
1
Third stage
Medicine
Lec-1
د
.
بشار
1/1/2014
GAIT and INVOLUNTARY MOVEMENTS
Abnormal gait
Seeing a patient walk can be very revealing for neurological diagnosis and is an important
element of assessing disability. Patterns of weakness, loss of coordination and
proprioceptive sensory loss produce a range of abnormal gaits .
Neurogenic gait disorders need to be distinguished from those due to skeletal
abnormalities, usually characterised by pain producing an antalgic gait, or limp. Gaits that
do not fit either pattern may be due to psychiatric disorders and are usually incompatible
with any anatomical or physiological deficit .
Pyramidal gait
Upper motor neuron (pyramidal) lesions cause a gait in which the upper limb is held in
flexion and the ankle joint in the lower limb kept relatively extended, the leg is swung
outwards at the hip (circumduction). In a hemiplegia, the asymmetry between the affected
and normal sides is obvious in walking. In a paraparesis, both lower limbs swing slowly from
the hips in extension and dragged stiffly over the ground .This can often be heard as well as
seen.
Foot drop
In normal walking, toe strike follows heel strike during the gait cycle.
If there is a lower motor neuron lesion affecting the lower limb , weakness of ankle
dorsiflexion disrupts this pattern. The result is a less controlled descent of the foot making a
slapping noise.
If the distal weakness is more severe, the foot will have to be lifted higher at the knee to
allow room for the inadequately dorsiflexed foot to swing through, producing a high
stepping gait .

2
Myopathic gait
During walking, alternate transfer of the body's weight through each leg requires careful
control of hip abduction by the gluteal muscles.
In proximal muscle weakness, usually caused by muscle disease, the hips are not properly
fixed by these muscles and trunk movements are exaggerated, producing a rolling or
waddling gait .
Ataxic gait
An ataxic gait can occur as the result of lesions in the cerebellum , vestibular apparatus or
peripheral nerves
Patients with lesions of the central parts of the cerebellum (the vermis) walk with a
characteristic broad-based gait, 'like a drunken sailor' (cerebellar function is particularly
sensitive to alcohol). Patients with acute vestibular disturbances walk in a similar broad-
based fashion, though the accompanying vertigo distinguishes them from those with
cerebellar lesions. Less severe degrees of cerebellar ataxia can be detected by asking the
patient to walk heel to toe; patients with vermis lesions are unable to do this .
Sensory ataxia
Impairment of joint position sense makes walking unreliable, especially in poor light. The
feet tend to be placed on the ground with greater emphasis, in an attempt to increase what
proprioceptive input is available. This results in a 'stamping' gait which is often combined
with foot drop when caused by a peripheral neuropathy, but it can occur in disorders of the
dorsal columns in the spinal cord
Apraxic gait
In an apraxic gait, there is normal power in the legs and no abnormal cerebellar signs or
proprioception loss, yet the patient cannot formulate the motor act of walking. This is a
higher cerebral dysfunction in which the feet appear stuck to the faloor and the patient
cannot walk, even though movement is normal on the examination couch.
Gait apraxia occurs in bilateral hemisphere disease such as normal pressure hydrocephalus
and diffuse frontal lobe disease .
3
Extrapyramidal gait
Patients with Parkinson disease and other extrapyramidal diseases have difficulty initiating
walking and difficulty controlling the pace of their gait . Patients may get stuck while trying
to start walking or when walking through doorways (freezing ) .Once started they may
shuffle and have problems controlling the speed of their walking and sometimes have
difficulty stopping . This produces the Festinant gait ; initial stuttering steps that quickly
increase in frequency while decreasing in length .
INVOLUNTARY MOVEMENTS
Rest tremor
This is pathognomonic of Parkinson disease .
It is characteristically pill rolling and usually presents asymmetrically.
Physiological tremor
This the most common type of action tremor and occurs at a frequency of 8-12 Hz.
It is common in normal subjects and exaggeration occurs in anxiety and in other situations .
