Intracranial hemorrhage
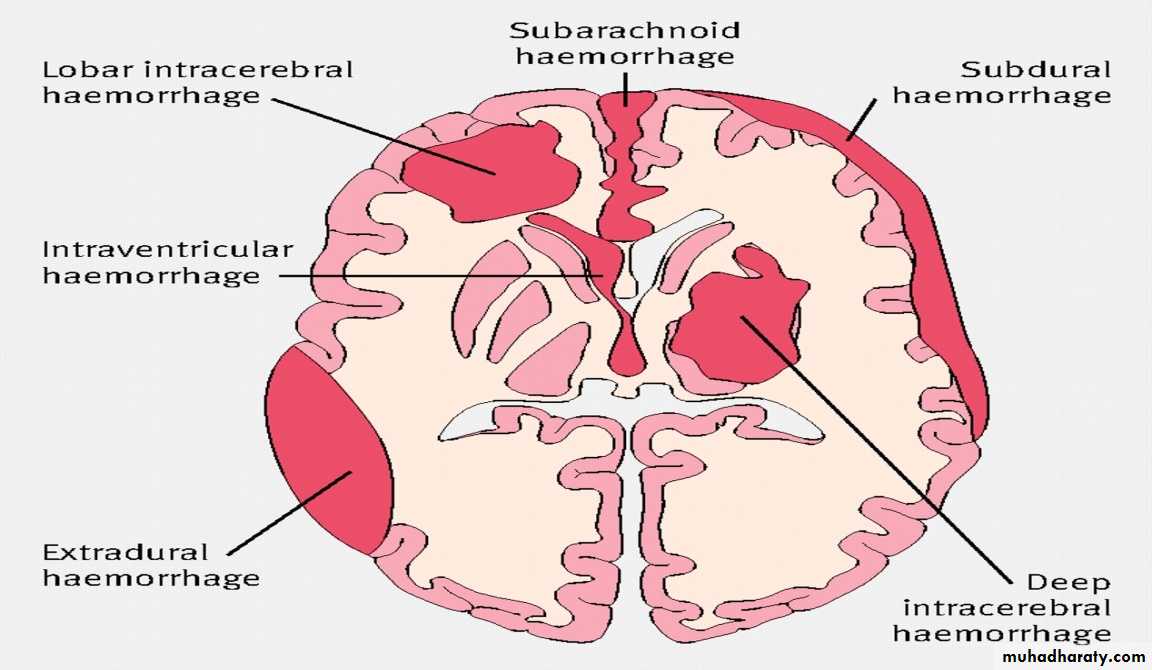
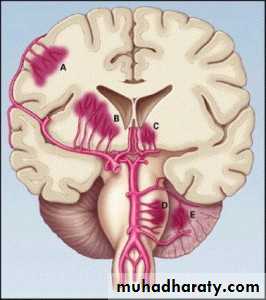
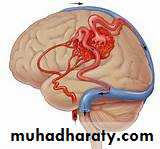
hemorrhage, or bleeding, within the cranial vault [skull] Either within the meninges or parenchymal bleedingtypes
IntracerebralCAPSULER
LOBER
Menengeal space
SUB DURAL
SUBARACHNOID
EPIDURAL
Intracranial hemorrhage
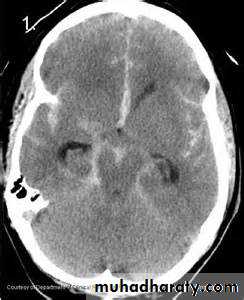
Thalamic
15%Pontine 8%
Cerebeller 8%
Lllober
20%
Putamen
40%
Putamen
40%
Thalamic
15%Cerebeller 8%
Pontine 8%
Lllober
20%Intracerebral HGE SITES
Etiology
hypertension, eclampsiaarteriopathy (eg, cerebral amyloid angiopathy, moyamoya)
drug abuse
reperfusion injury, hemorrhagic transformation
cold exposure)
rupture of an aneurysm or arteriovenous malformation (AVM)
altered hemostasis (eg, thrombolysis, anticoagulation, bleeding diathesis)
hemorrhagic necrosis (eg, tumor, infection)
venous outflow obstruction (eg, cerebral venous thrombosis)
EPIDEMIOLOGY
Each year, intracerebral hemorrhage affects approximately 15 per 100,000 individuals
Asian countries have a higher incidence of intracerebral hemorrhage than other regions of the world
a 30-day mortality rate of 45%.
