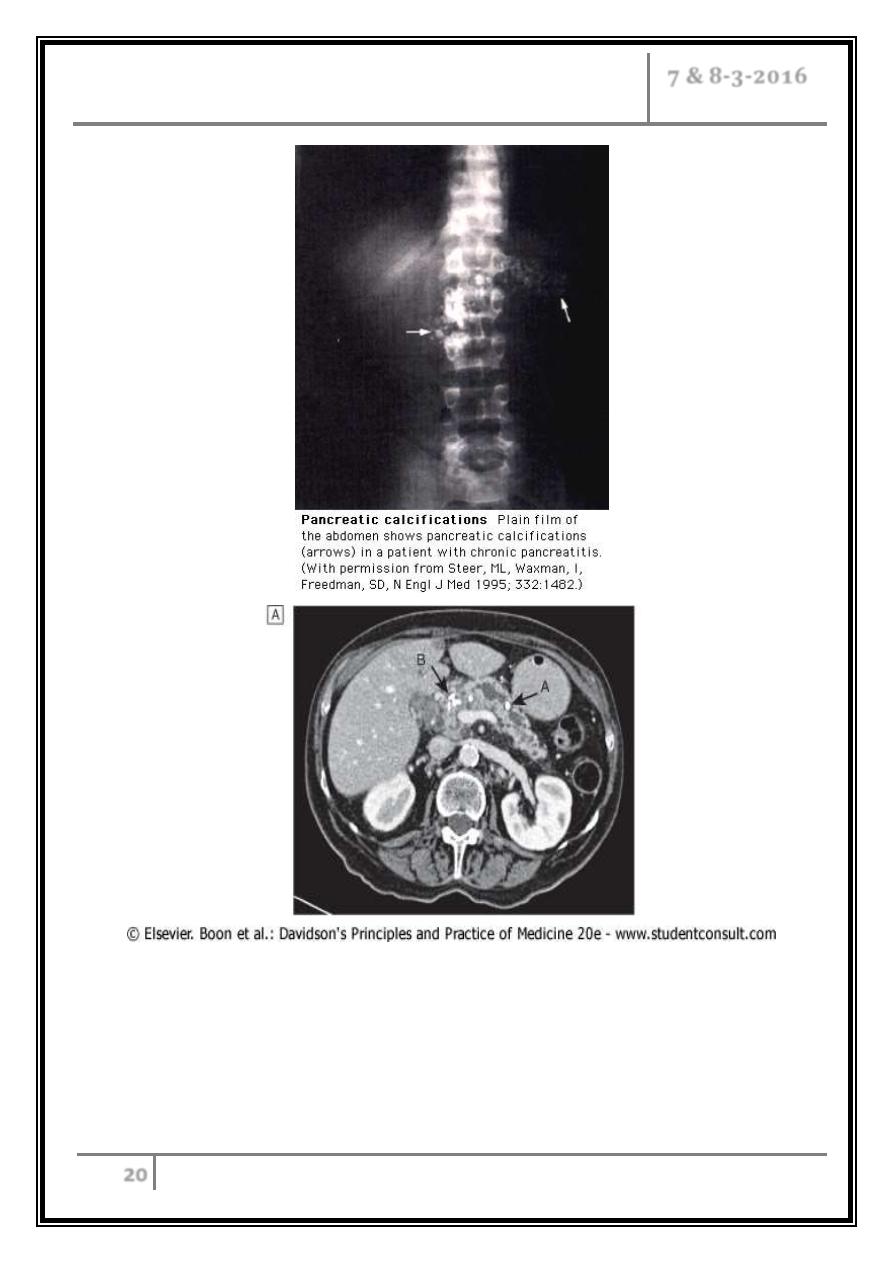
Imaging in chronic pancreatitis. CT scan showing a grossly dilated and
irregular duct with a calcified stone (arrow A). Note the calcification in
the head of the gland (arrow B). MRCP of the same patient showing
marked ductal dilatation with abnormal dilated side branches (arrows A).
A small cyst is also present (arrow B).