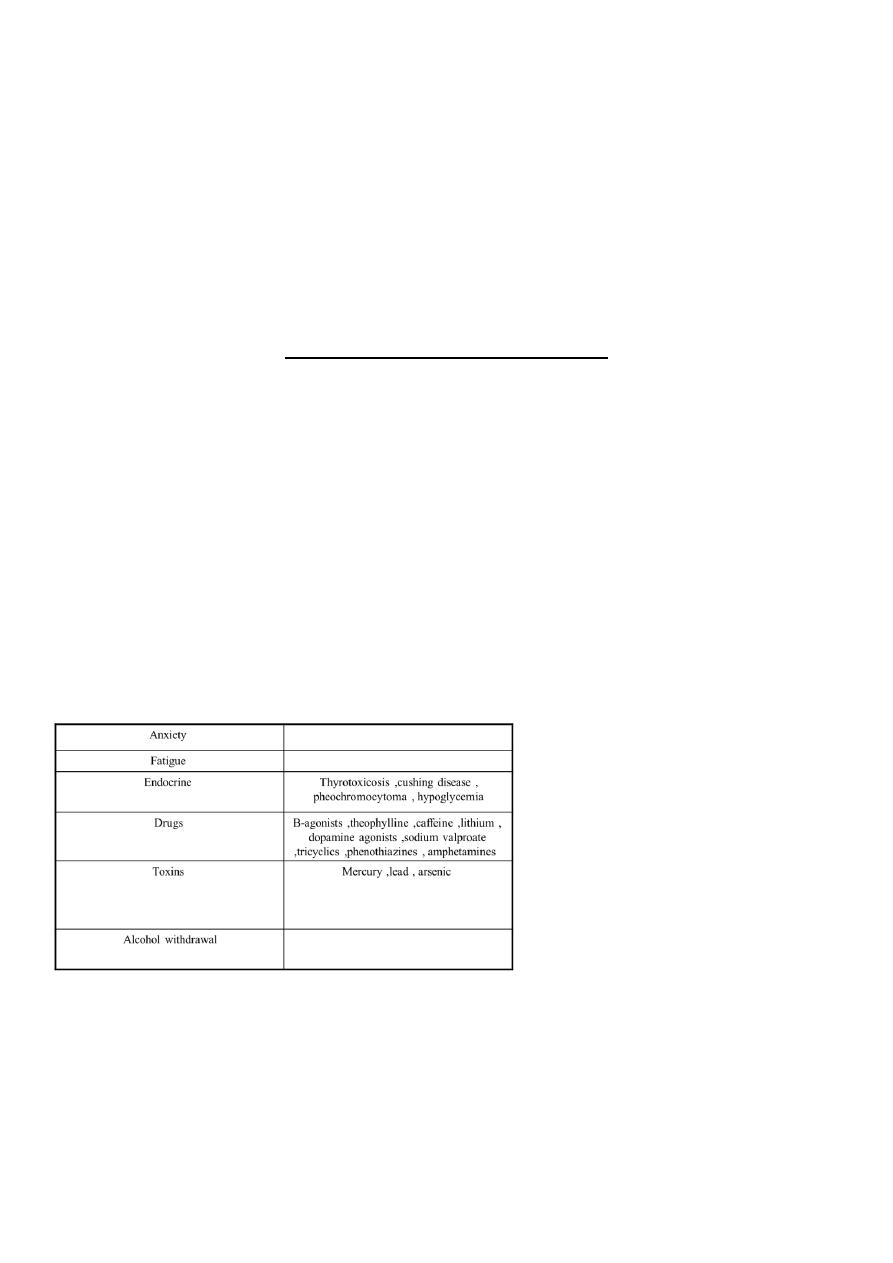
CAUSES OF EXAGGERATED PHYSIOLOGICAL TREMOR
Essential tremor
Essential tremor is distinct from a physiological tremor, although resembling it superficially.
It is slower and may become quite disabling. The condition is often inherited, and in some
families most obvious during certain specific actions such as writing or holding a glass ; here
there is an overlap with focal dystonias . Alcohol often suppresses it, sometimes to the

4
extent that the patient becomes dependent. Centrally acting β-adrenoceptor antagonists
(β-blockers) such as propranolol are often effective in treatment.
Intention tremor
This is characterised by oscillation at the end of a movement and typically occurs in
cerebellar disease. A more dramatic intention tremor occurs with lesions in the superior
cerebellar peduncle (the site of the cerebellar outflow to the red nucleus).Known as
peduncular rubral or Holmes tremor ; this is a violent large amplitude postural tremor that
worsens as a target is approached. It is common in advanced multiple sclerosis and may be
a source of considerable severity
Asterixis (flapping tremor)
Asterixis, the 'flapping' tremor seen in metabolic disturbances, is the result of intermittent
failure of the parietal mechanisms required to maintain a posture. Thus, when a patient is
asked to hold out the arms with the hands extended at the wrists, this posture is
periodically dropped, allowing the hands to drop transiently before the posture is taken up
again. Occasionally, unilateral asterixis can be seen in an acute parietal lesion, usually
vascular.
Causes of asterixis
Renal failure
Liver failure
Hypercapnia
Acute focal parietal or thalamic lesion
Chorea, athetosis, ballism
These are due to disturbance of balance of activity in the basal ganglia .
Chorea (the Greek for 'dance') : Jerky, small-amplitude, purposeless involuntary movements
. In the limbs they resemble fidgety movements, and in the face, grimaces; they suggest
disease in the caudate nucleus (as in Huntington's disease.
Hemiballismus: More dramatic ballistic flying violent movements of the limbs usually occur
unilaterally in vascular lesions of the subthalamic structures.
