Peripheral nerve disease
Peripheral neuropathy
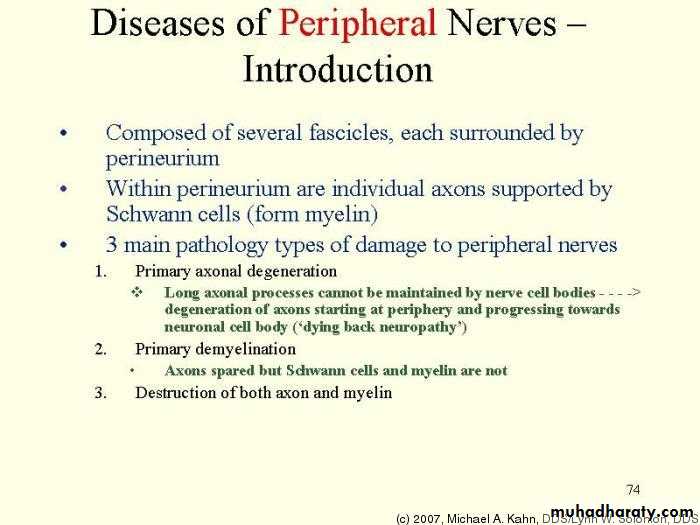
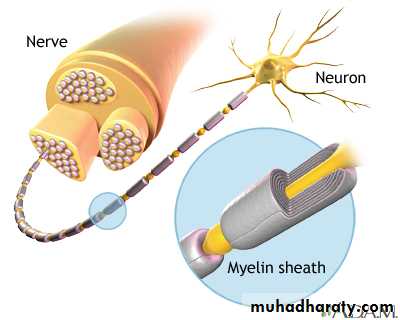
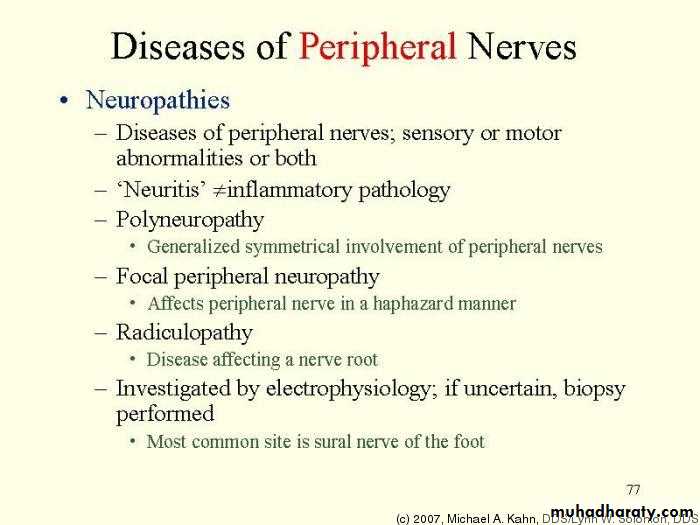
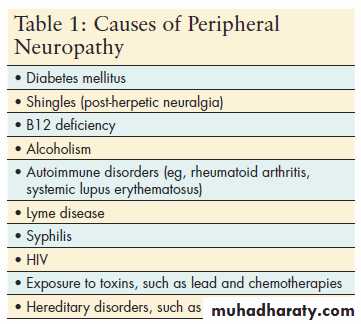
inherited and acquired pathological processes may affect the nerve roots (radiculopathy), the nerve plexuses (plexopathy) and/or the individual nerves (neuropathy).anatomical pattern ----
Single root ----monoradiculopathyMononeuropathy means focal involvement of a single nerve and implies a local process. Direct trauma, compression or entrapment, vascular lesions, and neoplastic infiltration diabetes mellitus, hypothyroidism,acromegaly, alcoholism, and HNPP
Multiple mononeuropathy or mononeuropathy multiplex
signifies simultaneous or sequential damage to multiple noncontiguous nerves
vasculitis or microangiopathy in diabetes mellitus, infectious, granulomatous,
leukemic, or neoplastic infiltration, sarcoidosis and -Multifocal motor neuropathy
Polyneuropathy is characterized by symmetrical, distal motor, and sensory deficits that have a graded increase in severity distally and by distal attenuation of reflexes. The sensory deficits produce a stocking-glove pattern.
Classification
ClassificationAcute
Subacute
Chronic
Small nerve fibers
Large nerve fibers
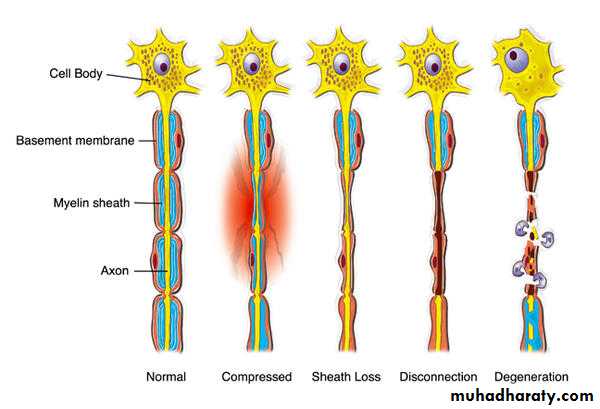
• Axonal• Demylination
• Mixed
• Classification
predominantly motor manifestations
Multifocal motor neuropathyGuillain-Barre syndrome
Acute motor axonal neuropathy
Porphyric neuropathy
Chronic inflammatory polyradiculoneuropathy
Neuropathy with osteosclerotic myeloma
Hereditary motor sensory neuropathies[ Charcot-Marie-Tooth disease)
Lead intoxication
Predominant sensory involvement diabetes; carcinoma; Sjogren's syndrome; dysproteinemia; acquired immunodeficiency syndrome (AIDS); vitamin B12 deficiency; celiac disease; intoxications with cisplatin, thalidomide, or pyridoxine; and inherited idiopathic sensory neuropathies.