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
21
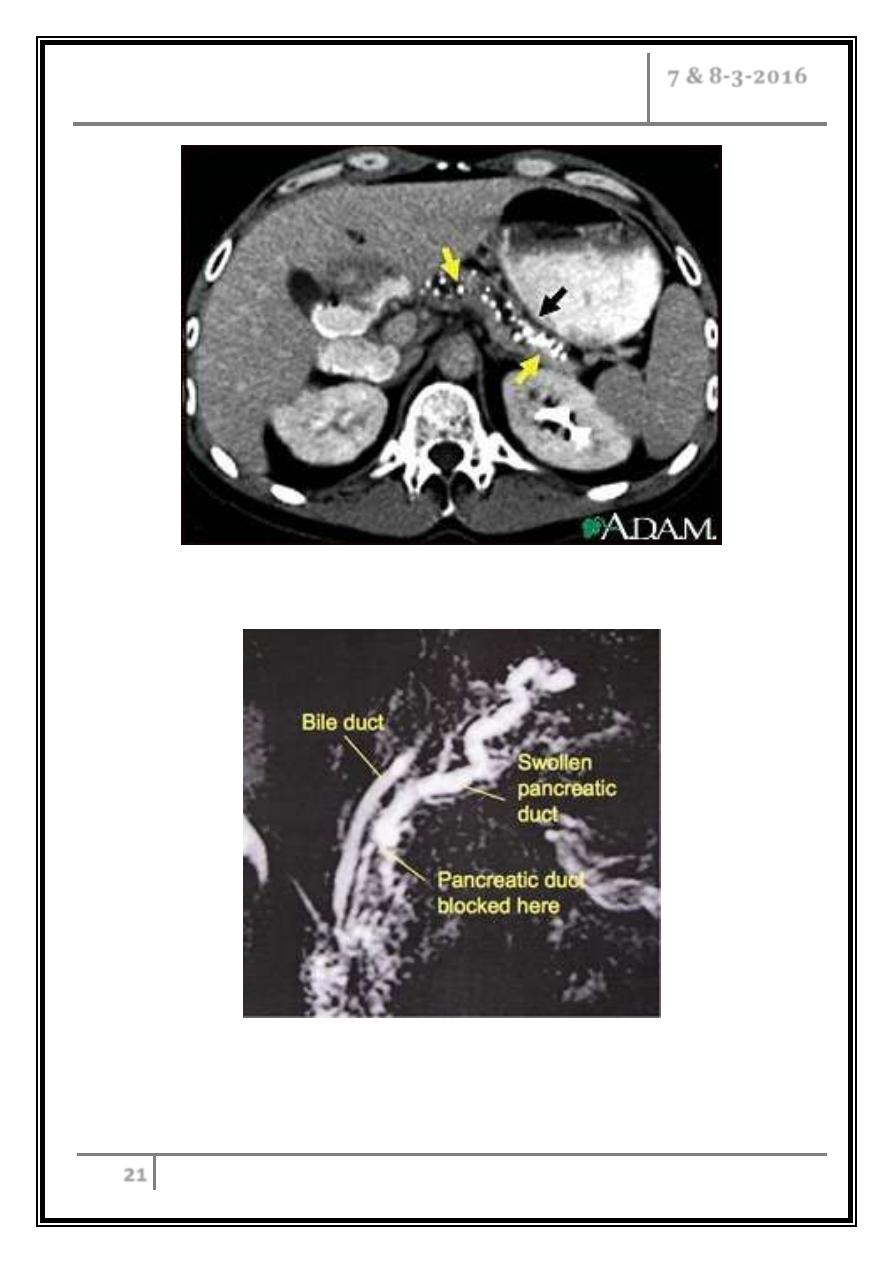
CT scan of the upper abdomen showing multiple white-colored
calcifications. These occur in chronic pancreatitis
This MRCP picture shows chronic pancreatitis causing a narrowing of
the pancreatic duct, with a swollen tortuous duct visible upstream
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
22
Complications
Pseudocysts and pancreatic ascites, which occur in both acute and chronic
pancreatitis.
Extrahepatic obstructive jaundice due to a benign stricture of the common bile
duct as it passes through the diseased pancreas.
Duodenal stenosis.
Portal or splenic vein thrombosis leading to segmental portal hypertension and
gastric varices.
Peptic ulcer.