Pontine or other brainstem intracerebral hemorrhage has a mortality rate of 75% at 24 hours.
slight male predominance
individuals older than 55 years and doubles with each decade until age 80 years.
In individuals younger than 45 years, lobar hemorrhage is the most common site
S & S
• Onset of symptoms of intracerebral hemorrhage is usually during daytime activity, with onset between (minutes to hours)• S & S of Raised ICP[ because of the presence of the mass]
Alteration in level of consciousness
Nausea and vomiting
Headache
Seizures
Clinical S and S
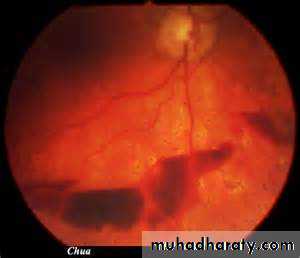
• 3. Subhyaloid retinal hemorrhages• 4. Focal neurological deficits –
Contralateral hemiparesis, contralateral sensory loss, contralateral conjugate gaze paresis, homonymous hemianopia, aphasia, neglect, or apraxia
Brain stem - Quadriparesis, facial weakness, decreased level of consciousness, gaze paresis, ocular bobbing, miosis [pinpoint] , or autonomic instability [hyperpyrexia]
Cerebellum - Ataxia
Laboratory Studies
Complete blood count (CBC) with platelets: Monitor for infection and assess hematocrit and platelet count to identify hemorrhagic risk and complications.Prothrombin time (PT)/activated partial thromboplastin time (aPTT): Identify a coagulopathy.
Serum chemistries including electrolytes and osmolarity: Assess for metabolic derangements, such as hyponatremia, and monitor osmolarity for guidance of osmotic diuresis.
Toxicology screen and serum alcohol level if illicit drug use or excessive alcohol intake is suspected: Identify exogenous toxins that can cause intracerebral hemorrhage.
Screening for hematologic, infectious, and vasculitic etiologies in select patients: Selective testing for more uncommon causes of intracerebral hemorrhage.
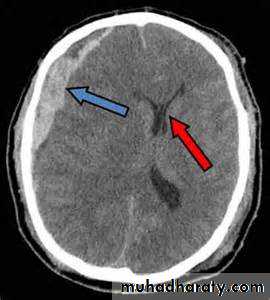
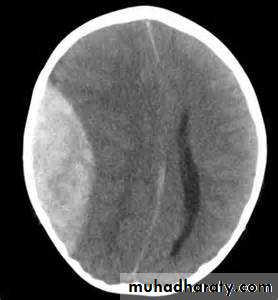
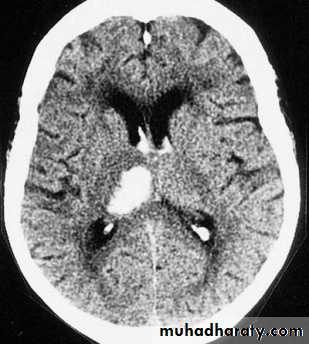
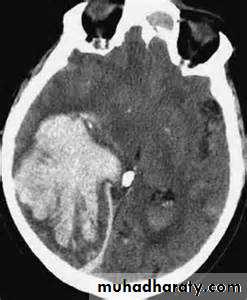
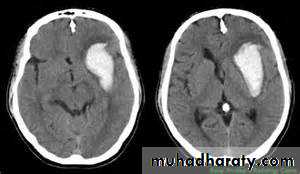
the principle imaging for ICH is CT scanning
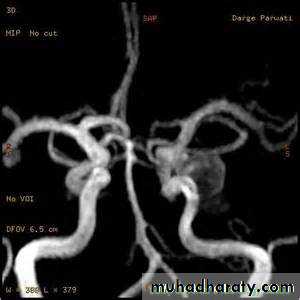
Conventional T1 and T2 sequences are not highly sensitive to hemorrhage in the first few hours, but newer gradient refocused echo sequences appear to be able to detect intracerebral hemorrhage reliably within the first 1-2 hours of onset (MRI studies incorporating gradient echo or susceptibility-weighted sequences may be used as the sole imaging modality for patients with acute stroke, readily identifying intracranial hemorrhage• Vessel imaging
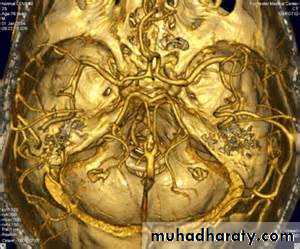
• CT angiography permits screening of large and medium-sized vessels for AVMs, vasculitis, and other arteriopathies.• MR angiography permits screening of large and medium-sized vessels for AVMs, vasculitis, and other arteriopathies.