Autonomic dysfunction is seen in GBS amyloid and diabetic, idiopathic panautonomic neuropathy, Porphyria, Hereditary sensory and autonomic neuropathy
Clinical features
Motor nerve involvement produces features of a lower motor neuron lesion weakness fasciculation crampssensory nerve : Parasthesia numbness analgesia anasthesia
Autonomic fibre involvement may cause postural hypotension due to disruption of vasomotor control, sweating, cardiac rhythm, and gastrointestinal, bladder and sexual functions
Acute Inflammatory Demyelinating Polyradiculoneuropathy (Guillain-Barre Syndrome)
motor weakness, areflexia, paresthesias with slight sensory loss, and increased protein in CSF without pleoeytosis (albuminocytological dissociation). The frequent finding of motor conduction block and reduced NCVs provided electrophysiologicalconfirmation of widespread demyelination
Features required for diagnosis
Progressive weakness of both legs and arms
A reflexia
Clinical features supportive of diagnosis
Progression 1 day -4 weeks
Relative symmetry of signs
Mild sensory symptoms or signs
Cranial nerve involvement (bifacial palsies)
Recovery beginning 2—4 wks after progression ceases
Autonomic dysfunction
Absence of fever at onset
Laboratory features supportive of diagnosis
Elevated cerebrospinal fluid protein with normal cells count
Elcctrodiagnostic features of nerve conduction slowing or block
Clinical features
1-4 weeks after respiratory infection or diarrhoea (particularly Campylobacter) in 70% of Patients.
Distal paraesthesia and numbness (often severe) precede a rapidly ascending muscle weakness, from lower to upper limbs, more marked proximally than distally.
Facial and bulbar weakness commonly develops,
respiratory weakness requiring ventilatory support occurs in 20% of cases. In most patients, weakness progresses for 1-4 weeks, but rapid deterioration to respiratory failure can develop within hours. On examination there is diffuse weakness with widespread loss of reflexes.
Clinical features
GBS TypesAcute inflammatory demyelinaring polyradiculoneuropathy
Acute motor axonal neuropathy
Acute motor sensory axonal neuropathy
Millar-Fisher syndrome (ophthalmoplegia, ataxia and areflexia)
Acute pandysautonomia
Sensory GBS
two thirds of patients report a preceding event, most frequently an upper respiratory or gastrointestinal infection Campylobacter jejuni, surgery, or immunization 1—4 weeks before the onset of neurological symptoms
Treatment
Supportive care in intensive care
Respiratory and bulbar function, the ability to handle secretions, heart rate, and blood pressure should be closely monitored during the progressive phase
mechanical ventilation
deterioration in forced vital capacity (FVC),
declining maximal respiratory pressures, and hypoxemia caused by atelectasis
rapid disease progression (onset to admission in less than 7 days), bulbar dysfunction, bilateral facial palsies, and autonomic instability
lower the risks of venous thrombosis and pulmonary embolism
Prevention and prompt treatment of infections
Chest physiotherapy and frequent oral suctioning
regular turning and attention to skin, eyes, mouth, bowel, and bladder
Physical therapy
Psychological support and constant reassurance
Plasma exchange and high-dose intravenous immune globulin(IVIG) infusions have been shown to be equally effective in moderate to severe weakness
Up to 30% of patients develop respiratory insufficiency requiring assisted ventilation, and between 2% and 5% die of complications.
20% still have residual motor weakness 1 year later. Approximately 70% of patients complete their recovery in 12 months and 82% in 24 months.
Chronic Inflammatory Demyelinating polyneuropathy
similar clinical features and CSF change and pathological abnormalities of multifocal with nerve conduction features reflectingdemyelination. to GBS
The major differences between the two conditions are
in the time course and their response to corticosteroids
Prednisone, plasmapheresis, and IVIg
Multifocal Motor Neuropathy with Conduction Block
more common in men
Progressive, asymmetrical, predominantly distal limb weakness. Profound weakness in muscles with normal bulk
Treatment with IVIG is currently the preferred treatment
Porphyric Neuropathy
inactivation of one of allelic genes that encodes for an enzyme of the heme biosynthetic pathway this provokes a compensatory overproduction of porphyrins and their precursors
Dominantly inherited disorders
Fits + abdominal pain +autonomic manifestationsOnly a few patients progress to develop the more ominous motor neuropathy with generalized, proximal, or asymmetrical muscle weakness developing over days or weeks