Athetosis : Slower writhing movements of the limbs . These are often combined with
chorea (and have a similar list of causes) and are then termed 'choreo-athetoid'
movements.
5
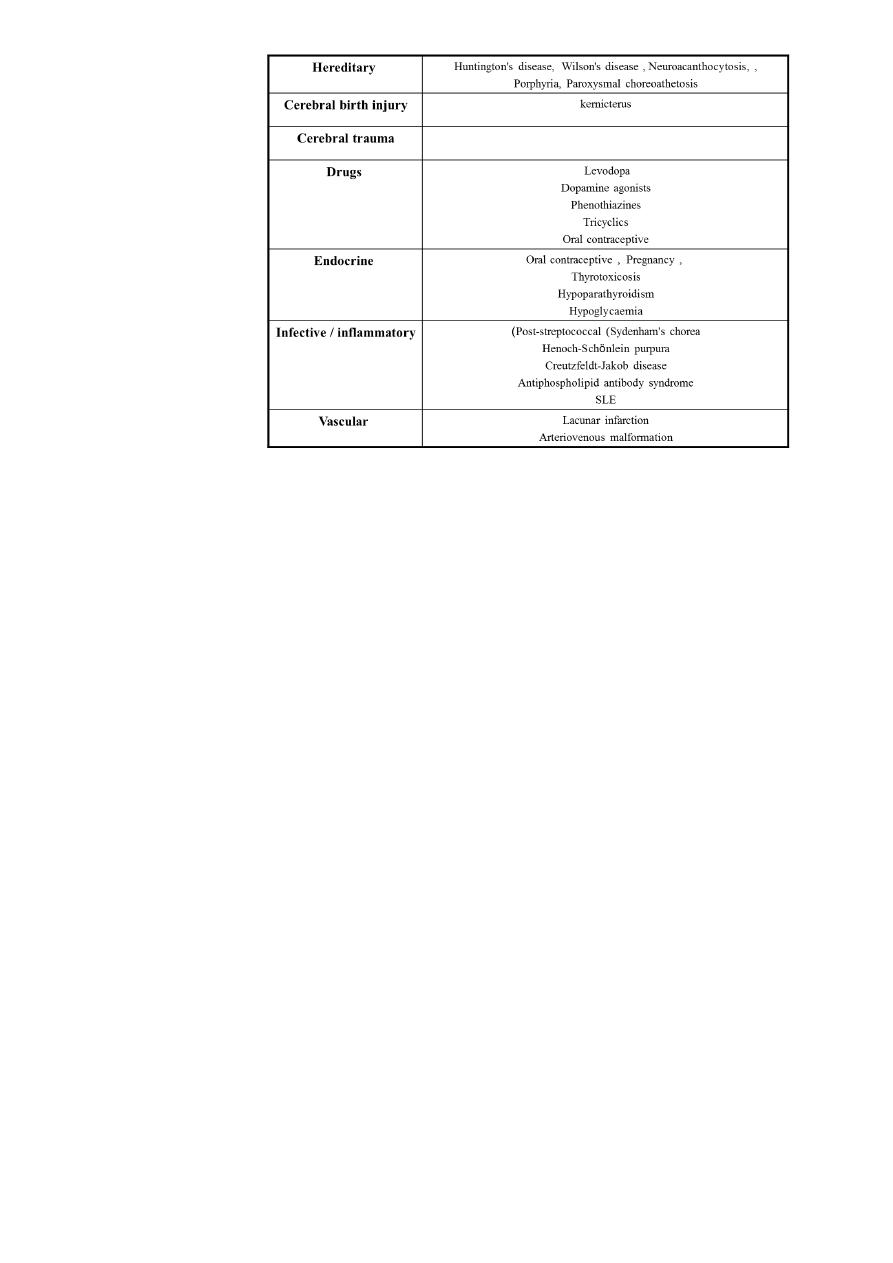
CAUSES OF CHOREA
Dystonia
This means sustained involuntary contraction that causes abnormal posture or movement.
It may be generalised in various diseases of the basal ganglia or may be focal or segmental,
as in spasmodic torticollis when the head involuntarily turns to one side. Other segmental
dystonias may cause abnormal disabling postures of a limb to be taken up during certain
specific actions, such as in writer's cramp or numerous other occupational 'cramps'. These
segmental dystonias can be treated by the administration of botulinum toxin to a few of
the responsible muscles.
Tics
Tics are repetitive semi-purposeful movements such as blinking or screwing up of the eyes.
They are distinguished from other involuntary movements by the ability of the patient to
suppress their occurrence, at least for a short time. An isolated tic may be no more than a
mild embarrassment, but may become frequent at certain times in childhood and then
disappear. The uncommon syndrome of Gilles de la Tourette consists of a tendency to
multiple tics and odd vocalisations, with obsessive behavioural abnormalities. The
pathogenic basis is not understood, but there may be some response to major
tranquillisers.