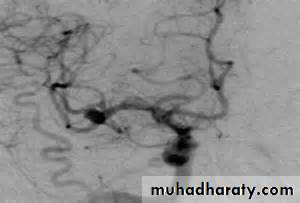
• Conventional catheter angiography definitively assesses large, medium-sized, and sizable small vessels for AVMs, vasculitis, and other arteriopathies
Consider catheter angiography for
• young patients
• patients with lobar hemorrhage
• patients without a history of hypertension
• patients without a clear cause of hemorrhage who are surgical candidates.
CT angiography
MRI angiographyCatheter MRI angiography
Treatment
Rapidly stabilize vital signs, and simultaneously acquire emergent CT scan.Intubate and hyperventilate if intracranial pressure is increased; initiate administration of mannitol for further control.
Maintain euvolemia, using normotonic rather than hypotonic fluids, to maintain brain perfusion without exacerbating brain edema.
Avoid hyperthermia.
Correct any identifiable coagulopathy with fresh frozen plasma, vitamin K, protamine, or platelet transfusions.
Initiate fosphenytoin or other anticonvulsant definitely for seizure activity or lobar hemorrhage, and optionally in other patients
treatment
recombinant factor VIIa (rFVIIa) within 4 hours after the onset of intracerebral hemorrhage limits the growth of the hematoma, reduces mortality, and improves functional outcomes at 90 days
Cautiously lower blood pressure to a mean arterial pressure (MAP) less than 130 mm Hg, but avoid excessive hypotension. Early treatment in patients presenting with spontaneous intracerebral hemorrhage is important as it may decrease hematoma enlargement and lead to better neurologic outcome
Treatment [surgery ]:
Consider surgery for patients with• cerebellar hemorrhage greater than 3 cm,
• patients with intracerebral hemorrhage associated with a structural vascular lesion
• young patients with lobar hemorrhage
• Hydrocephalus
Complications
Neurological deficits or deathSeizures
Hydrocephalus
Spasticity
Urinary complications
Aspiration pneumonia
Neuropathic pain
Deep venous thrombosis
Pulmonary emboli
Cerebral herniation
Prognosis
Early reduction in the level of consciousness carries an ominous prognosis.
. Larger hematomas have a worse outcome.
Lobar hemorrhage has a better outcome than deep hemorrhage.
Significant volume of intraventricular blood is a poor prognostic indicator.
The presence of hydrocephalus is associated with a poor outcome.
subarachnoid hemorrhage (SAH)
extravasations of blood into the subarachnoid space between the pial and arachnoid membranes80% are due to a ruptured berry aneurysm
Rupture of arteriovenous malformations (AVMs) accounting for 10% of cases of SAHIncreased blood pressure
Fibro muscular dysplasiapolycystic kidney disease
aortic coarctation
Blood vessel disorders: Systemic lupus erythematosus (SLE), Moyamoya disease,[6] granulomatous angiitis
Genetic disorders: Marfan syndrome, Ehlers-Danlos syndrome, Osler-Weber-Rendu syndrome, pseudoxanthoma elasticum
Metastatic tumors to cerebral arteries: Atrial myxoma, choriocarcinoma
Infections: Bacterial, fungal == mycotic aneurysm
disease states associated with higher incidence of berry aneurysms include the following
prognosis
10-15% of patients die before reaching the hospital.25% of patients die within 24 hours, with or without medical attention
40% in the first month.
. Rebleeding, a major complication, carries a mortality rate of 51-80%.