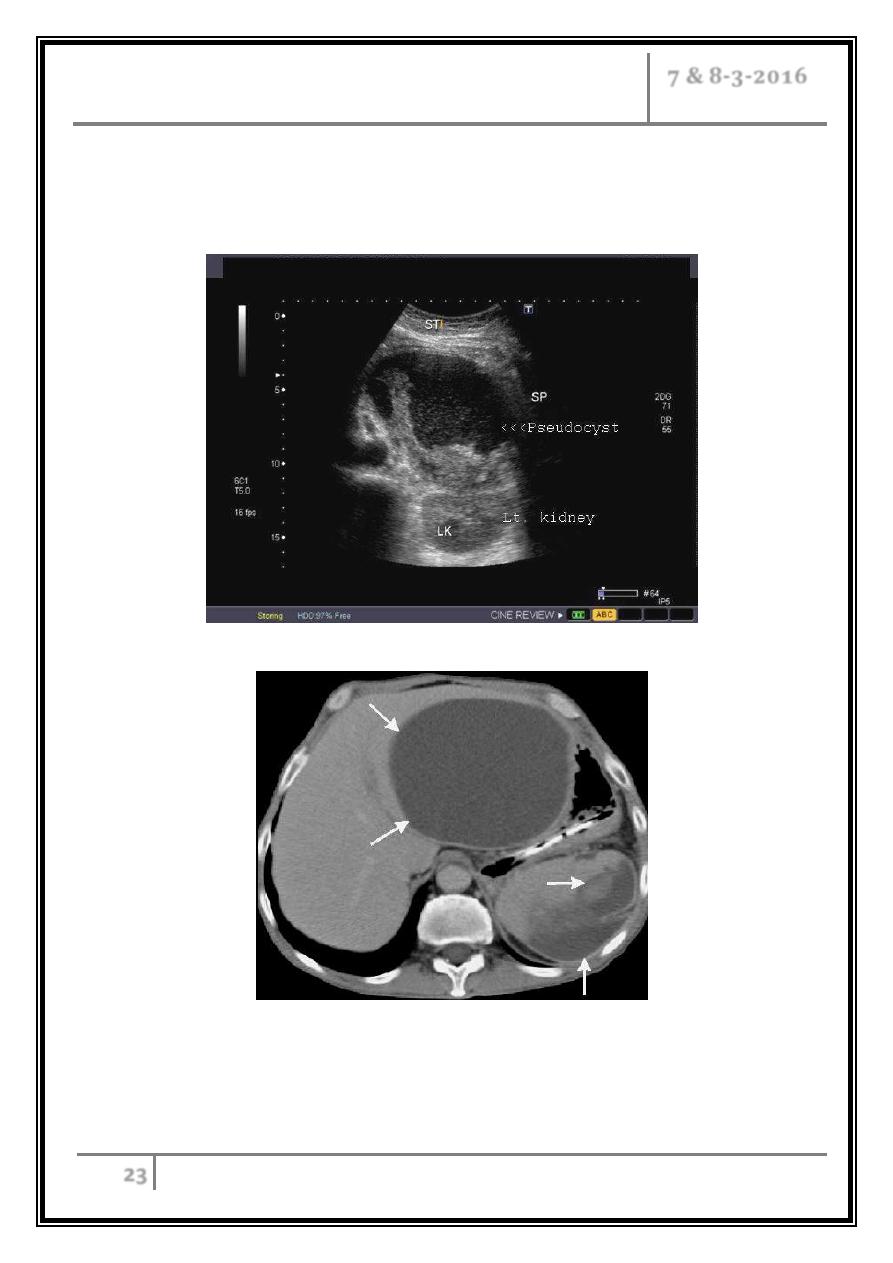
Pancreatic pseudocyst
It’s the most common structural complication of chronic pancreatitis.
It’s a fluid collection surrounded by granulation tissue.
Intra- or retroperitoneal rupture, bleeding or cyst infection occurs.
The larger cysts may occlude nearby structures including the duodenum and the
bile duct.
In pseudocysts, less than 6 cm in diameter, spontaneous resolution can be
anticipated.
In larger cysts that have been present for a period in excess of 6 weeks,
resolution is uncommon and a long-term complication rate of approximately
30% can be anticipated.
Many pseudocysts are closely opposed to the posterior wall of the stomach or
duodenum and can be successfully drained endoscopically using endoscopic
ultrasound to identify the optimum drainage site. A direct fistula is created
between the pseudocyst lumen and the gastric or duodenal lumen which is then
kept patent by the insertion of plastic stents. This approach will be successful in
approximately 75% of cases.
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
23
Surgical drainage is required for failures of endoscopic therapy or in
circumstances in which the pseudocyst anatomy does not allow endoscopic
access
Pancreatic pseudocyst
CT examination: A giant, sharp-contoured, hypodense lesion is depicted
(arrows). Is pancreatic pseudocyst in the omental bursa
Pancreatitis Dr. Khalid A. Al- Khazraji
7 & 8-3-2016
24
Management
o Alcohol avoidance is crucial in halting the progression of the disease and
reducing pain. Unfortunately, the majority of patients continue to drink alcohol.
o Pain relief: for short-term flare-ups of pain a combination of a non-steroidal
anti-inflammatory drug and an opiate (tramadol) is usually sufficient for
symptomatic relief, but the severe and unremitting nature of the pain often leads
to opiate use with the risk of addiction.
o Tricyclic antidepressants are used for chronic pain and reduce the need for
opiates.
o Oral pancreatic enzyme supplements suppress pancreatic secretion (by a
negative-feedback mechanism) and their regular use reduces analgesic
consumption in some patients.
o Patients who are abstinent from alcohol and who have severe chronic pain
which is resistant to conservative measures are considered for surgical or
endoscopic pancreatic therapy. Coeliac plexus nerve block or minimally
invasive thoracoscopic splanchnicectomy sometimes produces long-lasting pain
relief although relapse eventually occurs in the majority of cases.
o Steatorrhoea associated with pancreatic insufficiency may be high, with up to
30 mmol of fat lost per 24 hours. This will usually improve with pancreatic
enzymes supplements and a low fat diet.
o Current preparations are presented in the form of microspheres which reduce
the problems of acid degradation in the stomach. An acid suppressor (H2-
receptor antagonist PPI) is also given.
… End …