Thunderclap headachen : a severe headache that takes seconds to minutes to reach maximum intensity often described as the "worst headache of my life The headache may be accompanied by nausea and/or vomiting from increased ICP Photophobia and visual changes are common Sudden loss of consciousness (LOC) occurs at the ictus Seizures during the acute phase of SAH occur in 10-25% of patients
• Sentinel headaches
• Less severe hemorrhages or minor loss of blood from the aneurysm are reported to occur in 30-50% of aneurysmal SAHs. Sentinel leaks produce sudden focal or generalized head pain that may be severe. Sentinel headaches precede aneurysm rupture by a few hours to a few months, with a reported mean of 2 weeks prior to discovery of the SAH.
Signs of meningeal irritation
Neck stiffnessKerning sign
Bruduzneski sign
Funduscopy may reveal papilledema. Subhyaloid retinal hemorrhage
oculomotor nerve palsy with or without ipsilateral mydriasis, which results from rupture of a posterior communicating artery aneurysm. Abducens nerve palsy is usually due to increased ICP
S & S related to aneurysmal site :
Posterior communicating artery/internal carotid artery:focal, progressive retro-orbital headaches and oculomotor nerve palsy
Middle cerebral artery: contralateral face or hand paresis, aphasia (left side), contralateral visual neglect (right side)
Anterior communicating artery:
bilateral leg paresis and bilateral Babinski sign
Investigation
Non contrast CT followed by CT angiography (CTA) of the brain can rule out SAH with greater than 99% sensitivity.
LP may be negative if performed less than 2 hours after an SAH occurs;
LP is most sensitive 12 hours after onset of symptoms.
CSF samples taken within 24 hours of the ictus usually show a WBC-to-RBC ratio that is consistent with the normal circulating WBC-to-RBC ratio of approximately 1:1000.
After 24 hours, CSF samples may demonstrate a polymorphonuclear and mononuclear polycytosis secondary to chemical meningitis caused by the degradation products of subarachnoid blood.
xanthochromia is present 12 hours after the bleed and remains for approximately 2 weeks.
Xanthochromia is present 3 weeks after the bleed in 70% of patients, and it is still detectable at 4 weeks in 40% of patients
. Spectrophotometry is much more sensitive than the naked eye
Vessels imaging
10-20% of patients with clinically diagnosed SAH (on CT and/or lumbar puncture) have negative angiographic findings. A repeat angiogram is usually required in 10-21 days in such cases.MD-CTA derives from its noninvasiveness and a sensitivity and specificity comparable to that of cerebral angiography. This technique is beneficial in very unstable patients who cannot undergo angiography or in emergent settings prior to operative intervention for clot evacuation
Treatment
admitted to the intensive care unit (ICU) with strict bed rest the bed should be kept elevated at 30° to ensure optimal venous drainageantihypertensive agents when the mean arterial pressure (MAP) exceeds 130 mm Hg
Patients with signs of increased ICP or herniation should be
intubated and hyperventilated. Minute ventilation should be titrated to achieve a PCO2 of 30-35 mm Hg. Avoid excessive hyperventilation, which may potentiate vasospasm and ischemia.
Osmotic agents (eg, mannitol), which can decrease ICP dramatically (50% 30 minutes post administration)
Loop diuretics (eg, furosemide) also can decrease ICP
Early surgery or coiling is generally recommended in patients with straightforward aneurysms of a favorable clinical grade. Evidence from clinical trials suggests that patients who undergo surgery within 72 hours have a lower rate of rebleeding and tend to fare better than those treated later
Surgical treatment to prevent rebleeding consists of clipping the ruptured berry aneurysm. Endovascular treatment(ie, coiling) is an increasingly practiced alternative to surgical clipping. The neurosurgeon/neurointerventionalist must be involved early in the care of the patient with an aneurysmal SAH
higher-grade patients and those with significant medical co morbidities tend to be treated by coiling rather than clipping. Posterior circulation aneurysms are preferentially treated by coiling because of the significant morbidity and mortality associated with surgical clipping. The incidence of rebleeding was slightly higher in the coiled group,
Treatment of complication
For prevention of vasospasm, maintenance of normovolemia, normothermia, and normal oxygenation are paramount. Volume status should be monitored closely, with avoidance of volume contraction, which can predispose to vasospasm.Nimodipine
Complication and causes of death
HydrocephalusRebleeding
Vasospasm
Seizures
Cardiac dysfunction